Abstract
Background
Acute pyelonephritis (APN) can lead to renal scar formation, high blood pressure, and end-stage renal failure. Prompt and early diagnosis of APN is important for preventing future complications. Our goal was to study the mean platelet volume (MPV) as a predictor of APN in children.
Methods
The records of 43 patients with APN and 51 patients with a lower urinary tract infection (UTI) were investigated prospectively. APN was confirmed using radioactive nuclide 99mTc-DMSA scanning. The white blood cell (WBC) count, erythrocyte sedimentation rate (ESR), serum C-reactive protein (CRP), and MPV of both groups were measured and compared.
Results
The WBC count, MPV and ESR values, and the serum concentration of CRP were higher in the APN group than in the lower UTI group (p < 0.05). In the children with APN, the optimal cut-off value for the MPV was 8.2 fl [area under the curve (AUC): 0.906], with sensitivity of 81.4 % and specificity of 86.3 %. The MPV was associated with APN (p = 0.001), and the sensitivity and specificity of the MPV for the diagnosis of APN were higher than those of the other inflammation markers. MPV > 8.2 fl yielded an adjusted OR of 7.8 (95 % CI 3.3–18.4, p < 0.001) for APN. MPV > 8.2 fl was significantly associated with late renal scar formation (adjusted OR 5.7, 95 % CI 2.3–13.8, p < 0.001).
Conclusion
The MPV is a fast and reliable measurement with considerable predictive value for the diagnosis of APN and renal scars, and its predictive capacity is better than that of CRP, ESR, and WBC values.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary tract infections (UTIs) are common bacterial infectious diseases in infants and children [1]. UTIs can occur as bladder infections (lower UTI) or can also involve the kidneys (acute pyelonephritis) [2, 3]. Differentiating between these diseases is particularly difficult in infants and children, but it is necessary because pyelonephritis can lead to renal scar formation, high blood pressure, and end-stage renal failure in later life [4]. The prevalence of renal scarring due to acute pyelonephritis (APN) is 26.5–49 % [5].
A dimercaptosuccinic acid (DMSA) scan is considered the gold standard in imaging to determine renal parenchymal involvement [6]. However, a DMSA scan is not available in all medical centers and exposes children to radioactive chemicals. Although clinical symptoms, such as fever, abdominal pain, flank pain, nausea, and anorexia, and inflammatory markers, including white blood cells (WBC), the erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP), can determine the location of a UTI, these symptoms are not always reliable [7]. Therefore, a practical and prompt method that could assist clinicians in differentiating between upper and lower UTI is required.
There are several studies suggesting that platelets play an important role in the inflammatory response. Multiple inflammatory factors, such as cytokines and coagulation factors, are secreted by platelets [8]. The mean platelet volume (MPV) is a reflection of platelet size, which has been shown to correlate with platelet function and activation. A higher MPV value is indicative of increased platelet activity and thus more intense inflammation [9]. In recent years, studies have reported that MPV may be used as an inflammation marker in various diseases [10, 11].
We hypothesized that the MPV may be an easily measurable and reliable diagnostic method for distinguishing APN from lower UTI. Thus, the aim of this study was to determine the diagnostic value of the MPV in children with APN.
Materials and methods
Study population
This prospective study was conducted in the Department of Pediatrics at Adiyaman University Hospital, Turkey, between January 2013 and May 2104. Ninety-four patients aged from 2 months to 12 years with a first episode of UTI were enrolled. Inclusion criteria were as follows: (a) a first episode of a UTI; (b) the presence of clinical signs and symptoms, such as fever, abdominal pain, flank pain, dysuria, anorexia, and nausea; (c) pyuria (≥5 white blood cells per high-power field on spun urine); and (d) a positive urine culture. A positive urine culture was defined as more than 105 colony-forming units (CFUs)/ml of a single pathogen in a midstream clean-void urine sample or 104 CFUs/ml of a single pathogen in a sample obtained via urinary catheterization [12]. Patients with more than one organism in urine culture and those who had received antibiotic therapy or had a concomitant disease, such as septicemia, any type of renal disorder, congenital anomalies of the kidney and the urinary tract, chronic renal failure, or a previous diagnosis of vesicoureteral reflux (VUR), were excluded. Subjects with a history of smoking and patients with inflammatory, autoimmune, chronic infectious diseases, anemia, obesity, hypercholesterolemia, hypertension, diabetes mellitus, and chronic renal insufficiency were also excluded from the study.
