Abstract
Mutations in the NPHS2 gene are a frequent cause of familial and sporadic steroid-resistant nephrotic syndrome (SRNS). Inter-ethnic differences have also been suggested to affect the incidence of these mutations. The frequency and spectrum of podocin mutations in the Turkish population have remained largely unknown. As such, the aim of this study was to screen for podocin mutations in Turkish patients with SRNS. Thirty two patients from 30 unrelated families with SRNS were examined. There were seven familial cases from five different families and 25 sporadic cases. PCR-single-strand conformation polymorphism (SSCP) analysis of the NPHS2 gene was followed by direct sequencing. Five different NPHS2 mutations were detected in four of the 30 (13.3%) families studied; five familial patients from three unrelated families (60%) and one sporadic case (4%) were found to carry podocin mutations. The detected mutations included homozygous c. 419delG, compound heterozygous p. [Arg238Ser] + [Pro118Leu], homozygous p. [Pro20Leu; Arg168His] and heterozygous p. Pro20Leu. Two siblings with compound heterozygous mutations had been reported previously by our group. Podocin mutations were found to be responsible for some of the SRNS cases in Turkey, especially when there was more than one affected person in the family. Our results also suggest the presence of a wide range of phenotypic variability between individuals with the same genotype.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic nephrotic syndrome (NS) is the most frequent childhood glomerular disease. It is generally classified into steroid-sensitive and steroid-resistant forms, depending upon the patient’s response to steroid therapy. Most of the children with NS respond to corticosteroid therapy, whereas 10% of them fail to respond to this treatment [1]. During this past decade, genetic studies in children with familial NS have identified mutations in genes that encode important podocyte proteins [2].
Podocin is an integral membrane protein and is encoded by NPHS2. This gene has been mapped to 1q25–31 and is exclusively expressed in glomerular podocytes. NPHS2 mutations are responsible for autosomal recessive familial steroid-resistant focal segmental glomerulosclerosis (FSGS), which is characterized by early childhood onset, rapid progression to chronic renal failure and the absence of recurrence following renal transplantation [3]. NPHS2 mutations have been reported in approximately 40% of familial steroid-resistant nephrotic syndrome (SRNS) patients and have also been found in 10–30% of sporadic SRNS cases [4–6]. The clinical spectrum of NPHS2 mutations has been broadened as it has been designated that mutations might be responsible for NS occurring at birth, in childhood or in adulthood. Inter-ethnic differences have also been suggested to play a role in the incidence of these mutations. For example, mutations have been found in Italian, French, German and Israeli Arab children but not in Israeli Jewish and Japanese children [4, 5, 7–9]. The frequency and spectrum of podocin mutations in Turkey have remained largely unknown although a few case reports have been published [10, 11]. The aim of this study was to screen for podocin mutations in Turkish patients with SRNS.
Materials and methods
Patients
Inclusion criteria were ethnic origin (Turkish patients), age at onset of disease (younger than 16 years), patients with NS, unresponsiveness to steroid therapy and absence of clinical and laboratory findings of a systemic disease.
The definitions and criteria for NS and steroid resistance were those used by the International Study of Kidney Disease in Children [12]. Nephrotic syndrome was defined as massive proteinuria (>40 mg/m2 per hour), hypoalbuminemia (<2.5 g/dl) and edema. Remission of NS was defined as the disappearance of proteinuria (<4 mg/m2 per hour); steroid resistance was defined as the lack of response to daily orally administered prednisone treatment at 2 mg/kg per day for 1 month.
Medical records of each patient were reviewed for the clinical features, laboratory values and treatment regimens. Written informed consent was obtained from the parents of each patient, and the study was approved by the Ankara University Medical School Ethics Committee.
Mutation analysis
Mutation analysis was performed in our center except for two patients which had been previously studied in France [11].
Genomic DNA was extracted from peripheral blood using a standard phenol chloroform method. The individual exons of the NPHS2 gene were PCR-amplified using specific primers based on published information regarding intron-exon boundaries [3]. The sequences of the forward and reverse primers, PCR conditions and the sizes of PCR products are given in Table 1.
