Abstract
The aim of this study was to define in children younger than 2 years of age the diagnostic significance of clinical and laboratory findings to localize site of febrile urinary tract infection. We reviewed the records of 185 children younger than 2 years of age admitted to hospital with febrile urinary tract infection. Patients were divided into having either acute pyelonephritis or acute cystitis according to the presence or absence of acute lesions on dimercaptosuccinic acid (DMSA) renal scintigraphy. Clinical and laboratory [white blood cell count (WBC), urinalysis, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP)] findings were compared between the two groups using Student’s t test, chi-square test, and multivariate analysis. Patients with pyelonephritis had statistically significant higher age, WBC, ESR, and CRP than those with cystitis. Although the sensitivity of the tests was 80–100%, their specificity was <28%. On multivariate analysis, 33% of patients with cystitis were diagnosed as having pyelonephritis, whereas 22% of those with pyelonephritis were considered to have cystitis. Given the low specificity of clinical findings and available laboratory tests to define the site of urine infection in this age group, we recommend DMSA renal scintigram as the test of choice to make the diagnosis of acute pyelonephritis in these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary tract infection (UTI) is common in infants and young children [1]. It may involve the upper (acute pyelonephritis) and/or the lower (cystitis, urethritis) urinary tract. Renal scarring is present in 8–40% of patients after an episode of acute pyelonephritis [2–8]. As a result of the renal scars, patients may develop hypertension and variable degrees of renal failure [9]. The differentiation between upper and lower UTI has important clinical implications in children younger than 2 years of age. In this group, the clinical presentation tends to be nonspecific, and the chance of renal damage after acute pyelonephritis is considered to be higher than in older children [2, 10, 11].
Dimercaptosuccinic acid (DMSA) renal scan is a sensitive, specific, and reproducible test to evaluate for acute pyelonephritis in patients presenting with UTI [12–15]. Many nephrologists and general pediatricians routinely make the diagnosis of acute pyelonephritis on clinical and laboratory data only, and DMSA renal scan is not widely used as an initial diagnostic test. This practice of low utilization of the test is consistent with the 1999 subcommittee on UTIs of the American Academy of Pediatrics statement that “the role of DMSA renal scan in the clinical management of the child with UTI still is unclear” [16].
The purpose of this study was to assess the accuracy of clinical findings and commonly requested laboratory tests to localize the site of UTI in the febrile child younger than 2 years of age with a documented UTI using DMSA scan as the gold standard for the diagnosis of acute pyelonephritis.
Patients and methods
This retrospective study included children and infants ages 3 months to 2 years admitted to Tampa General Hospital (Tampa, Florida, USA) and to Hospital Regional (Valdivia, Chile) between 1999 and 2004 with fever and in whom the diagnosis of UTI was made. Infection was defined by the presence of >100,000 colonies per milliliter of a single bacterial species on a specimen obtained by bladder catheterization. All children underwent renal planar scintigraphy after administration of DMSA, followed by delayed imaging 2–4 h later using a high-resolution pinhole collimator. Although this is a retrospective study, our policy has been to review renal scan images with a nuclear medicine physician to reach consensus regarding the presence or absence of parenchyma involvement. Renal scintigraphy was performed between 48 h and 5 days after admission to the hospital. The diagnosis of pyelonephritis was made by the presence of a diminished DMSA cortical uptake but preservation of the reniform outline. Cystitis was identified by the absence of photopenic renal parenchyma defects in patient with a documented UTI. Clinical findings included the presence of gastrointestinal (vomiting, diarrhea) and/or neurological symptoms (irritability, seizures) as well as fever (≥38°C) at the time of admission. Laboratory evaluation on admission included white blood cell count (WBC; normal <10,000 WBC/mm3), erythrocyte sedimentation rate (ESR; normal 0–10), C-reactive protein (CRP; normal <0.5 μg/ml), urinalysis (pyuria defined as >10 cells/high power field), nitrite test, and urine culture. Review of charts was approved by the Institutional Review Board committee of each institution.
Statistical analysis
Results are reported as mean ± standard deviation (SD). Comparisons of the mean response of the DMSA positive and negative groups were performed using Student’s t test for the numeric variables (age, temperature, WBC, ESR, and CRP). Chi-square tests comparing the two groups were conducted for dichotomous variables (nitrite and pyuria). Multivariate discriminating analysis was used to determine whether clinical and commonly requested laboratory tests can be used to discern between the DMSA positive and negative groups. Sensitivity, specificity, accuracy, and predictive values were calculated as per methodology reported by Galen [17]. All analyses were conducted using SAS 9.1.
