Abstract
Background
Self-expanding metallic stents (SEMSs) are used as a bridge to surgery in patients with obstructive colorectal cancer. However, the role of laparoscopic resection after successful stent deployment is not well established. We aimed to compare the oncologic outcomes of laparoscopic vs open surgery after successful colonic stent deployment in patients with obstructive left-sided colorectal cancer.
Methods
In this multicenter study, 179 (97 laparoscopy, 82 open surgery) patients with obstructive left-sided colorectal cancer who underwent radical resection with curative intent after successful stent deployment were retrospectively reviewed. To minimize bias, we used inverse probability treatment-weighted propensity score analysis. The short- and long-term outcomes between the groups were compared.
Results
Both groups had similar demographic and tumor characteristics. The operation time was longer, but the degree of blood loss was lower in the laparoscopy than in the open surgery group. There were nine (9.3%) open conversions. After adjustment, the groups showed similar patient and tumor characteristics. The 5-year disease-free survival (DFS) (laparoscopic vs open: 68.7% vs 48.5%, p = 0.230) and overall survival (OS) (laparoscopic vs open: 79.1% vs 69.0%, p = 0.200) estimates did not differ significantly across a median follow-up duration of 50.5 months. Advanced stage disease (DFS: hazard ratio [HR] 1.825, 95% confidence interval [CI]: 1.072–3.107; OS: HR 2.441, 95% CI 1.216–4.903) and post-operative chemotherapy omission (DFS: HR 2.529, 95% CI 1.481–4.319; OS: HR 2.666, 95% CI 1.370–5.191) were associated with relatively worse long-term outcomes.
Conclusion
Stent insertion followed by laparoscopy with curative intent is safe and feasible; the addition of post-operative chemotherapy should be considered after successful treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Approximately 30% of patients with colorectal cancer (CRC) may present with obstruction requiring immediate decompression [1]. Self-expanding metallic stent (SEMS) insertion is effective for obstructive bowel decompression in patients with left-sided CRC and is therefore a feasible option for bridging to surgery. When successful deployment is achieved, patients can be treated electively overall and the rate of defunctioning stoma formation is reduced [2,3,4,5].
We previously reported that SEMS insertion followed by elective surgery is oncologically comparable to immediate surgery in patients with obstructive left-sided CRC [5]. However, we did not compare outcomes according to the surgical approach taken (laparoscopy or open surgery) after SEMS insertion.
Laparoscopic surgery is a standard surgical treatment option for patients with CRC owing to its oncological safety and better surgical outcomes than those observed with open surgery, as demonstrated in several cornerstone articles [6,7,8,9]. However, open surgery is still considered the mainstay treatment for those with advanced tumor stage, obstructive bowel dilatation, overt peritonitis, or severe adhesion; in these patients, laparoscopic surgery can be technically challenging or impossible to perform [10]. In addition, although debatable, the oncological safety of laparoscopic surgery is not guaranteed in these situations [11, 12].
Given these findings, this study was designed to compare the oncologic safety of laparoscopic vs open surgery after SEMS insertion in patients with obstructive left-sided CRC. Our hypothesis was that elective laparoscopic radical surgery for the obstructing CRC successfully decompressed with SEMS is non-inferior to open surgery.
Materials and methods
Patients and treatment
Patients who underwent radical resection after successful SEMS deployment for obstructive left-sided (splenic flexure to upper rectum) CRC between July 2002 and December 2011 at five tertiary referral hospitals were retrospectively reviewed. Patients presenting with obstruction from a left-sided CRC were treated with either stenting or emergency surgery, based on the surgeons’ decision. Obstruction was diagnosed based on patients’ symptoms, such as abdominal pain and distension and/or failure to pass gas or feces with/without vomiting, and/or the results of imaging modalities, such as the presence of an obstructing lesion with proximal dilatation observed on computed tomography (CT). After completing a diagnostic workup that included a physical examination, laboratory tests, and radiologic imaging tests, a board-certified colorectal surgeon decided whether to perform SEMS insertion first or proceed to emergency surgery. All SEMS insertion procedures were performed by experienced endoscopists or interventional radiologists, unless there was a sign of perforation, bowel peritonitis, or sepsis. “Successful” SEMS insertion was defined as an early deployment of SEMS followed by clinical resolution of bowel obstruction.
