Abstract
The podocin (NPHS2) gene encodes podocin protein, which has an important role in glomerular ultrafiltration and controlling slit membrane permeability. The detection of an NPHS2 mutation affects the treatment plan for children with nephritic syndrome (NS). The frequency and spectrum of podocin mutations in the Turkish population have remained largely unknown. The aim of this study was to screen for podocin mutations in Turkish patients with steroid-resistant NS (SRNS) and to compare it with other published series. There were 295 children with SRNS, originating from Turkey, included in this study. Forty-one patients (13.8%) had familial NS and 254 patients (86.2%) had sporadic NS. Mutation analysis was performed in all eight exons of the NPHS2 gene with the direct DNA sequencing method. There were 53 different pathogenetic NPHS2 mutations detected, including 37 novel mutations. The mutation detection rate was 24.7% for all patients, 29.2% for familial, and 24% for sporadic SRNS. The most common mutated exon was exon 5 (52 allele). The presence of mutations in exon 4 was found to increase the risk of end-stage renal disease (ESRD). Among patients with mutations, the rates of renal failure and/or ESRD (26%) were significantly higher than in those without mutations (12.6%). The mean time of progression to renal failure and ESRD in patients with mutations (1.8 ± 2.5 years) was significantly shorter than in patients without mutations (3.7 ± 4.0 years). Additionally, in patients with heterozygote mutations, fewer cases (13.6%) progressed to renal failure and/or ESRD than in with patients who had homozygote/compound heterozygote mutations (31.3%). In conclusion, podocin mutations are responsible for some of both familial and sporadic SRNS cases in Turkey. The mutations in this gene should be searched for in every child after presentation with the first episode of NS.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Nephrotic syndrome (NS) is an uncommon disorder in childhood and is characterized by edema, massive proteinuria, hypoalbuminemia, and hyperlipidemia. Clinically, NS has been divided into two categories on the basis of the response to steroid therapy: steroid-sensitive nephrotic syndrome (SSNS) and steroid-resistant nephrotic syndrome (SRNS). In SRNS, more than 75% of the patients exhibit the histology of focal segmental glomerulosclerosis (FSGS) in kidney biopsies and a considerable number of patients progress to end-stage renal disease (ESRD) [1–4]. Nephrin (NPHS1), α-actinin 4 (ACT4), and podocin (NPHS2) are proteins that play an important role in glomerular slit diaphragm homeostasis. The encoding genes, if mutated, are known to cause NS [5–8]. Podocin is a lipid raft-associated protein at the filtration slit, which is exclusively expressed in the glomerular podocytes at the foot processes [9–11]. The NPHS2 gene (OMIM number 604766) is located at chromosome 1q25–q31. It was first mapped by linkage analysis in families with autosomal recessive SRNS [3]. Then, Boute et al. [8] reported the first NPHS2 mutation in SRNS. Caridi et al. [12–16], Ruf et al. [17], and Weber et al. [18] got down to the details of the NPHS2 mutations, both in familial and sporadic cases of SRNS. Their studies are the most comprehensive so far.
The ethnic heterogeneity of this disease exposes the identification of NPHS2 mutations in patients from different countries. However, there is a limited number of studies on NPHS2 mutations from Turkey in the literature [12, 19, 20]. The aim of our study is to define NPHS2 mutations and genotype/phenotype correlations in Turkish children with SRNS and compare our results with those of other published series.
Material and methods
Definitions
Nephrotic syndrome was defined by edema, massive proteinuria (>40 mg/m2 per hour or a protein/creatinine ratio >2.0 mg/mg), hypoalbuminemia (<2.5 g/dl), and hyperlipidemia. Remission was defined as a urinary protein excretion below 4 mg/m2 per hour or a protein/creatinine ratio below 0.2 mg/mg for three consecutive days. Steroid resistance was accepted as no achievement of remission in spite of treatment with prednisolone, 2 mg/kg per day for 4 weeks. If steroid resistance was seen, patients were also treated with cyclosporine A (CsA) (3–5 mg/kg per day for least 6 months) and, thereafter, if required, with cyclophosphamide (CP) (2.5–3.0 mg/kg per day for 10–12 weeks). A diagnosis of FSGS was made using the criteria recently described by D’Agati et al. [21]. Renal failure was defined as a glomerular filtration rate (GFR) below 80 ml/min per 1.73 m2 body surface area, and ESRD was defined as a GFR below 10 ml/min per 1.73 m2 or the necessity for any renal replacement therapy.