Results
Demographics
One hundred eighty-five patients were included in the study. Of them, 97 were females and 88 males. Frequency and type of UTI by age are shown in Table 1. Seventy-four percent (137/185) of the patients were younger than 12 months old at the time of UTI diagnosis. Cystitis was present in 49.1% and acute pyelonephritis in 50.9% of patients. Males presented more cystitis and acute pyelonephritis than did females in the group <6 m of age. Cystitis and pyelonephritis in the groups older than 12 months were predominantly observed in females.
Diarrhea was most commonly seen in patients with acute pyelonephritis (p = 0.038). Vomiting and neurological findings did not differ significantly between patients with cystitis and those with acute pyelonephritis (Table 2).
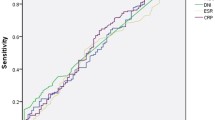
Comparisons between acute pyelonephritis and cystitis for quantitative variables (age, temperature, WBC, ESR, and CRP) are shown in Table 2. Patients presenting with acute pyelonephritis were older. Mean laboratory values were greater in patients with acute pyelonephritis compared with those with cystitis for all measures. Differences were statistically significant for CRP, ESR, and WBC and tending toward significance (p < 0.15) for pyuria and nitrite test. Sensitivity, specificity, and accuracy of individual laboratory tests and fever are shown in Table 3. All clinical and laboratory tests had high sensitivity but low specificity and accuracy.
To improve the diagnostic accuracy of laboratory tests, multivariate discriminating analysis was used to evaluate whether WBC, ESR, and CRP could be combined to improve the diagnosis of acute pyelonephritis. The combination of these three laboratory tests did not improve the accuracy of the diagnosis. Based on cross validation, 33% of the patients with acute cystitis were misclassified as having acute pyelonephritis, whereas 22% of those with acute pyelonephritis were misclassified as having cystitis.
Discussion
Febrile UTIs are common in young children. It is estimated that 60–65% of patients with a febrile UTI will have an acute pyelonephritis [1]. Our study demonstrates that neither clinical nor current available laboratory findings are accurate enough to confirm the diagnosis of acute pyelonephritis in children younger than 2 years of age with fever and UTI. We used the DMSA renal scan as the gold standard for the diagnosis of acute pyelonephritis [12], as it has a sensitivity of >90% and a specificity of 100% in the diagnosis of acute pyelonephritis [18–23]. The photopenic defect observed on DMSA scan is the result of a decrease in DMSA uptake by proximal tubular cells and decreased perfusion of the infected area. Because most UTIs are ascending in origin and involve the renal medulla prior to the cortex, it has been argued that some patients with early acute pyelonephritis may have no defects on DMSA scan (false negative results) because the lesions are only present in the renal medulla [13, 24].
There are no data that assess the false negative result rate using DMSA scan in children for the diagnosis of acute pyelonephritis. However, the scan needs to be performed when the bacteria have extended beyond the renal medulla and into the cortex. In this study, the scan was obtained between 48 h and 5 days after hospital admission. No data on serial scans defining the minimum time for optimal scanning are available. Hoberman et al. obtained scans 48 h after entering patients in their study. None of their patients initially presenting a normal DMSA renal scintigraphy was considered to have had acute pyelonephritis (false negative result) during follow-up [5].
The percentage of patients with acute pyelonephritis and cystitis in our study was similar to that observed by Hoberman in the same age group [5]. In contrast to Hoberman et al.’s study [5] but in agreement with others [25, 26], we observed a predominance of males in the first 6 months whereas females predominated after 12 months of age. In our study, fever was not significantly higher in patients with acute pyelonephritis, and extrarenal clinical findings could not discriminate between acute pyelonephritis and cystitis. Previous studies have not addressed extrarenal clinical findings when differentiating between upper and lower UTIs. In addition, fever has not been found significantly elevated in patients with pyelonephritis when compared with those with cystitis [27].