Data from the analyses of the urine samples obtained by the midstream clean catch method in toilet-trained children and by urinary catheter in infants and small children were used. Immediately after collection, the samples were inoculated on plates containing sheep blood agar and MacConkey agar. All of the plates were inoculated at 35–37° C and examined 24–48 h after culturing to determine the colony count and to identify the bacteria.
All the patients underwent renal bladder ultrasonography (US) within 48 h of admission, in addition to a DMSA scan within 5 days of admission. Based on the results of the DMSA renal scan, the patients were divided into APN and lower UTI groups [6]. In the DMSA scan, APN was diagnosed upon observation of focal or diffuse areas of diminished uptake that are associated with preservation of renal cortical outline. Renal scar formation was diagnosed by decreases in kidney volume (manifested by cortex attenuation, renal morphological abnormality, or profile shrinkage), with wedge-shaped defects [2]. A lower UTI was diagnosed by a normal DMSA scan. A late DMSA scan was performed in cases with an atypical UTI [seriously ill, poor urine flow, abdominal or bladder mass, raised creatinine, septicemia, failure to respond to correct antibiotic treatment within 48 h, or infection with non-Escherichia coli (E. coli) organisms], positive US, or positive acute findings on DMSA scintigraphy 6 months later. The renal scarring was assessed by the findings of 99mTc-DMSA semi-quantitatively by one radiologist who was blind to clinical signs and symptoms. Voiding cystourethrography (VCUG) was used for select cases with positive findings on US or DMSA scintigraphy and an atypical UTI [13].
This study was approved by the Ethics Committee of Adıyaman University (No. 2013/11-1.2), and informed consent was obtained from all parents before study entry.
Data acquisition
The age, gender, weight, height, clinical findings, values of CRP, ESR, and MPV, and WBC counts, in addition to the results of urinalysis, urine culture, US, DMSA, and VCUG, were recorded from the patients’ charts.
Blood samples
Blood from both groups was drawn by venipuncture before and after antibiotic therapy. Each sample of whole blood was collected in tubes containing ethylenediaminetetraacetic acid and processed within one hour. The Sysmex XT 2000i (Roche Diagnostics GmbH, Mannheim, Germany) automated analyzer was used for complete blood counts. The reference range for the MPV was between 7.0 and 11 fl. The CRP levels were measured with the spectrophotometric method using the Cobas c 501 module of the Cobas 6000 series autoanalyzer (Roche Diagnostics GmbH, Mannheim, Germany). The ESR levels were measured by the Alifax SIR20 (SIRE Analytical Systems, Udine, Italy).
Statistical analysis
For the evaluation of the patient data, the Statistical Package for the Social Sciences, version 15.0, (SPSS, Inc., Chicago, IL) software was used. A Chi square test or independent two-sample t test was used to compare variables between the two groups. The discriminative ability of each biomarker for APN was evaluated by drawing receiver operating characteristic (ROC) curves for the biomarkers and calculating their sensitivity, specificity, predictive values, and likelihood ratios. The relationships between APN/late renal scars and the MPV, CRP value, WBC count, and ESR were analyzed with backward, stepwise multivariate logistic regression models for each biomarker if the model assumption of linearity was violated. The mean ± SD of all the determined values was obtained. A p value <0.05 was considered statistically significant.
Results
Among the 94 children with a first episode of a UTI, 43 had APN (30 females and 13 males), and 51 had a lower UTI (36 females and 15 males) (p = 0.389). The minimum and maximum ages of the patients in the APN group were 3 months and 11 years, respectively, with a mean of 2.1 ± 1.98 years. Seven males and seven females in the APN group were <1 year, four males and 14 females were between 1 and 3 years, and two males and nine females were ≥3 years. The minimum and maximum ages of the patients in the lower UTI group were 2 months and 12 years, respectively, with a mean of 2.3 ± 2.18 years. Seven males and 11 females in the lower UTI group were <1 year, five males and 16 females were between 1 and 3 years, and three males and nine females were ≥3 years (p = 0.890). There was no statistically significant difference between the two groups in terms of age and gender (p > 0.05).