Patients
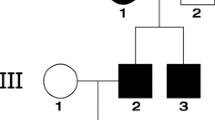
Two hundred and ninety-five children (170 boys and 125 girls) diagnosed with SRNS in 12 different pediatric nephrology departments in our country were included in the study. Geographical distribution of the centers was: seven in western Turkey, three in central Turkey, one in southern Turkey and one in the eastern part of Turkey. The medical records of each patient were reviewed for clinical features, laboratory values, and treatment regimens. In addition, patients with the NPHS2 mutation were grouped according to genetic analysis results: group A, familial NS; group B1, sporadic NS with two (homozygote or compound heterozygote) mutations; group B2, sporadic NS with a single (heterozygote) mutation. Furthermore, the main clinical features in patients with heterozygote mutations and compound heterozygote/homozygote mutations in NPHS2 were also compared. For genetic analysis, written informed consent was obtained from the parents of each patient, and the Ege University Medical School Ethics Committee approved the study.
Podocin mutation analysis
Genomic DNA from patients and healthy controls was extracted from peripheral blood leukocytes using QIAmp DNA Blood Mini Kits 50 (Qiagen, Hilden, Germany) according to the manufacturer’s instructions. Mutational analysis was performed by the direct sequencing of both strands of all eight exons of the NPHS2 gene. Primers for the eight exons of NPHS2 and sequencing were as described previously by Boute et al. [8] and Karle et al. [22]. Polymerase chain reaction (PCR) conditions were as follows: amplification was carried out on a GeneAmp PCR System 9700 (PE Applied Biosystems, Foster City, CA, USA) in a 50 μl reaction mixture in 0.2 ml thin-wall PCR strip tubes (Axygen Scientific, CA, USA) containing 1 μl genomic DNA solution, GeneAmp Gold Buffer (15 mmol/l Tris-HCl, pH 8.0, 50 mmol/l KCl; PE Applied Biosystems), 1.5 mmol MgCl2, 50 μmol/l each of the dGTP, dATP, dTTP and dCTP (Promega, Madison, WI, USA), 5 pmol each of forward and reverse primers, and 1.0 U AmpliTaq Gold polymerase (PE Applied Biosystems). The PCR products were applied to the electrophoretic analysis with a 2% agarose gel and visualized under UV illumination. The positive PCR products were purified by PCR purification columns (Genomics Millipore, Bedford, MA, USA). The purified PCR product was used for cycle sequencing procedure. Direct sequencing was carried out with ABI Prism BigDye Terminator Cycle Sequencing Ready Reaction Kits v. 3.2 (Applied Biosystems) in the automated sequencer ABI 3100.
Statistical analysis
All analyses were performed with SPSS for Windows version 11.0.0 (SPSS, USA). Differences in categorical variables between groups were tested with Fisher’s exact and chi-square tests. Differences in continuous variables between two groups were tested by the non-parametric Mann–Whitney U test. P < 0.05 was set as the level of statistical significance.