Acute-phase reactants (ESR, CRP, and WBC) in children with febrile UTI have been previously reported [6, 7, 25–31]. These studies have shown a statistically significantly increased level of WBC, CRP, and ESR in patients with acute pyelonephritis when compared with those with acute cystitis. These findings have led to the practice of obtaining these tests to differentiate between upper and lower UTIs. However, of the quoted studies, only a few have addressed the issue of specificity of these tests [7, 25, 26, 31]. Our study elaborates further on the use of acute phase reactant tests and demonstrates that they are not specific enough to confirm the diagnosis of acute pyelonephritis. In addition, comparison of our report to early studies is difficult for several reasons: (1) all previous studies include patients of all ages, (2) the time when the DMSA renal scan was performed is either not reported or, if given, it is unknown if those patients studied early had an increase rate of false negative results [7, 25, 26, 31]. In these previous reports, sensitivity of CRP and ESR tests varied from 72% to 93%, whereas specificity varied from 25% to 57%. Moreover, in those studies showing higher specificity, the cutoff values for CRP and ESR considered for identification of patients with acute pyelonephritis were arbitrarily increased [25]. This increased specificity was associated with a decrease in sensitivity of the test augmenting the number of false negative results. Therefore, it is impossible to select a cutoff level for CRP, ESR, or WBC that can afford discrimination between acute pyelonephritis and cystitis. At any cutoff point, sensitivity is sacrificed for specificity and vice versa.
We calculated accuracy of pyuria, CRP, ESR, and WBC to assess their discriminatory power in differentiating between pyelonephritis and cystitis. Our data showed that, at best, each test affords a 50/50 chance for patient younger than 2 years of age with a febrile UTI of having acute pyelonephritis. If every single test was unable to differentiate between cystitis and acute pyelonephritis in children younger than 2 years old, results combining the tests did not fare better.
When data on WBC, CRP, and ESR were analyzed in combination, 33% of patients showing no lesions on DMSA scan were diagnosed as having acute pyelonephritis, whereas 22% of those found to have inflammatory lesions on DMSA renal scan were reported as presenting acute cystitis. Multivariate analysis using CRP, ESR, and WBC has only been reported previously by Biggi et al. [25]. Their analysis is not comparable with ours because they only evaluated the number of true positive and false negative patients with documented acute pyelonephritis (diagnosis based on DMSA renal scan findings). Moreover, their true positive results included only patients with CRP, ESR, and WBC results above the median value of all patients studied.
We emphasize that our findings refer to patients 2 years old and younger with a documented febrile UTI. The lack of accuracy of the clinical and laboratory tests in the 3-months to 2-years age group does not imply that older patient evaluated for febrile UTI and complaining of flank pain also require a DMSA renal scan to make the diagnosis of pyelonephritis. However, even in older patients, the clinical diagnosis of acute pyelonephritis could be inaccurate, as Fairley et al., using the gold standard of a positive ureteral culture to make the diagnosis of acute pyelonephritis, demonstrated that 14% of patients presenting with flank pain and UTI did not have renal involvement [32].
There is the need to make an accurate diagnosis of acute pyelonephritis for several reasons:
-
1.
There is agreement that the antibiotic used for the treatment of acute pyelonephritis must have good tissue penetration because pyelonephritis is an interstitial nephritis. Thus, it is not appropriate to treat pyelonephritis with nitrofurantoin, a first-line antibiotic for UTI, which does not have tissue penetration. On the other hand, to use cefixime for acute cystitis might be considered overkill [33].
-
2.
The use of oral antibiotics to treat pyelonephritis on an outpatient basis has been recently advocated [5]. However, the trial was not specifically designed to assess whether oral or intravenous treatments for pyelonephritis were equivalent. Rather, it aimed at determining whether there were differences between them. Failure to show differences in a randomized trial does not mean that the treatments are equivalent [34, 35]. Until further studies resolve this controversy, it seems sensible to administer parenteral antibiotics as the initial therapy for acute pyelonephritis. Moreover, given the initial diagnostic uncertainty as to the presence of cystitis or pyelonephritis in these patients, it seems prudent to initially administer parenteral antibiotic therapy until results of the DMSA scan are available.
-
3.
Although there are no studies in children defining the length of therapy in the case of pyelonephritis, Johnson and Stamm [36] demonstrated in adults the need to treat acute pyelonephritis longer (14 days) than cystitis (up to 7 days).
For the above reasons, every effort should be made to accurately diagnose acute pyelonephritis in this age group. Lately, procalcitonin has been advocated as a sensitive and specific marker for acute pyelonephritis [37–39]. However, a recent study showed that at a 100% sensitivity, the specificity was only 42.8% [40].
In summary, our study shows that in patients younger than 2 years of age with febrile UTI, neither clinical nor laboratory data will allow an accurate diagnosis of acute pyelonephritis. Using the available laboratory criteria, the diagnosis will be missed in a large number of patients. In addition, many patients with cystitis will be classified as having acute pyelonephritis. Given the low specificity of clinical findings and available laboratory tests to define the site of urine infection in this age group, we recommend DMSA renal scintigram, when available, as the test of choice to make the diagnosis of acute pyelonephritis in these patients.
