Abstract
Background
A bridge to surgery (BTS) after self-expandable metallic stent (SEMS) placement is a widely recognized treatment strategy for obstructive colorectal cancer. However, there is still a lack of evidence for the efficacy and safety of laparoscopic surgery following SEMS placement. The aim of this systematic review and meta-analysis was to compare the short-term and long-term outcomes of laparoscopic surgery with those of open surgery following SEMS placement in patients with obstructive colorectal cancer.
Methods
An electronic literature search through to December 2022 was performed to identify studies comparing short-term and long-term outcomes between laparoscopic and open surgery following SEMS placement for obstructive colorectal cancer. The main outcome measures were postoperative complication rates and mortality. Secondary outcome measures were the 3-year recurrence-free survival (RFS) and 3-year overall survival (OS) rates. The meta-analysis was performed using fixed-effect or random-effects methods to calculate odds ratios (ORs) with 95% confidence intervals (95% CIs).
Results
The meta-analysis included 15 studies and 883 patients, of whom 467 (52.9%) underwent laparoscopic surgery and 416 (47.1%) underwent open surgery following SEMS placement. The postoperative complication rate was significantly lower in the laparoscopic surgery group than in the open surgery group (OR 0.47, 95% CI 0.32–0.67, P < 0.001). There was no significant difference in the 3-year RFS rate or 3-year OS rate between the laparoscopic and open surgery groups (3-year RFS, OR 0.78, 95% CI 0.50–1.24, P = 0.30; 3-year OS, OR 0.68, 95% CI 0.41–1.12, P = 0.13).
Conclusion
This meta-analysis found that the short-term outcome was better in patients who underwent laparoscopic surgery following SEMS placement than in those who underwent open surgery. Furthermore, there was no significant difference in long-term outcomes between the two groups. Laparoscopic surgery following SEMS placement may be a safe and effective treatment option for obstructive colorectal cancer.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Approximately 8–34% of patients with colorectal cancer have obstructive symptoms [1,2,3]. Obstructive colorectal cancer (OCRC) is considered a life-threatening condition that requires immediate intervention. However, emergency one-stage resection for OCRC is associated with significantly higher mortality and morbidity rates than elective surgery [4, 5]. In the last two decades, elective surgery following self-expandable metallic stent (SEMS) placement, known as a bridge to surgery (BTS), has been introduced and is widely accepted as an alternative treatment strategy to emergency surgery [6,7,8,9,10,11,12,13]. BTS for OCRC is now recommended in the 2020 European Society of Gastrointestinal Endoscopy guidelines [14]. Although the usefulness and safety of laparoscopic surgery is well established in patients with colorectal cancer [15,16,17,18], there have been no comprehensive studies in OCRC. Recent retrospective cohort studies have demonstrated better results for laparoscopic surgery than for open surgery following SEMS placement [7, 19,20,21,22,23,24,25,26,27,28,29,30,31,32]. However, it is quite difficult to perform randomized controlled trials (RCTs) with large enough sample sizes to reach a conclusion, partly because of the rarity of OCRC. Therefore, we performed this systematic review and meta-analysis of the relevant published studies, which included a total of 883 patients, to determine the efficacy and safety of laparoscopic surgery following SEMS placement for OCRC.
Methods
The meta-analysis was performed in accordance with the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [33].
Literature retrieval and study selection
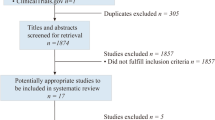
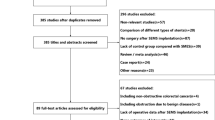
The literature in the MEDLINE (PubMed), Google Scholar, and Cochrane Library databases was systematically searched through to December 2022 to identify relevant studies (Fig. 1). The search was limited to human studies published in English or Japanese. The search terms used were (“colon cancer” OR “colonic obstruction” OR “malignant obstruction”) AND (“laparoscopic surgery” OR “minimally invasive surgery” OR “open surgery” OR “laparotomy”) AND (“stent” OR “endoscopic decompression”). The related articles function was used to broaden the search. The reference lists of all relevant publications were searched manually for additional studies that may have been initially overlooked using our search strategy. The quality of the included studies was assessed using the Newcastle–Ottawa scale (NOS) for observational studies [34]. Studies were considered to be of high quality if they had an NOS score of ≥ 7. The MINORS (Methodological Index for Non-Randomized Studies) tool was used to assess the risk of bias for individual studies [35]. GRADE (Grading of Recommendations Assessment, Development and Evaluation) methodology was used to assess the quality of evidence and reported in the results with the help of GRADE Pro software (McMaster University and Evidence Prime Inc., Ontario, CA; https://www.gradepro.org/) [36].
Inclusion and exclusion criteria
The inclusion and exclusion criteria were defined a priori. Studies were included if they compared postoperative complications between patients with acute OCRC who underwent laparoscopic surgery and those who underwent open surgery following SEMS placement. Surgery was defined as primary tumor resection with or without primary anastomosis. Duplicated study reports and studies for which predefined outcomes were not reported or it was impossible to extract the number of outcome events were excluded.