The most frequent clinical symptoms in the APN and lower UTI patients were fever, anorexia, and dysuria. Among the patients with APN, 35 had fever with temperature >39 °C (81.4 %), 30 had anorexia (69.8 %), 26 had dysuria, or crying while urinating (60.5 %), 15 had abdominal pain (34.9 %), and eight had nausea (18.6 %). These ratios in the patients with lower UTI were 56.9, 64.7, 62.7, 29.4, and 15.6 %, respectively. Fever (>39 °C) was more frequently observed in the patients with APN (p = 0.01), but there was no statistically significant difference between the two groups in terms of other symptoms (p > 0.05). E. coli was the most common organism responsible for the UTIs in the two groups: 69.8 % in APN cases and 78.4 % in lower UTI cases (p = 0.642). Gram-positive organisms were 11.6 % in APN cases and 9.6 % in lower UTI cases. Abnormal findings on the US in the APN group were dilation of the pelvicalyceal system (27.9 %), hydronephrosis (11.6 %), ureteropelvic junction obstruction (2.3 %), and kidney stones (4.6 %). These values in the lower UTI group were 9.2, 4.6, 2.3, and 2.3 %, respectively. Late renal scar formation was detected in 17 APN patients (39.5 %) and three lower UTI patients (5.9 %). VCUG was performed in 22 APN patients and eight lower UTI patients. VUR was detected in ten APN patients (23.3 %) (five had grade 1 VUR, two had grade 2 VUR, and three had grade ≥3 VUR) and two lower UTI patients (one had grade 1 VUR, and one had grade 2 VUR).
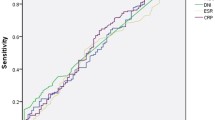
The WBC count, MPV and ESR values, and serum concentrations of CRP were higher in the APN group than in the lower UTI group (p < 0.001) (Table 1). The sensitivity, specificity, positive predictive values, negative predictive values, positive likelihood ratios, and negative likelihood ratios of the inflammatory markers were determined with different cut-off values (Table 2). The median area under the ROC curve was 0.906 for the MPV [95 % confidence interval (CI) 0.828–0.957, p = 0.001], 0.813 for CRP (95 % CI 0.720–0.886, p = 0.001), 0.744 for the WBC count (95 % CI 0.644–0.829, p = 0.001), and 0.717 for the ESR (95 % CI 0.614–0.805, p = 0.01) (Fig. 1).
In all UTI patients, no statistically significant difference was found in MPV values between the patients with Gram-positive infections and Gram-negative infections (8.74 ± 0.78 and 9.02 ± 0.69 fl, respectively; p = 0.679). The MPV values were higher in patients with VUR compared to patients without VUR (9.79 ± 0.88 and 8.71 ± 0.69 fl, respectively; p = 0.001). Also, MPV values were higher in the patients with late renal scars compared to patients without late renal scars (9.71 ± 0.82 and 8.61 ± 0.62 fl, respectively; p < 0.001).
The MPV was significantly associated with APN (Table 3). MPV > 8.2 fl yielded an adjusted OR of 7.789 (95 % CI 3.299–18.388, p < 0.001). The CRP and WBC count were also significantly related to APN. The ESR was not related to APN. The MPV was significantly associated with late renal scars (Table 3). MPV > 8.2 fl yielded an adjusted OR of 5.696 (95 % CI 2.348–13.821, p < 0.001). VUR was also significantly related to late renal scars (OR 0.061, 95 %CI 0.013–0.297, p = 0.001). The CRP, WBC count, and ESR were not related to late renal scars.
The before and after treatment values of MPV were 9.41 ± 0.79 and 7.62 ± 0.87 fl, respectively, and the CRP levels were 27.19 ± 18.29 and 6.13 ± 3.14 mg/dL, respectively. Significant differences in the MPV and CRP were observed before and after treatment (p < 0.05).
Discussion
We demonstrated that the MPV is a fast and reliable measurement and that it has considerable predictive value for the diagnosis of APN and renal scars. Moreover, its predictive capacity was better than that of the CRP, ESR, or WBC values regardless of considered thresholds.
Delay in the diagnosis of APN can lead to severe complications, such as renal scarring, arterial hypertension, and chronic renal failure. Differentiating APN from lower UTI is difficult based on common clinical manifestations and laboratory indices. Although the DMSA renal scan is the gold standard to differentiate APN from lower UTI, it is not available in all medical centers. In addition, this method is costly and exposes children to radioactive chemicals. Furthermore, DMSA cannot distinguish between old scarring and acute parenchymal involvement [14, 15]. Thus, an easier and more practical method is necessary.
Serum CRP, ESR, and WBC are acute-phase reactants that are used to diagnose APN and to distinguish APN from lower UTI [16]. Some studies reported that CRP, ESR, and WBC values were neither entirely sensitive nor specific for distinguishing APN from lower UTI [17–19]. Others reported that rapid diagnostic tests, such as serum procalcitonin, interleukin (IL)-1β, IL-6, and IL-8, can be used to diagnose APN [19, 20]. In contrast, some studies found that these rapid diagnostic tests were not valuable markers for differentiating between APN and lower UTI [21, 22].
