Abstract
Current formulas that estimate the delivered dose of hemodialysis rely upon pre- and post-treatment blood urea nitrogen (BUN) concentrations for calculation. Single-pool kinetic modeling (spKt/V) uses a convenient 30-s post-dialysis BUN sample but does not take urea rebound into account. Double-pool modeling (eKt/V) uses an equilibrated BUN (eqBUN) and is the best reflection of the true urea mass removed by hemodialysis but is inconvenient for patients and costly to the dialysis unit to wait to obtain an eqBUN sample. We compared simple spKt/V and eKt/V estimation formulas using data obtained from the Centers for Medicare & Medicaid Services (CMS) End Stage Renal Disease (ESRD) Clinical Performance Measures (CPM) Project to determine how frequently these two results would lead to different prescription management. We set an expected difference Kt/V (spKt/V−eKt/V) of 0.20 based on results of the Hemodialysis (HEMO) Study; 1,513 paired spKt/V and estimated eKt/V results were available for comparison. For patients with an arteriovenous fistula (AVF) or arteriovenous graft (AVG) (n=720), mean spKt/V and estimated eKt/V were 1.62±0.30 and 1.37±0.26, respectively. For patients with a catheter (n=793), mean spKt/V and estimated eKt/V were 1.53±0.32 and 1.33±0.29, respectively. Examination of the different spKt/V and estimated eKt/V pairings revealed a greater adequacy discordance rate between a 0.20 difference in spKt/V and estimated eKt/V at higher Kt/V values, but Kt/V discordance rates only varied from 0.3 to 5.5% depending on the paired Kt/V values used.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Current formulas that estimate the delivered dose of hemodialysis rely upon pre- and post-treatment blood urea nitrogen (BUN) concentrations for calculation [1]. The effect of post-dialysis urea rebound on the calculation of Kt/V has been the subject of significant recent research [2–8]. The relatively rapid removal of BUN during hemodialysis causes BUN concentration disequilibrium between intracellular (ICF) and extracellular (ECF) fluid spaces. The ECF BUN concentration rebounds in a logarithmic fashion for 1 h after the hemodialysis treatment as BUN equilibrates between the ICF and ECF. Since Kt/V calculation is based in part on the post-hemodialysis BUN level, urea rebound has a significant impact upon the calculation of the delivered dose of hemodialysis. While single-pool kinetic modeling (spKt/V) uses a convenient 30-s post-dialysis BUN sample, it does not take urea rebound into account. Double-pool modeling (eKt/V) uses an equilibrated BUN (eqBUN) and is the best reflection of the true urea mass removed by hemodialysis. However, it is inconvenient for patients and costly to the dialysis unit to wait 1 hour post-dialysis to obtain an eqBUN sample. Several formulas have been developed to approximate double-pool equilibrated Kt/V without obtaining a measured eqBUN [3, 4, 6].
No large-scale study has examined the differences between spKt/V and eKt/V measurement in pediatric patients receiving hemodialysis. We utilized data from the Centers for Medicare & Medicaid Services (CMS) End Stage Renal Disease (ESRD) Clinical Performance Measures (CPM) Project to calculate both spKt/V and estimate eKt/V in a large cohort of pediatric patients receiving maintenance hemodialysis. The aims of the current study were to (1) determine the differences between spKt/V and estimated eKt/V, (2) determine if hemodialysis access affects Kt/V calculation, and (3) assess if management of the hemodialysis prescription would differ based on whether delivered hemodialysis doses were measured by spKt/V versus estimated eKt/V.
Methods
Patient population
Since 1999, the CMS ESRD CPM Project has collected data on all pediatric in-center hemodialysis patients in the United States aged from 12 years up to but not including 18 years. Since study year 2002, the ESRD CPM Project has included data from all in-center pediatric hemodialysis patients less than 18 years of age. We included data from all pediatric patients aged 0–18 years in the CPM database.