References
Hoberman A, Chao HP, Keller DM, Hickey R, Davis HW, Ellis D (1993) Prevalence of urinary tract infection in febrile infants. J Pediatr 123:17–23
Martinelli J, Claesson I, Lidin-Janson G, Jodal U (1995) Urinary infection, reflux and renal scarring in females continuously followed for 13–38 years. Pediatr Nephrol 9:131–136
Smellie J, Edwards D, Hunter N, Normand ICS, Prescod N (1975) Vesicoureteral reflux and renal scarring. Kidney Int 8:565–575
Rushton HG (1997) The evaluation of acute pyelonephritis and renal scarring with technetium 99m-dimercaptosuccinic acid renal scintigraphy: evolving concepts and future directions. Pediatr Nephrol 11:108–120
Hoberman A, Wald ER, Hickey RW, Baskin M, Charron M, Majd M, Kearney DH, Reynolds EA, Ruley J, Janosky JE (1999) Oral versus initial intravenous therapy for urinary tract infections in young febrile children. Pediatrics 104:79–86
Jakobsson B, Soderlundh S, Berg U (1992) Diagnostic significance of 99mTc-dimercaptosuccinic acid (DMSA) scintigraphy in urinary tract infection. Arch Dis Child 67:1338–1342
Benador D, Benador N, Slosman DO, Nussle D, Mermillod B, Girardin E (1994) Cortical scintigraphy in the evaluation of renal parenchyma changes in children with pyelonephritis. J Pediatr 124:17–20
Ataei N, Madani A, Habibi R, Khorasani M (2005) Evaluation of acute pyelonephritis with DMSA scans in children presenting after the age of 5 years. Pediatr Nephrol 20:1439–1444
Jacobson SH, Eklof O, Eriksson CG, Lins LE, Tidgren B, Winberg J (1989) Development of hypertension and uraemia after pyelonephritis in childhood: 27 year follow-up. BMJ 299:703–706
Gleeson FV, Gordon I (1991) Imaging in urinary tract infection. Arch Dis Child 66:1282–1283
Benador D, Benador N, Slosman D, Mermillod B, Girardin E (1997) Are younger children at highest risk of renal sequelae after pyelonephritis? Lancet 349:17–19
Piepsz A, Blaufox MD, Gordon I, Granerus G, Majd M, O’Reilly P, Rosenberg AR, Rossleigh MA, Sixt R (1999) Consensus on renal cortical scintigraphy in children with urinary tract infection. Scientific committee on radionuclides in nephrourology. Semin Nucl Med 29:160–174
Andrich MP, Majd M (1992) Diagnostic imaging in the evaluation of the first urinary tract infection in infants and young children. Pediatrics 90:436–441
De Sadeleer C, Tondeur M, Melis K, Van Espen MB, Verelst J, Ham H, Piepsz A (2000) A multicenter trial on interobserver reproducibility in reporting on 99mTc-DMSA planar scintigraphy: a Belgian survey. J Nucl Med 41:23–26
Basiratnia M, Nochi AH, Lofti M, Alavi MS (2006) Power Doppler sonographic evaluation of acute childhood pyelonephritis. Pediatr Nephrol 21:1854–1857
American Academy of Pediatrics, Committee on Quality Improvement, Subcommittee on Urinary Tract Infection (1999) Practice parameter: the diagnosis, treatment and evaluation of the initial urinary tract infection in febrile infants and young children. Pediatrics 103:843–852
Galen RS (1975) Predictive values of laboratory tests. Am J Cardiol 36:536–538
Arnold AJ, Brownless SM, Carty HM, Rickwood AM (1990) Detection of renal scarring by DMSA scanning-an experimental study. J Pediatr Surg 25:391–393
Rushton HG, Majd M (1992) Dimercaptosuccinic acid renal scintigraphy for the evaluation of pyelonephritis and scarring: a review of experimental and clinical studies. J Urol 148:1726–1732
Majd M, Rushton HG, Chandra R, Andrich MP, Tardiff CP, Rashti F (1997) Technetium-99-m-DMSA renal cortical scintigraphy to detect experimental acute pyelonephritis in piglets: comparison of planar (pinhole) and SPECT imaging. J Nucl Med 38:1731–1734
Risdon RA, Gosley ML, Parkhouse HF, Gordon I, Ransley PG (1994) Renal pathology and the 99mTc-DMSA image during the evolution of the early pyelonephritis scar: an experimental study. J Urol 151:767–773