Results
Patients and mutations
The study population consisted of 295 SRNS patients. Their mean age at onset of proteinuria was 3.87 ± 3.08 years (median 2.72 years), and their median follow-up time was 3.89 years. Forty-one patients (13.8%) had familial NS and 254 patients (86.2%) had sporadic NS. Parental consanguinity was found in 49 patients (16.6%). Of the 295 SRNS patients, 73 (24.7%) showed NPHS2 mutation. The epidemiology, clinical data, treatment, and progression data of patients with or without NPHS2 mutation are presented in Table 1. Furthermore, the data of patients with heterozygote mutations and compound heterozygote/homozygote mutations in NPHS2 are presented in Table 2. NPHS2 mutations, clinical and treatment and disease progression of patients with mutations in NPHS2 are shown in Table 3. In familial NS, 12 (29.2%) of the 41 patients had an NPHS2 mutation. Eight patients had homozygote and four patients had double homozygote NPHS2 mutations (P20L and R168H in three patients, R3G and D267N in one patient). R168H, P20L and K289X were the most common mutations in familial NS patients. Among patients with sporadic NS, mutational screening gave positive findings in 61 (24%) patients. Homozygote, compound heterozygote, and heterozygote NPHS2 mutations were found in 29 (47.6%), 12 (19.6%) and 20 (32.8%) patients in the sporadic NS group, respectively. R229Q and P20L were the most common mutations in the sporadic NS patients. The mutation frequency was not different between the familial and sporadic NS groups (P > 0.05). We found 53 different mutations and functional variants identified from the NPHS2 gene, as shown in Table 4. The most common mutated exons were exon 5 (52 allele), exon 1 (28 allele), and exon 3 (17 allele). We did not find any mutation in exon 6. G34G and A318A were the most common polymorphisms in patients with mutations. Among 53 different NPHS2 mutations, 37 were novel mutations (Table 4, bold characters in Table 3). None of the novel mutations was found in at least 50 control chromosomes. Patients with novel A213T, 503delG, H228D, and V218G mutations progressed to ESRD. The age at onset of proteinuria in patients with novel M115T and 377insT mutations was under 1 year. All NPHS2 mutations are also presented in Table 4. The overall clinical features of our series, including age at onset, progression to ESRD and histological presentation, were compared with those of sporadic/familial SRNS reported in previous studies of patients of Central European, North African and Middle Eastern origins (Table 5).
Renal histology and NPHS2 mutations
A kidney biopsy was performed in 202 (68.4%) patients. Among patients with homozygote/compound heterozygote mutations, the histological findings were as follows: FSGS in 36 (70.5%), diffuse mesangial proliferation (DMP) in four, minimal change nephrotic syndrome (MCNS) in four, membranoproliferative glomerulonephritis (MPGN) in three, and, IgM deposition with mesangial proliferation (IgMN) in three patients (the diagnosis failed in one patient due to insufficient biopsy material). Among patients with heterozygote mutations, the histological findings were as follows: FSGS in 16 (72.7%), MCNS in four, IgMN in one, and MPGN in one. Among patients without mutation, the most frequent histological findings were: FSGS in 45 (34.8%), MCNS in 27 (20.9%), IgMN in 16 (12.4%), and DMP in nine (6.9%) (no biopsy was performed in 93 patients). The frequency of FSGS in patients with mutations was significantly higher than in those without mutations (P < 0.05) (Table 1).
NPHS2 mutations and disease progression
The mean age at onset of NS was significantly higher in patients without mutations than in patients with mutations (P < 0.05). The frequency of familial NS, consanguinity, hematuria, and hypertension in patients with mutations was significantly higher than in patients without mutations (P < 0.05) (Table 1, 2). Among patients with mutations, the rate of renal failure and/or ESRD (19/73, 26%) was significantly higher than among patients without mutations (28/222, 12.6%), (P < 0.05). The mean time of progression to renal failure and ESRD in patients with mutations (1.8 ± 2.5 years) was significantly shorter than in patients without mutations (3.7 ± 4.0 years) (P < 0.05). Additionally, in patients with heterozygote mutations, fewer (13.6%) progressed to renal failure and/or ESRD than did those with homozygote/compound heterozygote mutations (31.3%) (Table 2, P < 0.05). The mean time of progression to ESRD in patients with compound heterozygote/homozygote (5.1 ± 2.7 years) was significantly shorter than in patients with heterozygote mutations (8.3 ± 3.4 years) (P < 0.05) (Table 2).
P118L, R138X, R168H, R138Q, IVS7+5G>A, A212T, insT460–467, P20L, 503delG, H228D, S211A, and V218G mutations are associated with progression to ESRD. Dealing with mutations in exon 4 of the NPHS2 gene, we observed ESRD in five of nine patients (66.6%). The presence of mutations in exon 4, regardless of other risk factors such as age at onset and duration of disease, was found to increase the risk of renal failure and ESRD by 4.3 times and 4.4 times, respectively (95% CI 1.2–15.2 and 1.2–15.8). The mutations in other exons of NPHS2 did not correlate with disease progression. Additionally, the clinical courses regarding the age at onset and the progression of illness in the Turkish patients were consistent with those reported previously for SRNS patients (Table 5).