Patients with immediate stenting success were admitted and closely observed for bowel decompression with fasting, parenteral nutritional support, and antibiotics administration, as required. If there were any signs of peritoneal irritation, sepsis, or the worsening of obstructive symptoms after stent deployment, the patient underwent immediate surgery. After a bowel decompression-waiting period that lasted 1–2 weeks, patients underwent elective resection with either laparoscopy or open surgery, as selected by the surgeon, once sufficient bowel decompression was achieved. This decision on surgical approach was mainly based on preference and/or clinical setting rather than any established protocol. Patients with recurrent CRC, synchronous CRC, hereditary CRC, palliative resection, and stage IV disease were all excluded from the cohort. We also excluded patients with more than a 30-day time interval from stenting to surgery, as these patients were likely not intended for curative radical surgery. Adjuvant chemotherapy was recommended based on the final pathologic disease stage for eligible patients. Patients were followed up according to our standard post-operative surveillance protocol, which includes physical examinations; serum carcinoembryonic antigen level testing; radiologic workups, including CT scans of the chest, abdomen, and pelvis; and endoscopic assessment.
Patients were divided into two groups based on the approach used (laparoscopy vs open surgery), and their outcomes were analyzed accordingly. All open conversions were analyzed as the laparoscopy group according to the intention-to-treat principle. All stenting procedures and surgeries were performed by experienced endoscopists, radiologists, and board-certified colorectal surgeons from each participating institution. All participating hospitals were high-volume centers that perform at least 250 laparoscopic colectomies per year. The institutional review boards of the participating hospitals approved this study before the commencement of data collection and waived the requirement for informed consent because of the study’s retrospective design and the minimal risk to the involved patients (IRB No. B-1506/302-119).
Study outcomes
Data on the patients’ baseline demographic characteristics, including age, sex, body mass index (BMI), and American Society of Anesthesiologists (ASA) class were collected. Patient status at admission, including the presence of hypotension, tachycardia, and fever, was noted, and laboratory values including those indicative of leukocytosis as well as albumin and creatinine levels were extracted. Radiologic findings including those on tumor size, location, and the extent of proximal dilatation as well as treatment-related parameters such as the type of operation, laparoscopic or open procedure, stoma formation status, operation duration, expected blood loss, and whether or not adjuvant chemotherapy was delivered were documented.
The primary outcomes were 5-year disease-free survival (DFS) and overall survival (OS). DFS was determined from the date of initial surgery to the date of recurrence detection, last follow-up, or death [13]. Recurrence was determined by radiologic or histologic confirmation. OS was defined from the date of initial surgery to the date of death or last follow-up. The secondary outcomes were short-term surgical outcomes, including the duration of hospital stay, 30-day mortality, and re-operation/re-admission rates.
Propensity score analysis
Owing to the infeasibility of performing a randomized-controlled trial due to the small sample size, inverse probability treatment-weighted (IPTW) propensity score analyses that mimic pseudo-randomized cohorts was used to improve the degree of comparability and to reduce bias due to confounding variables between the laparoscopy and open surgery groups [14]. The IPTW method was used to generate a pseudo-population with well-adjusted covariate combinations between the groups, stabilizing the weights between the subjects without losing subject strength in matching [14, 15]. The covariates for propensity score in relation to the baseline characteristics of the patients were as follows: age, sex, BMI, ASA score, presence of leukocytosis at admission, serum albumin and creatinine levels at admission, extent of proximal dilatation, tumor location, tumor size, and TNM stage.
Statistical analysis
Continuous variables were reported as their means (± standard deviation) or medians (interquartile range [IQR]) for normally or non-normally distributed variables and were compared using the Student’s t-test or Mann–Whitney U-test, respectively. Categorical variables were compared using the Pearson chi-square test or Fisher’s exact test. Analysis of the time-dependent variables was performed using the Kaplan–Meier method, and these were compared using the log-rank test. Univariate and multivariate analyses of the factors affecting survival were conducted using the Cox proportional hazard regression technique. In the multivariable analysis, the stepwise backward elimination technique was used, including variables with an initial P-value of < 0.2 in the univariate analysis and an elimination threshold P-value of 0.1. P-values of < 0.05 were considered indicative of a statistically significant finding. Statistical analyses were performed using SPSS (version 20.0; Chicago, IL) and R (R version 3.5.1; R Core Team, Vienna, Austria).