Giblin JG, O’Connor KP, Fildes RD, Harkness B, Levin K, Newsome JT, Sesternhenn I, Gibbons MD (1993) The diagnosis of acute pyelonephritis in the piglet using single photon emission computerized tomography dimercaptosuccinic acid scintigraphy: a pathological correlation. J Urol 150:759–762
Craig JC, Wheeler DM, Irwig L, Howman-Giles RB (2000) How accurate is dimercaptosuccinic acid scintigraphy for the diagnosis of acute pyelonephritis? A meta-analysis of experimental studies. J Nucl Med 41:986–993
Linshaw MA (1999) Controversies in childhood urinary tract infections. World J Urol 17:383–395
Biggi A, Dardanell L, Pomero G, Cussino P, Noello C, Sernia O, Spada A, Camuzzini G (2001) Acute renal cortical scintigraphy in children with a first urinary tract infection. Pediatr Nephrol 16:733–738
Stokland E, Hellstrom M, Jacobsson B, Jodal U, Lungren P, Sixt R (1996) Early 99mTC dimercaptosuccinic acid (DMSA) scintigraphy in symptomatic first-time urinary tract infection. Acta Paediatr 85:430–436
Tappin DM, Murphy AM, Mocan H, Shaw R, Beattie TJ, McAllister TA, MacKenzie JR (1989) A prospective study of children with first acute symptomatic E. coli urinary infection. Early 99mtechnitium dimercaptosuccinic acid scan appearance. Acta Paediatr Scand 78:923–929
Hoberman A, Wald ER, Reynolds EA, Penchansky L, Charron M (1996) Is urine culture necessary to rule out urinary tract infection in young febrile children? Pediatr Infect Dis 15:304–309
Madj M, Rushton HG, Jantausch B, Wiedermann BL (1991) Relationship among vesicoureteral reflux, P-fimbriated Escherichia coli, and acute pyelonephritis in children with febrile urinary tract infection. J Pediatr 119:578–585
Mellis K, Vandeviveri J, Hoskens C, Vervaet A, Sand A, Van Acker KJ (1992) Involvement of the renal parenchyma in acute urinary tract infection: the contribution of 99mTc dimercaptosuccinic acid scan. Eur J Pediatr 151:536–539
Donoso G, Lobo G, Arnell F, Arteaga MP, Hevia P, Rosati P, Lagos E, Wolff C, Perez A, Jimenez C (2004) Tc 99M DMSA scintigraphy in children with a first episode of acute pyelonephritis: correlation with laboratory tests, echography and the presence of vesico-ureteral reflux. Rev Med Chil 132:58–64
Fairley KF, Carson NE, Gutch RC, Leighton P, Grounds AD, Laird EC, McCallum PH, Sleeman RL, O’Keefe CM (1971) Site of urinary tract-infection in general practice. Lancet 2:615–618
Fisher MC (1999) Pyelonephritis at home-why not? Pediatrics 104:109–111
Lozano JM (2004) Treatment of acute pyelonephritis in children. Conclusions should have been more cautious. BMJ 328:957
Jones B, Jarvis P, Lewis JA, Ebbutt AF (1996) Trials to assess equivalence: the importance of rigorous methods. BMJ 313:36–39
Johnson JR, Stamm WE (1989) Urinary tract infections in women: diagnosis and treatment. Ann Intern Med 111:906–917
Gervaix A, Galetto-Lacour A, Gueron T, Vadas L, Zamora S, Suter S, Girardin E (2001) Uselfulness of procalcitonin and C-reactive protein rapid tests for management of children with urinary tract infection. Pediatr Infect Dis J 20:507–511
Pecile P, Miorin E, Romanello C, Fallet E, Valent F, Giacomuzzi F, Tenore A (2004) Procalcitonin: A marker of severity of acute pyelonephritis in children. Pediatrics 114:e249–e254
Bigot S, Leblond P, Foucher C, Hue V, D’ Herbomez M, Foulard M (2005) Uselfulness of procalcitonin for the diagnosis of acute pyelonephritis in children. Arch Pediatr 12:1075–1080
Guven AG, Kazdal HZ, Koyun M, Aydin F, Gungor F, Akman S, Baysal YE (2006) Accurate diagnosis of acute pyelonephritis: how helpful is procalcitonin. Nucl Med Comm 27:715–721
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Garin, E.H., Olavarria, F., Araya, C. et al. Diagnostic significance of clinical and laboratory findings to localize site of urinary infection. Pediatr Nephrol 22, 1002–1006 (2007). https://doi.org/10.1007/s00467-007-0465-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-007-0465-7