Discussion
This study is the largest evaluation of NPHS2 gene mutations in SRNS patients in Turkey. Based on our results, the incidence of podocin mutations in familial SRNS cases in our country (29.2%) was found to be lower than in European and American children (∼40%) but higher than that found in Japanese and Korean children (0%) [14, 17, 18, 23]. According to our results, the incidence of podocin mutations in sporadic SRNS cases in Turkey (24%) was similar to that among European and American children (10–30%) but higher than that found in Chinese (4%), Japanese, and Korean children (0%), [14, 16–18, 23, 24]. Furthermore, Caridi et al. [16] have demonstrated a mutation detection rate of 45–55% in families with recessive traits and 8–20% in sporadic NS. Our results are important because the frequency and spectrum of podocin mutations in Turkey are largely unknown.
Clinical developments have suggested that podocin plays an essential role both in the functional component of the slit diaphragm and in the maintenance of the glomerular permeability barrier [16, 25, 26]. Overall clinical features of our series, including age at onset, progression to ESRD, and histological presentation, were compatible with those of sporadic/familial SRNS reported in previous studies with patients of Central European, North African, Asian, and Middle Eastern origins (Table 5). Different NPHS2 mutations have been found in Italian, French, German and, Israeli-Arab children [13, 14, 17, 18, 22, 27]. However, it has been reported that there is a lack of contribution of podocin mutations in Israeli-Jewish, Chinese, and Japanese children [23, 24, 28]. Our results are in sharp contrast with those of Asian studies, suggesting that genetic factors of FSGS differ among Asian patients and that yet unidentified genes are involved in the pathogenesis of SRNS in Asian patients [23, 24, 28].
Most of the studies so far published have referred to European populations and have reported that R138Q was most frequently found in Germany and France [17, 18], while the P20L variant was observed mainly in Italy [14] and Turkey [16]. Essentially, P20L has also been reported frequently in Europe [8, 12, 13, 15]. Also, the R168H mutation has been reported in Israeli-Arab children [27]. In our study, R168H and P20L were the most common mutations in familial NS patients.
The age at onset of proteinuria is rather variable in different reports [12, 16, 17, 18]. Weber et al. [18] reported that R138Q could be associated with early onset as well as V180M, R229Q and R238S could be associated with late onset NS. In our study, P20L and R168H were found to be associated with early onset. Seven of 14 cases with an age at onset within the first year of life showed P20L and R168H mutations. Also, R138Q mutation was determined only in four patients with sporadic NS. In three of them, the first clinical symptoms had been observed before the age of 3 years, and one progressed to ESRD. The fourth patient had compound heterozygote mutations (R138Q and R229Q), the first occurring at 9.5 years.
It has been pointed out that sporadic NS patients with a NPHS2 mutation progressed to ESRD after 73 months from the onset of proteinuria (range 6–155 months), while familial cases reached ESRD after a follow-up of 76 months (range 18–162 months) [14, 16, 17]. Similarly, in our study, patients with a mutation progressed to ESRD after 70 months from the onset of proteinuria (range 32–130 months). In addition, the presence of a mutation in exon 4 indicated an increased risk of renal failure or ESRD in our NPHS2 population.
The diagnosis of diseases related to podocin mutations is difficult because of the heterogeneous clinical and pathological spectrum; therefore, a molecular diagnosis based on sequencing is required. In patients with the sporadic form of SRNS, identification of NPHS2 mutations is of importance, not only for therapeutic considerations but also for genetic counseling. However, there is no clear genotype/phenotype correlation in children with NPHS2 mutations [15, 17, 24–28]. The rate of familial NS, hematuria and hypertension, the mean age at diagnosis, the presence of consanguinity, and the FSGS histology in patients with mutations were found to be significantly higher than in patients without mutations (P < 0.05). Therefore, we propose that mutational analysis of NPHS2 should be performed in children immediately after they have presented with their first episode of NS. This information may have important implications for the clinical and therapeutic approach to patients with a nephrotic syndrome that is unresponsive to steroids, because, theoretically, ineffective and potentially harmful immunosuppression could be avoided in carriers of the mutations. Also, Caridi et al. [13], Ruf et al. [17] and Frishberg et al. [27] have suggested that children with a first episode of NS should be tested for a podocin mutation before therapy, to avoid an unnecessary steroid course in those with NPHS2 mutations. Therefore, further studies with more patients are required to search the genotype/phenotype relationships for homozygote or compound heterozygote mutations in NPHS2 and responses to other forms of immune suppressive treatments, such as CsA, tacrolimus, cyclophosphamide, methylprednisolone pulse therapy, or mycophenolate mofetil. For the significance of single heterozygote sequence variants, functional studies must be performed.