Results
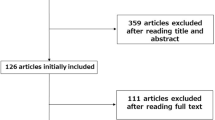
During the study period, a total of 314 cases presented with left-sided colon or upper rectal cancer obstruction. The study flow chart is shown in Fig. 1. SEMS insertion was the first treatment in 207 (65.9%) patients; in 187 (90.3%) patients, the treatment was successful. Among them, elective interval surgeries within 30 days were performed in 179 patients, which comprised the study population. Among them, 97 (54.2%) patients were treated laparoscopically and 82 (45.8%) were treated with open surgery. Nine (9.3%) open conversions were observed in the laparoscopy group: five due to severe adhesions or local invasion of the main tumor, two due to anastomosis instability issues, one due to a narrow pelvis, and one due to CO2 retention during surgery.
Baseline characteristics
The most commonly observed site of obstruction was the sigmoid colon (n = 144, 80.4%) followed by the rectum (n = 15, 8.4%), descending colon (n = 13, 7.3%), and the splenic flexure (n = 7, 3.9%). The patients’ median age was 63.6 (IQR 54.0–64.0) years, and 106 (59.2%) of the patients were male. The median BMI was 22.9 kg/m2 (IQR 20.9–25.0), and 89.9% of the patients had ASA class I/II disease. The median follow-up duration of the cohort was 50.5 months.
Before adjustment, the proportion of patients presenting with tachycardia at admission was lower and the interval from SEMS insertion to surgery was shorter in the laparoscopy than in the open surgery group (Table 1). The other baseline characteristics did differ between the groups, including sex, age, BMI, ASA class, laboratory results, tumor size, location, proximal dilatation, operation type, and stoma formation. After adjustment, these differences were well-rounded.
The laparoscopy group was characterized by longer operation time and lower degree of blood loss (Table 2). This observed difference persisted after adjustment. The pathologic tumor stage was similar between the groups; however, the rate of angiolymphatic invasion and venous invasion was higher in the laparoscopy than in the open surgery group. The perioperative outcomes were similar among the groups, with no cases of 30-day mortality in either group. The proportion of patients receiving adjuvant chemotherapy did not differ between the groups (83.5% vs 74.4%, p = 0.188). The pathological and perioperative findings were well-rounded after adjustment.
Unadjusted and adjusted survival
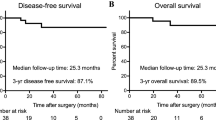
The median follow-up time was 47.3 (IQR 33.7–61.1) months in the laparoscopy group and 52.5 (IQR 35.2–61.0) months in the open surgery group. There were no significant between-group differences in 5-year DFS estimates either before or after adjustment (laparoscopy group vs open surgery group; unadjusted 5-y DFS 68.9% vs 57.1%, p = 0.233; adjusted 5-y DFS 68.7% vs 48.5%, p = 0.230) (Fig. 2).
There were no significant between-group differences in 5-year OS estimates either before or after adjustments (laparoscopy group vs open surgery group; unadjusted 5-y OS 81.6% vs 71.0%, p = 0.206; adjusted 5-y OS 79.1% vs 69.0%, p = 0.200) (Fig. 3).
Factors affecting survival
Factors affecting survival were examined for the entire cohort. In univariate analyses, BMI, bowel dilatation (up to the cecum and small bowel), TNM stage, and adjuvant chemotherapy were identified as significant risk factors affecting DFS (Table 3). Multivariate analyses showed bowel dilatation up to the cecum (hazard ratio [HR] = 3.40, 95% confidence interval [CI]: 1.21–9.56, p = 0.021), advanced tumor stage (HR = 2.65, 95% CI 1.18–5.95, p = 0.018), and the omission of adjuvant chemotherapy (HR = 4.73, 95% CI 2.10–10.6, p < 0.001) to be significant risk factors affecting DFS. Meanwhile, factors affecting OS in univariate analyses included BMI, bowel dilatation, TNM stage, and adjuvant chemotherapy (Table 4). Multivariate analyses showed bowel dilatation up to the cecum (HR = 3.40, 95% CI 1.21–9.56, p = 0.021), advanced tumor stage (HR = 2.65, 95% CI 1.18–5.95, p = 0.018), and the omission of adjuvant chemotherapy (HR = 4.73, 95% CI 2.10–10.6, p < 0.001) to be significant risk factors affecting OS.