Data collection methods
All in-center hemodialysis patients <18 years old (hereafter referred to as pediatric patients) identified by the 18 ESRD Networks (regional organizations contracted by CMS to perform quality oversight activities to assure the appropriateness of services and protection for dialysis patients) as receiving hemodialysis on 31 December 2002 were entered into the study. During May 2003, a three-page data collection form was sent to each facility that had one or more pediatric patients receiving maintenance hemodialysis. The use of these forms was authorized through the National Institutes of Health clinical exemption process. Descriptive information on each selected patient and hemodialysis facility was printed on gummed labels and sent to the individual ESRD Networks along with the forms to be used to collect data. Clinical information in the patients’ medical records was abstracted for each pediatric patient who was receiving in-center hemodialysis during the months of October, November, and December 2002. ESRD CPM data relevant for the current study included: patient age, vascular access information, pre- and post-dialysis weight, pre- and post-dialysis BUN concentrations, and dialysis session lengths for spKt/V and estimated eKt/V calculations.
Completed forms were returned to the appropriate Network office where data were reviewed for acceptability and manually entered into a computerized database (Visual FoxPro). The data were aggregated by The Renal Network, Inc. and forwarded to CMS for analysis.
Kt/V calculation
Single-pool Kt/V was calculated using the second-generation natural logarithm equation of Daugirdas, which has been validated as an acceptable surrogate to formal urea kinetic modeling [9, 10]:
where C0=pre-dialysis BUN (mg/dl), C1=post-dialysis BUN (mg/dl), t=session length (h), UF=ultrafiltrate (kg), and W=post-dialysis weight (kg).
Equilibrated Kt/V was estimated using the rate equation specific for the type of vascular access [6]:
where T=treatment time in hours and spKt/V was calculated using Eq. (1).
spKt/V versus estimated eKt/V value management comparison
Since the difference between spKt/V and estimated eKt/V for the large group of adult patients reported in the Hemodialysis (HEMO) Study was 0.16 in the low-dose group and 0.18 in the high-dose group, we opted to set a paired difference between spKt/V and estimated eKt/V (ΔKt/V=spKt/V-estimated eKt/V) of greater than 0.20 as a threshold for a difference in hemodialysis dose prescription management [11]. We chose to set the 0.20 ΔKt/V limit, which is slightly higher than the mean ΔKt/V seen in the HEMO Study, because children potentially receive more efficient dialysis as a result of a higher K/V ratio and would conceivably have greater urea rebound and resultant greater ΔKt/V. We then compared paired spKt/V versus estimated eKt/V combinations: spKt/V >1.2 and estimated eKt/V <1.0, spKt/V >1.4 and estimated eKt/V <1.2, and spKt/V >1.6 and estimated eKt/V <1.4 to determine how often spKt/V and estimated eKt/V results lead to different hemodialysis prescription adjustments. For example, if a patient’s paired spKt/V versus estimated eKt/V results were 1.5 and 1.18, respectively, we hypothesized that a difference in prescription management would result theoretically—no change based on the spKt/V value and increase prescribed dose based on the estimated eKt/V value.
Statistical analysis
Comparison of spKt/V and estimated eKt/V values was made by linear regression analysis. Potential association between patient post-dialysis weight and ΔKt/V was performed by linear regression analysis. Rates of predicted hemodialysis prescription change (i.e., if Kt/V was less than lower threshold limit) were compared between spKt/V and estimated eKt/V for each lower threshold pair by chi-square analysis. Comparison of mean values between groups was performed by unpaired t-test. A p value <0.05 was considered significant.
Results
There were 663 patients in the file for analysis. Ninety-four percent (625/663) of the patients had at least one paired spKt/V and estimated eKt/V result. Vascular access information was available for 99% (659/663) of the patients. Characteristics of the patients in the analysis are shown in Table 1. Patients with AV were older and larger than patients with VV.
A total of 1,513 paired spKt/V and estimated eKt/V results were available for comparison: 720 paired results were obtained from patients dialyzed by an AVF or AVG (AV) and 793 paired results were obtained from patients dialyzed by a central venous catheter (VV). Mean AV spKt/V and estimated eKt/V were 1.63±0.30 and 1.37±0.26, respectively. Mean VV spKt/V and estimated eKt/V were 1.53±0.32 and 1.33±0.29, respectively. Patients with AV had significantly higher spKt/V but not eKt/V (Table 1).