A small number of studies have described polymorphism in untranslated regions, including intronic positions. The significance of certain mutations is yet unknown, especially in patients affected by compound heterozygote mutations with the R229Q variant [18, 29]. In this study, the R229Q mutation was determined in one patient with familial NS and in 13 patients with sporadic NS. Five of the 13 patients with sporadic NS had a homozygote R229Q mutation, and one of them progressed to ESRD. Other reported homozygote polymorphisms are A242V, A318A, S96S, L346L, A44E, G34G, and A297A [13, 18, 22, 26, 28–36]. In our study, we found the following variants: G34G in 263 patients, A318A in 47 patients, S96S in three patients, L314L in one patient, and Y131Y in one patient. Further studies are necessary to determine the allele and genotype frequencies across different populations.
Our study has contributed to the descriptions of novel podocin mutations. Thirty-seven new mutations (Table 4 and bold characters in Table 3) have been described in our study. Age at onset of proteinuria in patients with M115T and 377insT novel mutations was under 1 year. We think that this syndrome will be more understandable with the increase in identification of other causative genes in different populations.
In conclusion, podocin mutations are responsible for some of both familial and sporadic SRNS cases in Turkey. The mutations in this gene should be searched for in every child after presentation with the first episode of NS, thus avoiding an unnecessary second trial of standard steroid therapy with SRNS. Further genetic studies in families with NPHS2-negative SRNS are warranted for the identification of other causative genes.
References
Arbeitsgemeinschaft fur Pädiatrische Nephrologie (1988) Short versus standard prednisone therapy for initial treatment of idiopathic nephrotic syndrome in children. Lancet 1:380–383
International Study of Kidney Disease in Children (1981) Primary nephrotic syndrome in children: clinical significance of histopathologic variants of minimal change and of diffuse mesangial hypercellularity. A report of the International Study of Kidney Disease in Children. Kidney Int 20:765–771
Fuchshuber A, Jean G, Gribouval O, Gubler MC, Broyer M, Beckmann JS, Niaudet P, Antignac C (1995) Mapping a gene (SRN1) to chromosome 1q25-q31 in idiopathic nephrotic syndrome confirms a distinct entity of autosomal recessive nephrosis. Hum Mol Genet 4:2155–2158
Fuchshuber A, Gribouval O, Ronner V, Kroiss S, Karle S, Brandis M, Hildebrandt F (2001) Clinical and genetic evaluation of familial steroid-responsive nephrotic syndrome in childhood. J Am Soc Nephrol 12:374–378
Kestila M, Lenkkeri U, Mannikko M, Lamerdin J, McCready P, Putaala H, Ruotsalainen V, Morita T, Nissinen M, Herva R, Kashtan CE, Peltonen L, Holmberg C, Olsen A, Tryggvason K (1998) Positionally cloned gene for a novel glomerular protein—nephrin—is mutated in congenital nephrotic syndrome. Mol Cell 4:575–582
Winn MP, Conlon PJ, Lynn KL, Howell DN, Slotterbeck BD, Smith AH, Graham FL, Bembe M, Quarles LD, Pericak-Vance MA, Vance JM (1999) Linkage of a gene causing familial focal segmental glomerulosclerosis to chromosome 11 and further evidence of genetic heterogeneity. Genomics 58:113–120
Kaplan JM, Kim SH, North KN, Rennke H, Correia LA, Tong HQ, Mathis BJ, Rodriguez-Perez JC, Allen PG, Beggs AH, Pollak MR (2000) Mutations in ACTN4, encoding α-actinin-4, cause familial focal segmental glomerulosclerosis. Nat Genet 24:251–256