Discussion
In this study, there was no difference in DFS or OS outcomes according to the surgical approach even after adjusting for confounding variables in patients undergoing elective surgery with curative intent for left-sided obstructive CRC, following successful SEMS insertion. In addition, post-operative short-term outcomes were comparable in both groups. To the best of our knowledge, this is the largest study to compare the long-term oncologic outcomes associated with laparoscopy and open surgery after SEMS insertion in patients with left-sided obstructive CRC, and the first to apply propensity score adjustment using IPTW analysis. Since conducting a randomized study according to the treatment method may not be feasible in this context, or may require a long recruitment period, owing to the rarity of the disease, the enrollment of a pseudo-randomized cohort might be the best method for the evaluation of this outcome.
SEMS insertion followed by surgical resection is an attractive treatment option for obstructive left-sided CRC. Successful SEMS insertion followed by primary resection enables one-stage elective surgery and extends the time available for thorough preoperative evaluation, thereby enhancing the patient’s fitness for surgery. Previous studies have shown the feasibility and oncologic safety of SEMS insertion [1,2,3,4,5], since it can provide a bridge to surgery in select cases, according to the National Comprehensive Cancer Network for obstructive CRC [16]. However, further treatment options in terms of minimally invasive approaches are not well established, in particular, after successful SEMS deployment and bowel decompression [17]. Previous studies have shown that the laparoscopic approach is feasible and safe in terms of short-term outcomes [18,19,20,21]. Although these previous studies presented encouraging results, they were limited by their retrospective nature and small sample size. A recent retrospective study showed that the laparoscopic approach was comparable to open surgery in terms of long-term oncologic results, with a relatively large treatment cohort [22]. In that study, a total of 94 patients (50 open surgery, 44 laparoscopy) were recruited from 4 tertiary hospitals over an 8-year period, and the resulting 5-year DFS (55.8% open vs 61.5% laparoscopic; p = 0.955) and OS (67.1% open vs 71.7% laparoscopic; p = 0.942) values were similar in both groups. Although the study was not adjusted for disease severity or confounding variables, the cohort was similar in terms of baseline characteristics, making these findings promising.
In the present study, adjuvant chemotherapy was the only factor associated with both DFS and OS. This is in line with the results of previous studies in which adjuvant chemotherapy was beneficial to patients with stage II disease and factors considered high-risk as well as in cases of stage III CRC [22,23,24,25]. These findings suggest that adjuvant chemotherapy should be recommended to all patients with obstructive CRC, regardless of tumor stage, even after adequate bowel decompression from SEMS.
These findings notwithstanding, successful SEMS deployment has been associated with pathologic or systemic features that may decrease DFS [26,27,28]. In our previous study, patients receiving SEMS showed a higher proportion of lymphatic and perineural invasion than did those receiving emergency surgery [5]. However, this did not translate to differences in survival outcomes. In fact, in the present study, the presence of a higher proportion of lymphatic and venous invasion in patients receiving laparoscopic surgery than in those receiving open surgery did not affect DFS or OS estimates. The biologic effect exerted by the mechanical stress of SEMS insertion on tumors remains unclear, with some studies suggesting that SEMS insertion may suppress cancer proliferation [29]. While the similar DFS- and OS-related outcomes in both groups may have been due to the higher proportion of patients receiving adjuvant chemotherapy in the laparoscopy group, after adjustments to control for this difference, the DFS and OS estimates remained similar.
This study has several limitations. The main limitation is its retrospective and non-randomized design. However, to decrease the degree of confounding bias and to mimic a randomized-controlled design, we performed PS matching analysis with the IPTW method. Second, there was no objective criterion for determining the surgical approach (either laparoscopic or open surgery), which was solely at the surgeon’s discretion, and may have led to selection bias. However, all the surgeries were performed by colorectal surgery specialists, many of whom are participants of a major clinical trial focusing on the comparison of laparoscopic vs open surgery [7, 8]. Third, the relatively small sample size and consequently poor statistical power may impede generalizability of the present findings. However, to date, the present study is among the largest (if not the largest) studies to compare the long-term oncologic outcomes associated with laparoscopic and open surgery following SEMS insertion in patients with left-sided CRC obstruction. Further studies in future should aim for greater statistical power when attempting to validate the present findings.
In conclusion, laparoscopic surgery after SEMS insertion with curative intent for left-sided CRC obstruction showed long-term outcomes comparable to those associated with open surgery. Post-operative chemotherapy should be considered for this patient group after successful treatment. Further large-scale, well-designed studies are warranted to reach a more confirmative conclusion.