The MPV is a simple, cheap, and easy biomarker of platelet function because it can be measured in almost all laboratories. The platelet volume is correlated with platelet function and activation [23]. In addition to their primary hemostatic function, platelets are involved in the pathogenesis of infectious diseases [24]. Previous studies suggested that cytokines, such as IL-3 and IL-6, may influence megakaryocyte ploidy, leading to the production of larger and more reactive platelets [25]. Sheu et al. [20] showed that invasion of the lipid A component of endotoxin and P fimbriae present in E. coli and other Gram-negative bacteria induces inflammation and the release of IL-1β, IL-6, and IL-8 cytokines. Hence, elevated levels of IL-6 in APN might be the result of an increased MPV. Based on observations of the MPV, we hypothesized that this inflammation marker might be used for the diagnosis of APN.
To our knowledge, only one study has investigated the relationship between the MPV and APN. In our study, the values of all the inflammatory markers (WBC, ESR, CRP, and MPV values) were greater in the APN group than in the lower UTI group. These findings are compatible with those of Catal et al. [26]. They noted that platelet counts were higher in APN patients and MPV values were higher in Gram-positive infections compared with Gram-negative infections. In contrast to their study, we found that the platelet counts in the APN and lower UTI patients were similar. In addition, there was no statistically significant difference in MPV values between those with Gram-positive infections and Gram-negative infections. Catal et al. did not provide data on the sensitivity and specificity of the MPV or the other acute-phase reactants assessed in their study. They also provided no data on the relation between the MPV and late renal scars. In our study, the sensitivity, specificity, and positive and negative predictive values of the MPV using a cut-off value of >8.2 fl was 81.4, 86.3, 84.6, and 83.3 %, respectively, in predicting APN. Based on the ROC curve, the sensitivity, specificity, positive predictive value, and negative predictive value of the MPV were higher than those of the WBC, CRP, and ESR levels. The MPV (OR 7.789, 95 % CI 3.299–18.388, p < 0.001), CRP (OR 1.059, 95 % CI 1.013–1.107, p = 0.011), and WBC (OR 1.000, 95 %CI 1.000–1.000, p = 0.024) were significantly related to APN. However, the ESR was not related to APN.
The MPV and CRP levels after the treatment significantly decreased compared with those before the treatment (p < 0.05), suggesting that both biomarkers can be used for observing pathogenesis and curative effects. We also found that the MPV (OR 5.696, 95 % CI 2.348–13.821, p < 0.001) and VUR (OR 0.061, 95 %CI 0.013–0.297, p = 0.001) were significantly associated with renal scars. There was no association between CRP, WBC, and ESR levels and late renal scars.
Conclusion
MPV is a simple parameter that is provided by most commercially available automated hematology analyzers. Our data from this study suggest that MPV values were significantly higher among patients with APN and that MPV is a reliable marker for differentiating APN from lower UTIs. They also indicate that the MPV is a reliable marker for predicting late renal scars. Further studies with a larger patient population are required to establish the exact role of MPV values in patients with APN.
References
Buonsenso D, Cataldi L. Urinary tract infections in children: a review. Minerva Pediatr. 2012;64:145–57.
Elder JS. Urinary tract infection. In: Kliegman RM, Stanton BF, St. Geme JW, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 19th ed. Philadelphia: Saunders; 2011. pp. 1829–38.
Edefonti A, Tel F, Testa S, De Palma D. Febrile urinary tract infections: clinical and laboratory diagnosis, imaging, and prognosis. Semin Nucl Med. 2014;44:123–8.
Jacobson SH, Eklöf O, Eriksson CG, Lins LE, Tidgren B, Winberg J. Development of hypertension and uraemia after pyelonephritis in childhood: 27 year follow up. BMJ. 1989;299:703–6.
Faust WC, Diaz M, Pohl HG. Incidence of post-pyelonephritic renal scarring: a meta-analysis of the dimercapto-succinic acid literature. J Urol. 2009;181:290–7.
Shaikh N, Ewing AL, Bhatnagar S, Hoberman A. Risk of renal scarring in children with a first urinary tract infection: a systematic review. Pediatrics. 2010;126:1084–91.
Mori R, Lakhanpaul M, Verrier-Jones K. Diagnosis and management of urinary tract infection in children: summary of NICE guidance. BMJ. 2007;335:395–7.
Bath PM, Butterworth RJ. Platelet size: measurement, physiology and vascular disease. Blood Coagul Fibrinolysis. 1996;7:157–61.
Gasparyan AY, Ayvazyan L, Mikhailidis DP, Kitas GD. Mean platelet volume: a link between thrombosis and inflammation? Curr Pharm Des. 2011;17:47–58.