Boute N, Gribouval O, Roselli S, Benessy F, Lee H, Fuchshuber A, Dahan K, Gubler MC, Niaudet P, Antignac C (2000) NPHS2, encoding the glomerular protein podocin, is mutated in autosomal recessive steroid-resistant nephrotic syndrome. Nat Genet 24:349–354
Roselli S, Gribouval O, Boute N, Sich M, Benessy F, Attie T, Gubler MC, Antignac C (2001) Podocin localizes in the kidney to the slit diaphragm area. Am J Pathol 160:131–139
Huber TB, Simons M, Hartleben B, Sernetz L, Schmidts M, Gundlech E, Saleem MA, Walz G, Benzing T (2003) Molecular basis of the functional podocin-nephrin complex: mutations in the NPHS2 gene disrupt nephrin targeting to the lipid raft microdomains. Hum Mol Genet 12:3397–3405
Schwarz K, Simons M, Reiser J, Saleem MA, Faul C, Kriz W, Shaw AS, Holzman LB, Mundel P (2001) Podocin, a raft-associated component of the glomerular slit diaphragm, interacts with CD2AP and nephrin. J Clin Invest 108:1621–1629
Caridi G, Berdeli A, Dagnino M, DiLuca M, Mir S, Cura A, Ravazzolo R, Ghiggeri GM (2004) Infantile steroid-resistant nephrotic syndrome associated with double homozygote mutations of podocin. Am J Kidney Dis 43:727–732
Caridi G, Bertelli R, Carrea A, Di Duca M, Catarsi P, Artero M, Carraro M, Zennaro C, Candiano G, Musante L, Seri M, Ginevri F, Perfumo F, Ghiggeri GM (2001) Prevalence, genetics, and clinical features of patients carrying podocin mutations in steroid-resistant nonfamilial focal segmental glomerulosclerosis. J Am Soc Nephrol 12:2742–2746
Caridi G, Bertelli R, Di Duca M, Dagnino M, Emma F, Onetti Muda A, Scolari F, Miglietti N, Mazzucco G, Murer L, Carrea A, Massella L, Rizzoni G, Perfumo F, Ghiggeri GM (2003) Broadening the spectrum of diseases related to podocin mutations. J Am Soc Nephrol 14:1278–1286
Caridi G, Bertelli R, Scolari F, Sanna-Cherchi S, Di Duca M, Ghiggeri GM (2003) Podocin mutations in sporadic focal-segmental glomerulosclerosis occurring in adulthood. Kidney Int 64:365
Caridi G, Perfumo F, Ghiggeri GM (2005) NPHS2 (podocin) mutations in nephrotic syndrome. Clinical spectrum and fine mechanisms. Pediatr Res 57:54–61
Ruf RG, Lichtenberger A, Karle SM, Haas JP, Anacleto FE, Schultheiss M, Zalewski I, Imm A, Ruf EM, Mucha B, Bagga A, Neuhaus T, Fuchshuber A, Bakkaloglu A, Hildebrant F (2004) Patients with mutations in NPHS2 (podocin) do not respond to standard steroid treatment of nephrotic syndrome. J Am Soc Nephrol 15:722–732
Weber S, Gribouval O, Esquivel EL, Moriniere V, Tete MJ, Legendre C, Niaudet P, Antignac C (2004) NPHS2 mutation analysis shows genetic heterogeneity of steroid-resistant nephrotic syndrome and low post-transplant recurrence. Kidney Int 66:571–579
Ozer EA, Aksu N, Erdogan H, Yavascan O, Kara O, Gribouval O, Gubler MC, Antignac C (2004) A novel NPHS2 gene mutation in Turkish children with familial steroid-resistant nephrotic syndrome. Nephrology 9:310–312
Ozcakar ZB, Cengiz FB, Cakar N, Uncu N, Kara N, Acar B, Yuksel S, Ekim M, Tekin M, Yalcinkaya F (2006) Analysis of NPHS2 mutations in Turkish steroid-resistant nephrotic syndrome patients. Pediatr Nephrol 21:1093–1096
D’Agati VD, Fogo AB, Bruijn JA, Jennette JC (2004) Pathologic classification of focal segmental glomerulosclerosis: a working proposal. Am J Kidney Dis 43:368–382
Karle S, Uetz B, Ronner V, Glaeser L, Hildebrandt F, Fuchshuber A, Members of the APN Study Group (2002) Novel mutations in NPHS2 are detected in familial and sporadic steroid-resistant nephrotic syndrome. J Am Soc Nephrol 13:388–393