References
Mangano A, Motson RW (2016) Evidence-based analysis of self-expanding metallic stent as a bridge to surgery versus emergency surgery for colon cancer. Future Oncol 12:1957–1960
Tan CJ, Dasari BVM, Gardiner K (2012) Systematic review and meta-analysis of randomized clinical trials of self-expanding metallic stents as a bridge to surgery versus emergency surgery for malignant left-sided large bowel obstruction. Br J Surg 99:469–476
van Hooft JE, Bemelman WA, Oldenburg B, Marinelli AW, Lutke Holzik MF, Grubben MJ, Sprangers MA, Dijkgraaf MG, Fockens P, Collaborative Dutch Stent-In Study G (2011) Colonic stenting versus emergency surgery for acute left-sided malignant colonic obstruction: a multicentre randomised trial. Lancet Oncol 12:344–352
Amelung FJ, Borstlap WAA, Consten ECJ, Veld JV, van Halsema EE, Bemelman WA, Siersema PD, Ter Borg F, van Hooft JE, Tanis PJ, Dutch Snapshot Research G (2019) Propensity score-matched analysis of oncological outcome between stent as bridge to surgery and emergency resection in patients with malignant left-sided colonic obstruction. Br J Surg 106:1075–1086
Kang SI, Oh H-K, Yoo JS, Ahn S, Kim MH, Kim MJ, Son IT, Kim D-W, Kang S-B, Park YS, Yoon CJ, Shin R, Heo SC, Lee IT, Youk EG, Kim MJ, Chang TY, Park S-C, Sohn DK, Oh JH, Park JW, Ryoo S-B, Jeong S-Y, Park KJ (2018) Oncologic outcomes of preoperative stent insertion first versus immediate surgery for obstructing left-sided colorectal cancer. Surg Oncol 27:216–224
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy AM, Group COcLoORS (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477-484
Kang SB, Park JW, Jeong SY, Nam BH, Choi HS, Kim DW, Lim SB, Lee TG, Kim DY, Kim JS, Chang HJ, Lee HS, Kim SY, Jung KH, Hong YS, Kim JH, Sohn DK, Kim DH, Oh JH (2010) Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol 11:637–645
Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB, Choi HS, Kim DW, Chang HJ, Kim DY, Jung KH, Kim TY, Kang GH, Chie EK, Kim SY, Sohn DK, Kim DH, Kim JS, Lee HS, Kim JH, Oh JH (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15:767–774
Colon Cancer Laparoscopic or Open Resection Study G, Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy A, Bonjer HJ (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10:44–52
Newman CM, Arnold SJ, Coull DB, Linn TY, Moran BJ, Gudgeon AM, Cecil TD (2012) The majority of colorectal resections require an open approach, even in units with a special interest in laparoscopic surgery. Colorectal Dis 14:29–34
Allaix ME, Furnee EJ, Mistrangelo M, Arezzo A, Morino M (2016) Conversion of laparoscopic colorectal resection for cancer: What is the impact on short-term outcomes and survival? World J Gastroenterol 22:8304–8313
Scheidbach H, Garlipp B, Oberlander H, Adolf D, Kockerling F, Lippert H (2011) Conversion in laparoscopic colorectal cancer surgery: impact on short- and long-term outcome. J Laparoendosc Adv Surg Tech A 21:923–927
Punt CJ, Buyse M, Kohne CH, Hohenberger P, Labianca R, Schmoll HJ, Pahlman L, Sobrero A, Douillard JY (2007) Endpoints in adjuvant treatment trials: a systematic review of the literature in colon cancer and proposed definitions for future trials. J Natl Cancer Inst 99:998–1003
Heinze G, Juni P (2011) An overview of the objectives of and the approaches to propensity score analyses. Eur Heart J 32:1704–1708
Cole SR, Hernan MA (2004) Adjusted survival curves with inverse probability weights. Comput Methods Programs Biomed 75:45–49
National Comprehensive Cancer Network (2019) NCCN Guidelines Colon Cancer (version 2. 2019). http://www.nccn.org/. Accessed 5 Aug 2019
van Hooft JE, Veld JV, Arnold D, Beets-Tan RGH, Everett S, Gotz M, van Halsema EE, Hill J, Manes G, Meisner S, Rodrigues-Pinto E, Sabbagh C, Vandervoort J, Tanis PJ, Vanbiervliet G, Arezzo A (2020) Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline—Update 2020. Endoscopy 52:389–407