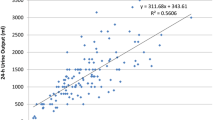
Mean spKt/V and estimated eKt/V values for both AV and VV accesses demonstrated tight correlation across the entire spKt/V range (r=0.99, p<0.0001). ΔKt/V demonstrated a trend toward a greater discrepancy for smaller patients (r 2=−0.34, p<0.001), which was consistent across all access types (Figs. 1, 2, and 3).
Examination of the different spKt/V and estimated eKt/V pairings revealed a greater adequacy discordance rate between a 0.20 difference in spKt/V and estimated eKt/V at higher values (Fig. 4, Table 2). Bland-Altman analysis demonstrated a ΔKt/V maximum 0.29 for spKt/V values less than 1.4, whereas ΔKt/V ranged from 0.13 to 0.56 for spKt/V values greater than or equal to 1.4 (Fig. 4). ΔKt/V was greater or equal to 0.3 in 46 of 379 cases where spKt/V was greater than or equal to 1.4. Only 5 total samples were discordant in the spKt/V >1.2 and estimated eKt/V <1.0 pair, 26 total paired samples were discordant between the spKt/V >1.4 and estimated eKt/V <1.2 pair, whereas 83 total samples were discordant between the spKt/V >1.6 and estimated eKt/V <1.4 threshold (p<0.05). Thus, for spKt/V >1.4, a discordance rate of less than 3% was observed. Neither mean post-dialysis weights nor patient ages differed for patients with versus without discordant values.
Discussion
Delivered hemodialysis dose measurement currently utilizes calculations that reflect urea mass removed during the treatment. Hemodialysis dose management is based on delivering a minimally acceptable or “adequate” amount of urea clearance. Kt/V, a unitless term which reflects urea clearance normalized for urea distribution across patient total body water, depends on sampling of a pre- and post-treatment serum BUN concentration. While using an equilibrated post-treatment BUN sample or methods to estimate double-pool equilibrated Kt/V will lead to lower values that better reflect the true urea mass removed than spKt/V methods, no published pediatric study has assessed for the likelihood of whether hemodialysis dose prescription change would differ based on spKt/V versus estimated eKt/V criteria.
We assumed a ΔKt/V of 0.20 to be expected to result from urea rebound based on data for the HEMO Study that showed an average ΔKt/V of 0.16. Data from our current study using CMS ESRD CPM Project data demonstrate a similar ΔKt/V of 0.21–0.26 based on patient vascular access. Children might be expected to have higher rebound and resultant greater ΔKt/V than adults since they receive more efficient dialysis (i.e., a higher K/V ratio), although this has yet to be verified by direct measurement and the mechanisms which result in rebound in adults (such as cardiopulmonary recirculation) may be irrelevant in children with normal myocardial reserve and well-preserved vascular tone. Patients with AV had significantly higher spKt/V, but not eKt/V than patients with VV. Patients with VV were also significantly smaller and younger than patients with AV, which may thus solely reflect greater rebound in smaller patients, and not be a function of access type.
The fact that we observed a trend toward greater ΔKt/V in smaller patients who typically receive the most efficient dialysis supports the concept that urea rebound may be greater in smaller children, who may therefore be at a greater risk for hemodialysis prescription discrepancy based on spKt/V versus estimated eKt/V criteria. As a result, the 0.20 ΔKt/V threshold led to more potential hemodialysis prescription discrepancies at higher Kt/V values. We realize the use of the Daugirdas rate equation may have led to the increased ΔKt/V in smaller patients, since smaller patients likely receive shorter dialysis times. Thus, our data may merely reflect a mathematical tautology inherent with the rate equation and not a true physiological phenomenon. In fact, recent pediatric data demonstrate the questionable consistency of the Daugirdas rate equation in children [3]. Nonetheless, the low discordance rate seen across the entire patient cohort argues for spKt/V to be a clinically acceptable tool for patient hemodialysis adequacy management.