The PCR reaction was performed in a total volume of 25 μl containing 100 ng genomic DNA, 20 pmol of each primer, 2 mM deoxynucleotide triphosphates and 1 U thermostable DNA polymerase. Three different touchdown programmes were used. For the first touchdown PCR (TD1), the annealing temperature was lowered 2°C every two cycles from 64 to 54°C; the denaturation and extension temperatures stayed constant at 94 and 72°C, respectively. For the second touchdown PCR (TD2), the annealing temperature was lowered 1°C every cycle from 65 to 60°C for five cycles, followed by the annealing temperature of 60°C for five cycles; the denaturation and extension temperatures stayed at 94 and 72°C, respectively. For the last touchdown PCR (TD3), the annealing temperature was lowered 0.5°C every cycle from 70 to 60°C for 20 cycles, followed by the annealing time being increased 1 s every cycle for 20 cycles; the denaturation temperature stayed constant at 94°C.
The coding exons were screened using PCR-single-strand conformation polymorphism (SSCP) protocols. The PCR products were denatured at 95°C, loaded onto 7% denaturing polyacrylamide gels, run overnight at +4°C in a vertical gel electrophoresis system (Protean II Xi Cell; BioRad, USA) and visualized with silver staining. Samples showing band changes were directly sequenced with an automated sequencer (Beckman Coulter, CEQ 2000 XL, USA) after cycle sequencing reactions (DTCS kit; Beckman Coulter) and analysed using Beckman Coulter software.
Results
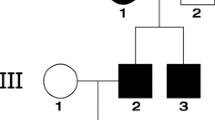
The study comprised 32 pediatric patients (15 males, 17 females) from 30 unrelated families with SRNS who have been followed in the Pediatric Nephrology Clinics of Ankara University Medical School and the Ministry of Health Ankara Dışkapı Children’s Hospital. The mean age at onset of disease was 54.8±48.1 months (range: 2–192 months). There were seven familial cases from five different families and 25 sporadic cases. Consanguinity was recorded in 14 patients (43.8%). Renal biopsies showed FSGS in 21 (65.4%) patients, diffuse mesangial proliferation (DMP) in seven (22%) patients, minimal change nephrotic syndrome (MCNS) in two (6.3%) patients and nonspecific pathology in two (6.3%) patients. All patients were treated with standard steroid therapy and showed steroid resistance. Twenty one (70%) of the patients were also treated with cyclophosphamide and/or other immunosupressive agents [mycophenolate mofetile (MMF), cyclosporin A] and did not respond to these drugs. At the time of analysis three (9.4%) patients had end stage renal disease, three (9.4%) had chronic renal insufficiency and one (3.1%) had undergone kidney transplantation.
NPHS2 mutations were detected in four of the 30 (13.3%) families studied; five familial patients from three unrelated families and one sporadic case were found to carry these mutations. The clinical characteristics of the patients with NPHS2 mutations and identified mutations are presented in Table 2.
Discussion
This study is the first systematic evaluation of NPHS2 gene mutations in familial and sporadic SRNS patients in Turkey. We have found five different NPHS2 mutations in four of 30 unrelated families. Three of the five families (60%) with familial SRNS and one of the 25 (4%) with sporadic SRNS were found to carry NPHS2 mutations. Based on our results, the incidence of podocin mutations in sporadic SRNS cases in Turkey is lower than that among European and American children (10–30%) but similar to that found in Chinese children (4%) [4, 6, 7, 13]. The low mutation rates in Turkey can be attributed to the small number of patients tested. However, ethnic factors, various other known or unknown genes and other pathogenetic mechanisms of NS can all affect podocin mutation rates in different parts of the world.