Chung TS, Lim SB, Sohn DK, Hong CW, Han KS, Choi HS, Jeong SY (2008) Feasibility of single-stage laparoscopic resection after placement of a self-expandable metallic stent for obstructive left colorectal cancer. World J Surg 32:2275–2280
Shimizu H, Yamazaki R, Ohtsuka H, Osaka I, Takuma K, Morita Y (2018) Feasibility of laparoscopic surgery after stent insertion for obstructive colorectal cancer. Asian Journal of Endoscopic Surgery 11:118–122
Enomoto T, Saida Y, Takabayashi K, Nagao S, Takeshita E, Watanabe R, Takahashi A, Nakamura Y, Asai K, Watanebe M, Nagao J, Kusachi S (2016) Open surgery versus laparoscopic surgery after stent insertion for obstructive colorectal cancer. Surg Today 46:1383–1386
Rho SY, Bae SU, Baek SJ, Hur H, Min BS, Baik SH, Lee KY, Kim NK (2013) Feasibility and safety of laparoscopic resection following stent insertion for obstructing left-sided colon cancer. Journal of the Korean Surgical Society 85:290–295
Bae SU, Yang CS, Kim S, Lim DR, Jeong WK, Dong Kim D, Kim JH, Shin EJ, Lee YJ, Lee JY, Kim NK, Baek SK (2019) Long-term oncologic outcomes of laparoscopic versus open resection following stent insertion for obstructing colon cancer: a multi-center retrospective study. Surg Endosc 33:3937–3944
Meyers BM, Cosby R, Quereshy F, Jonker D (2017) Adjuvant Chemotherapy for Stage II and III Colon Cancer Following Complete Resection: A Cancer Care Ontario Systematic Review. Clin Oncol (R Coll Radiol) 29:459–465
Labianca R, Nordlinger B, Beretta GD, Mosconi S, Mandala M, Cervantes A, Arnold D, Group EGW (2013) Early colon cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 24 Suppl 6: vi64–72
Figueredo A, Coombes ME, Mukherjee S (2008) Adjuvant therapy for completely resected stage II colon cancer. Cochrane Database Syst Rev 16:CD005390.
Kim HJ, Choi GS, Park JS, Park SY, Jun SH (2013) Higher rate of perineural invasion in stent-laparoscopic approach in comparison to emergent open resection for obstructing left-sided colon cancer. Int J Colorectal Dis 28:407–414
Yamashita S, Tanemura M, Sawada G, Moon J, Shimizu Y, Yamaguchi T, Kuwai T, Urata Y, Kuraoka K, Hatanaka N, Yamashita Y, Taniyama K (2018) Impact of endoscopic stent insertion on detection of viable circulating tumor cells from obstructive colorectal cancer. Oncol Lett 15:400–406
Maruthachalam K, Lash GE, Shenton BK, Horgan AF (2007) Tumor cell dissemination following endoscopic stent insertion. Br J Surg 94:1151–1154
Matsuda A, Miyashita M, Matsumoto S, Sakurazawa N, Kawano Y, Yamahatsu K, Sekiguchi K, Yamada M, Hatori T, Yoshida H (2018) Colonic stent-induced mechanical compression may suppress cancer cell proliferation in malignant large bowel obstruction. Surg Endosc 33:1290–1297
Acknowledgements
An abstract version of this article was presented at the 13th Scientific and Annual Meeting of European Society of Coloproctology 2018. None of the authors have commercial associations (e.g., consultancies, stock ownership, equity interests, patent-licensing arrangements, research support, speaking fees) that may pose a conflict of interest in connection with this study. We would like to thank Editage (www.editage.co.kr) for English language editing.
Funding
This work was supported by a Grant (No. 02-2018-036) from the SNUBH Research Fund.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Disclosures
Drs. Min Hyun Kim, Sung Il Kang, Jeehye Lee, Heung-Kwon Oh, Soyeon Ahn, Duck-Woo Kim, Sung-Bum Kang, Rumi Shin, Seung Chul Heo, Eui Gon Youk, Sung-Chan Park, Dae Kyung Sohn, Jae Hwan Oh, Min Jung Kim, Ji Won Park, Seung-Bum Ryoo, Seung-Yong Jeong, and Kyu Joo Park have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, M.H., Kang, S.I., Lee, J. et al. Oncologic safety of laparoscopic surgery after metallic stent insertion for obstructive left-sided colorectal cancer: a multicenter comparative study. Surg Endosc 36, 385–395 (2022). https://doi.org/10.1007/s00464-021-08293-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08293-5