It was not the purpose of the current study to define the minimally adequate or optimal hemodialysis dose for pediatric patients. We realize that the mean delivered dose of dialysis observed in this study is higher than recommended by the Kidney Dialysis Outcomes Quality Initiative (K/DOQI) guidelines and that no study has demonstrated conclusive benefit of delivered dialysis at these doses, although one study showed improved growth in children with spKt/V of 2 and enhanced protein administration [12]. Such recommendations would require long-term outcome studies that control for hemodialysis (HD) dose. Given the discrepancies between spKt/V and estimated eKt/V, we suggest that any pediatric study which controls for HD dose should use estimated eKt/V instead of spKt/V methods to most precisely quantify the delivered HD dose across the range of patient sizes and doses delivered in pediatric practice. Given the concerns cited above, more precise and validated formulas than the Daugirdas rate equation may be preferable for outcome study purposes [3, 5], and certainly more study is required to confidently promote acceptance of the Daugirdas rate equation for standard clinical practice in estimating eKt/V in pediatric patients receiving hemodialysis.
References
(1997) NKF-DOQI clinical practice guidelines for hemodialysis adequacy. National Kidney Foundation. Am J Kidney Dis 30:S15–S66
Goldstein SL (2004) Adequacy of dialysis in children: does small solute clearance really matter? Pediatr Nephrol 19:1–5
Goldstein SL, Brewer ED (2000) Logarithmic extrapolation of a 15-minute postdialysis BUN to predict equilibrated BUN and calculate double-pool Kt/V in the pediatric hemodialysis population. Am J Kidney Dis 36:98–104
Maduell F, Garcia-Valdecasas J, Garcia H, Hernandez-Jaras J, Siguenza F, del Pozo C, Giner R, Moll R, Garrigos E (1997) Validation of different methods to calculate Kt/V considering postdialysis rebound. Nephrol Dial Transplant 12:1928–1933
Sharma A, Espinosa P, Bell L, Tom A, Rodd C (2000) Multicompartment urea kinetics in well-dialyzed children. Kidney Int 58:2138–2146
Daugirdas JT, Schneditz D (1995) Overestimation of hemodialysis dose depends on dialysis efficiency by regional blood flow but not by conventional two pool urea kinetic analysis. ASAIO J 41:M719–M724
Leblanc M, Charbonneau R, Lalumiere G, Cartier P, Deziel C (1996) Postdialysis urea rebound: determinants and influence on dialysis delivery in chronic hemodialysis patients. Am J Kidney Dis 27:253–261
Pedrini LA, Zereik S, Rasmy S (1988) Causes, kinetics and clinical implications of post-hemodialysis urea rebound. Kidney Int 34:817–824
Daugirdas JT (1993) Second generation logarithmic estimates of single-pool variable volume Kt/V: an analysis of error. J Am Soc Nephrol 4:1205–1213
Goldstein SL, Sorof JM, Brewer ED (1999) Natural logarithmic estimates of Kt/V in the pediatric hemodialysis population. Am J Kidney Dis 33:518–522
Eknoyan G, Beck GJ, Cheung AK, Daugirdas JT, Greene T, Kusek JW, Allon M, Bailey J, Delmez JA, Depner TA, Dwyer JT, Levey AS, Levin NW, Milford E, Ornt DB, Rocco MV, Schulman G, Schwab SJ, Teehan BP, Toto R (2002) Effect of dialysis dose and membrane flux in maintenance hemodialysis. N Engl J Med 347:2010–2019
Tom A, McCauley L, Bell L, Rodd C, Espinosa P, Yu G, Yu J, Girardin C, Sharma A (1999) Growth during maintenance hemodialysis: impact of enhanced nutrition and clearance. J Pediatr 134:464–471
Disclaimer
The views expressed in this manuscript are those of the authors and do not necessarily reflect official policy of the Centers for Medicare & Medicaid Services.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goldstein, S.L., Brem, A., Warady, B.A. et al. Comparison of single-pool and equilibrated Kt/V values for pediatric hemodialysis prescription management: analysis from the Centers for Medicare & Medicaid Services Clinical Performance Measures Project. Pediatr Nephrol 21, 1161–1166 (2006). https://doi.org/10.1007/s00467-006-0112-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-006-0112-8