Kitamura A, Tsukaguchi H, Iijima K, Araki J, Hattori M, Ikeda M, Honda M, Nozu K, Nakazato H, Yoshikawa N, Kagami S, Muramatsu M, Choi Y, Cheong HI, Doi T (2006) Genetics and clinical features of 15 Asian families with steroid-resistant nephrotic syndrome. Nephrol Dial Transplant 21:3133–3138
Yu Z, Ding J, Huang J, Yao Y, Xiao H, Zhang J, Liu J, Yang J (2005) Mutations in NPHS2 in sporadic steroid-resistant nephrotic syndrome in Chinese children. Nephrol Dial Transplant 20:902–908
Lenkkeri U, Mannikko M, McCready P, Lamerdin J, Gribouval O, Niaudet PM, Antignac CK, Kashtan CE, Homberg C, Olsen A, Kestila M, Tryggvason K (1999) Structure of the gene for congenital nephrotic syndrome of the Finnish type (NPHS1) and characterization of mutations. Am J Hum Genet 64:51–61
Dusel JA, Burdon KP, Hicks PJ, Hawkins GA, Bowden DW, Freedman BI (2005) Identification of podocin (NPHS2) gene mutations in African Americans with nondiabetic end-stage renal disease. Kidney Int 68:256–262
Frishberg Y, Rinat C, Megged O, Shapira E, Feinstein S, Raas-Rothschild A (2002) Mutations in NPHS2 encoding podocin are a prevalent cause of steroid-resistant nephrotic syndrome among Israeli-Arab children. J Am Soc Nephrol 3:400–405
Maruyama K, Iijima K, Ikeda M, Kitamura A, Tsukaguchi H, Yoshiya K, Hoshii S, Wada N, Uemura O, Satomura K, Honda M, Yoshikawa N (2003) NPHS2 mutations in sporadic steroid-resistant nephrotic syndrome in Japanese children. Pediatr Nephrol 18:412–416
Tsukaguchi H, Sudhakar A, Le TC, Nguyen T, Yao J, Schwimmer JA, Schachter AD, Poch E, Abreu PF, Appel GB, Pereira AB, Kalluri R, Pollak MR (2002) NPHS2 mutations in late-onset focal segmental glomerulosclerosis: R229Q is a common disease associated allele. J Clin Invest 110:1659–1666
Franceschini N, North KE, Kopp JB, McKenzie L, Winkler C (2006) NPHS2 gene, nephrotic syndrome and focal segmental glomerulosclerosis: a HuGE review. Genet Med 8:63–75
Wu MC, Wu JY, Lee CC, Tsai CH, Tsai FJ (2001) A novel polymorphism (c288C>T) of the NPHS2 gene identified in a Taiwan Chinese family. Hum Mutat 17:81–82
Schultheiss M, Ruf RG, Mucha BE, Wiggins R, Fuchshuber A, Lichtenberger A, Hildebrandt F (2004) No evidence for genotype/phenotype correlation in NPHS1 and NPHS2 mutations. Pediatr Nephrol 19:1340–1348
Komatsuda A, Wakui H, Maki N, Kigawa A, Goto H, Ohtani H, Hamai K, Oyama Y, Makoto H, Sawada K, Imai H (2003) Analysis of mutations in alpha-actinin 4 and podocin genes of patients with chronic renal failure due to sporadic focal segmental glomerulosclerosis. Ren Fail 25:87–93
Roselli S, Moutkine I, Gribouval O, Benmerah A, Antignac C (2004) Plasma membrane targeting of podocin through the classical exocytic pathway: effect of NPHS2 mutations. Traffic 5:1–8
Niaudet P (2004) Podocin and nephrotic syndrome: implications for the clinician. J Am Soc Nephrol 15:832–834
Koziell A, Grech V, Hussain S, Lee G, Lenkkeri U, Tryggvason K, Scambler P (2002) Genotype/phenotype correlations of NPHS1 and NPHS2 mutations in nephrotic syndrome advocate a functional interrelationship in glomerular filtration. Hum Mol Genet 11:379–388
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Berdeli, A., Mir, S., Yavascan, O. et al. NPHS2 (podicin) mutations in Turkish children with idiopathic nephrotic syndrome. Pediatr Nephrol 22, 2031–2040 (2007). https://doi.org/10.1007/s00467-007-0595-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-007-0595-y