Cengiz C, Erhan Y, Murat T, Ercan A, Ibrahim S, Ihsan G, et al. Values of mean platelet volume in patients with chronic tonsillitis and adenoid hypertrophy. Pak J Med Sci. 2013;29:569–72.
Karadag-Oncel E, Ozsurekci Y, Kara A, Karahan S, Cengiz AB, Ceyhan M. The value of mean platelet volume in the determination of community acquired pneumonia in children. Ital J Pediatr. 2013;39:16.
White B. Diagnosis and treatment of urinary tract infections in children. Am Fam Physician. 2011;83:409–15.
La Scola C, De Mutiis C, Hewitt IK, Puccio G, Toffolo A, Zucchetta P, et al. Different guidelines for imaging after first UTI in febrile infants: yield, cost, and radiation. Pediatrics. 2013;131:665–71.
Jakobsson B, Nolstedt L, Svensson L, Söderlundh S, Berg U. 99 m Technetium-dimercaptosuccinic acid scan in the diagnosis of acute pyelonephritis in children: relation to clinical and radiological findings. Pediatr Nephrol. 1992;6:328–34.
Ifergan J, Pommier R, Brion MC, Glas L, Rocher L, Bellin MF. Imaging in upper urinary tract infections. Diagn Interv Imaging. 2012;93:509–19.
Al-Sayyad AJ, EL-Morshedy SM, Abd Al Hamid EA, Karam NA, Imam ABA, Karam RA. Evaluation of biomarkers to differentiate upper from lower urinary tract infections in children. UroToday Int J. 2011;4:49.
Ayazi P, Mahyar A, Daneshi MM, Jahani Hashemi H, Pirouzi M, Esmailzadehha N. Diagnostic accuracy of the quantitative C-reactive protein, erythrocyte sedimentation rate and white blood cell count in urinary tract infections among infants and children. Malays J Med Sci. 2013;20:40–6.
Kotoula A, Gardikis S, Tsalkidis A, Mantadakis E, Zissimopoulos A, Deftereos S, et al. Comparative efficacies of procalcitonin and conventional inflammatory markers for prediction of renal parenchymal inflammation in pediatric first urinary tract infection. Urology. 2009;73:782–6.
Gurgoze MK, Akarsu S, Yilmaz E, Gödekmerdan A, Akça Z, Ciftçi I, et al. Proinflamtory cytokines and procalcitonin in children with acute pyelonephritis. Pediatr Nephrol. 2005;20:1445–8.
Sheu JN, Chen MC, Lue KH, Cheng SL, Lee IC, Chen SM, et al. Serum and urine levels of interleukin-6 and interleukin-8 in children with acute pyelonephritis. Cytokine. 2006;36:276–82.
Mahyar A, Ayazi P, Ahmadi R, Daneshi-Kohan MM, Hashemi HJ, Dalirani R, et al. Are serum procalcitonin and interleukin-1 beta suitable markers for diagnosis of acute pyelonephritis in children? Prague Med Rep. 2014;115:16–23.
Krzemien G, Roszkowska-Blaim M, Kostro I, Szmigielska A, Karpinska M, Sieniawska M, et al. Urinary levels of interleukin-6 and interleukin-8 in children with urinary tract infections to age 2. Med Sci Monit. 2004;10:593–7.
Martin JF, Trowbridge EA, Salmon G, Plumb J. The biological significance of platelet volume: its relationship to bleeding time, platelet thromboxane B2 production and megakaryocyte nuclear DNA concentration. Thromb Res. 1983;32:443–60.
Becchi C, Al Malyan M, Fabbri LP, Marsili M, Boddi V, Boncinelli S. Mean platelet volume trend in sepsis: is it a useful parameter? Minerva Anestesiol. 2006;72:749–56.
Kaser A, Brandacher G, Steurer W, Kaser S, Offner FA, Zoller H, et al. Interleukin-6 stimulates thrombopoiesis through thrombopoietin: role in inflammatory thrombocytosis. Blood. 2001;98:2720–5.
Catal F, Bavbek N, Bayrak O, Uz E, Isik B, Karabel M, et al. Platelet parameters in children with upper urinary tract infection: is there a specific response? Ren Fail. 2008;30:377–81.
Conflict of interest
The authors have declared that no conflict of interest exists.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Tekin, M., Konca, C., Gulyuz, A. et al. Is the mean platelet volume a predictive marker for the diagnosis of acute pyelonephritis in children?. Clin Exp Nephrol 19, 688–693 (2015). https://doi.org/10.1007/s10157-014-1049-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-014-1049-z