The only recurrent NPHS2 mutation in Turkey was p.Pro20Leu. Interestingly, we found this mutation homozygous in association with homozygous p.Arg168His in one familial case. This complex allele in the homozygous state has been previously described in three patients from two unrelated families from Turkey [10]. These three patients had common clinical features of a very early onset of NS (within the first 6 months of life) and the same histopathological background of FSGS. Our patient, however, presented with NS at 5.5 years of age and had a pathological diagnosis of DMP. Although Caridi et al. [10] proposed that this complex haplotype results in a more serious phenotype, the identification of the same complex mutation in our patient suggests the presence of a wide range of phenotypic variability between individuals with the same genotype.
Another patient in whom we identified the p.Pro20Leu mutation was a sporadic case. Moreover, p. Pro20Leu was in heterozygous state. Boute et al. [3] detected a homozygous p. Pro20Leu mutation in one of the families in 2000 when they first identified this gene. Caridi et al. [14] detected heterozygous p. Pro20Leu mutations in five children with more favorable outcomes. Ruf et al. [6] considered this mutation to be a polymorphism because they found homozygous p. Pro20Leu mutations in two healthy control patients, while Weber et al. [7] considered p. Pro20Leu mutation to be more than a polymorphism, stating also that heterozygous NPHS2 mutations play a role in later onset patients with a mild clinical course. In general, the disease-causing role of heterozygous mutations in NPHS2 has not yet been well documented. Some authors propose that while assuming a causative role of heterozygous sequence variants, a second mutation may have been missed or may be located in the promoter region or in an intron [6]. The second alternative would be the involvement of other genes in the pathogenesis of NS via the mechanism of ‘digenic inheritance’ [15]. The early onset of disease (at 12 months of age) in our patient might have been due to the presence of the two unknown aforementioned factors. It should be noted here, however, that the screening strategy we used may have missed some sequence changes in the coding regions as well.
Two siblings in our study were found to carry the homozygous c. 419delG mutation which results in a frameshift in the protein; these siblings had disease onset at 2 months and 2 years of age, respectively. Two other siblings with p. [Arg 238 Ser] + [Pro118 Leu] mutations had disease onset at later ages. There is an growing understanding of a genotype-phenotype correlation in patients with NPHS2 mutations. Weber et al. [7] detected that familial cases with pathogenic mutations in the homozygous or compound heterozygous states, patients with frameshift or nonsense mutations in the homozygous or compound heterozygous states and patients with homozygous p. Arg138Glu had an early mean age of disease onset. They also recognized that some missense mutations were associated with a milder clinical course, and p. Val180Met and p. Arg238Ser variants were identified in patients with a later onset. Our results and those of Weber et al. [7] are similar in this regard, but these associations were not valid to all patients due to the presence of diverse phenotypic variability.
In conclusion, podocin mutations are responsible for some of the SRNS cases in Turkey, especially when there is more than one affected person in the family. Due to the important role of NPHS2 analysis in the treatment and follow-up of SRNS patients, mutations in this gene should be searched for in each patient with SRNS in Turkey. Further genetic studies in families with NPHS2-negative SRNS are warranted for the identification of other causative genes.
References
Niaudet P (2004) Steroid-resistant idiopathic nephrotic syndrome in children. In: Avner ED, Harmon WE, Niaudet P (eds) Pediatric Nephrology. Lippincott Williams & Wilkins, Philadelphia, pp 557–573
Pollak MR (2003) The genetic basis of FSGS and steroid resistant nephrosis. Semin Nephrol 23:141–146
Boute N, Gribouval O, Roselli S, Benessy F, Lee H, Fuchshuber A, Dahan K, Gubler MC, Niaudet P, Antignac C (2000) NPHS2, encoding the glomerular protein podocin, is mutated in autosomal recessive steroid-resistant nephrotic syndrome. Nat Genet 24:349–354
Karle SM, Uetz B, Ronner V, Glaeser L, Hildebrandt F, Fuchshuber A (2002) Novel mutations in NPHS2 detected in both familial and sporadic steroid-resistant nephrotic syndrome. J Am Soc Nephrol 13:388–393
Caridi G, Bertelli R, Carrea A, Di Duca M, Catarsi P, Artero M, Carraro M, Zennaro C, Candiano G, Musante L, Seri M, Ginevri F, Perfumo F, Ghiggeri GM (2001) Prevalence, genetics and clinical features of patients carrying podocin mutations in steroid resistant nonfamilial focal segmental glomerulosclerosis. J Am Soc Nephrol 12:2742–2746
Ruf RG, Lichtenberger A, Karle SM, Haas JP, Anacleto FE, Schultheiss M, Zalewski I, Imm A, Ruf EM, Mucha B, Bagga A, Neuhaus T, Fuchshuber A, Bakkaloğlu A, Hildebrandt F; Arbeitsgemeinschaft für Pädiatrische Nephrologie Study Group (2004) Patients with mutations in NPHS2 (Podocin) do not respond to standard steroid treatment of nephrotic syndrome. J Am Soc Nephrol 15:722–732
Weber S, Gribouval O, Esquivel EL, Moriniere V, Tete MJ, Legendre C, Niaudet P, Antignac C (2004) NPHS2 mutation analysis shows genetic heterogeneity of steroid-resistant nephrotic syndrome and low post-transplant recurrence. Kidney Int 66:571–579
Frishberg Y, Rinat C, Megged O, Shapira E, Feinstein S, Raas-Rothschild A (2002) Mutations in NPHS2 encoding podocin are a prevalent cause of steroid-resistant nephrotic syndrome among Israeli-Arab children. J Am Soc Nephrol 13:400–405
Maruyama K, Iijima K, Ikeda M, Kitamura A, Tsukaguchi H, Yoshiya K, Hoshii S, Wada N, Uemuro O, Satamura K, Honda M, Yoshikawa N (2003) NPHS2 mutations in sporadic steroid- resistant nephrotic syndrome in Japanese children. Pediatr Nephrol 18:412–416
Caridi G, Berdeli A, Dagnino M, Di Duca M, Mir S, Cura A, Ravazzalo R, Ghiggeri GM (2004) Infantile steroid-resistant nephrotic syndrome associated with double homozygous mutations of podocin. Am J Kidney Dis 43:727–732
Ekim M, Özçakar ZB, Acar B, Yüksel S, Yalçınkaya F, Tulunay Ö, Ensari A, Erbay B (2004) Three siblings with steroid-resistant nephrotic syndrome: New NPHS2 mutations in a Turkish family. Am J Kidney Dis 44:E22–E24
International Study of Kidney Disease in Children (1981) The primary nephrotic syndrome in children. Identification of patients with minimal change nephrotic syndrome from initial response to prednisone. A report of the International Study of Kidney Disease in Children. J Pediatr 98:561–564
Yu Z, Ding J, Huang J, Yao Y, Xiao H, Zhang J, Liu J, Yang J (2005) Mutations in NPHS2 in sporadic steroid-resistant nephrotic syndrome in Chinese children. Nephrol Dial Transplant 20:902–908
Caridi G, Bertelli R, Di Duca M, Dagnino M, Emma F, Onetti Muda A, Scolari F, Miglietti N, Mazzucco G, Murer L, Carrea A, Massella L, Rizzoni G, Perfumo F, Ghiggeri GM (2003) Broadening the spectrum of disease related to podocin mutations. J Am Soc Nephrol 14:1278–1286
Koziell A, Grech V, Hussain S, Lee G, Lenkkeri U, Tryggvason K, Scombler P (2002) Genotype/phenotype correlations of NPHS1 and NPHS2 mutations in nephrotic syndrome advocate a functional inter-relationship in glomerular filtration. Hum Mol Genet 11:379–388
Acknowledgements
This study was supported by an Ankara University Research Project Grant (20040809190). F. Başak Cengiz is a student at the Biotechnology Institute of Ankara University
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Özçakar, Z.B., Cengiz, F.B., Çakar, N. et al. Analysis of NPHS2 mutations in Turkish steroid-resistant nephrotic syndrome patients. Pediatr Nephrol 21, 1093–1096 (2006). https://doi.org/10.1007/s00467-006-0116-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-006-0116-4