Extraction of data
The full-text version of each eligible study was evaluated by two investigators (S.K., A.M.) working independently. The following data were extracted: name of the primary author, year of publication, country in which the study was performed, number of participating institutions, design and duration of the study, number of study participants and their characteristics, including age, sex, and tumor-related variables, interval between SEMS placement and surgery, and all available information on short-term and long-term outcomes.
Data synthesis and statistical analysis
Short-term outcomes (primary anastomosis, stoma construction, overall morbidity, surgical site infection, anastomotic leakage, and postoperative ileus) and long-term outcomes (3-year recurrence-free survival [RFS] and 3-year overall survival [OS]) were compared between patients who underwent laparoscopic surgery (the LS group) and those who underwent open surgery (the OpS group). Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. An OR of < 1 favored the BTS group, and the point estimate of the OR was considered statistically significant at P < 0.05 if the 95% CI did not include the value 1. The pooled OR was calculated using a Mantel–Haenszel fixed-effect model or a DerSimonian–Laird random-effects model to combine ORs for outcomes of interest. The meta-analysis was performed using Review Manager (Version 5.1) for Windows (Nordic Cochrane Center, Cochrane Collaboration, Copenhagen, Denmark; http://www.cc-ims.net/RevMan). The Cochran’s chi-square-based Q statistic test was used to assess between-study heterogeneity. The I2 value was used to test for heterogeneity among the included studies. Study heterogeneity was measured using the χ2 and I2 statistics, with a χ2 P value of < 0.05 and an I2 value of ≥ 50% indicating heterogeneity [37]. A fixed-effect model was used to estimate the overall effect if the OR was homogeneous; if the OR was not homogeneous, a random-effects model was used [38]. Publication bias was assessed by visual examination and statistical analysis of a funnel plot, with asymmetry formally assessed by use of Egger’s linear regression test and the rank correlation (Begg’s) test using WINPEPI software (available at http://www.brixtonhealth.com/pepi4windows.html) [39, 40].
Results
Literature review and included studies
In total, 485 potentially relevant citations were identified during the initial screening. After reviewing the titles and abstracts, 359 studies were excluded. One hundred and eleven further studies were excluded after full-text evaluation, leaving 15 studies published between 2004 and 2022 [7, 19,20,21,22,23,24,25,26,27,28,29,30,31,32] for inclusion in the meta-analysis (Fig. 1). The background characteristics of the included studies are shown in Table 1. Three studies [19,20,21] originated from Europe and 12 [7, 22,23,24,25,26,27,28,29,30,31,32] from Asia. All the studies had a retrospective observational design. In total, 467 (52.9%) of the 883 patients included in the meta-analysis underwent laparoscopic surgery and 416 (47.1%) underwent open surgery. The risk of bias was assessed independently using the NOS score (Table 2). The NOS score was ≤ 6 in three studies [19, 20, 24] and ≥ 7 in 12 [7, 21,22,23, 25,26,27,28,29,30,31,32]. The included studies had a mean MINORS score (± standard deviation) of 12.93 ± 4.15, indicating that the quality of evidence for non-randomized studies was fair. The MINORS results for the included studies are shown in Table 3. According to the GRADE criteria, the overall quality of evidence was very low for ileus, stoma construction, and primary anastomosis, low for mortality, anastomotic leak, wound infection, and 3-year OS and RFS, and moderate for postoperative complications (Table 4).
Short-term outcomes
Postoperative complications
All 15 studies reported postoperative complications. Only four studies [7, 19, 31, 32] reported the severity of these complications and eight [7, 19, 23, 25, 29,30,31,32] reported postoperative complications occurring within 30 days after surgery. Therefore, postoperative complications were defined as the overall morbidities listed in the included studies [7, 19,20,21,22,23,24,25,26,27,28,29,30,31,32]. The postoperative complication rate was 13.3% (62/467) in the LS group and 23.8% (99/416) in the OpS group. The heterogeneity test indicated a χ2 value of 19.06 and an I2 value of 27%, demonstrating homogeneity. Therefore, a fixed-effect model was adopted (OR 0.47, 95% CI 0.32–0.67, P < 0.001) (Fig. 2). This meta-analysis demonstrated that laparoscopic surgery contributed to a significant reduction in postoperative complications compared to open surgery. We found no significant publication bias by visual inspection of the funnel plot (Supplementary Fig. 1) or on Egger’s test (P = 0.772) or Begg’s test (P = 0.255).
Mortality
Mortality was reported in eleven studies. The postoperative mortality rates in the LS and OpS groups were 0.5% (2/408) and 0.3% (1/329), respectively. The heterogeneity test indicated a χ2 value of 0.63 and an I2 value of 0%, indicating homogeneity. Therefore, the fixed-effect model was adopted (OR 1.01, 95% CI 0.18–5.55, P = 0.99) (Fig. 3). There was no significant difference in mortality between the two groups. We found no significant publication bias during visual inspection of the funnel plot (Supplementary Fig. 2) or on Egger’s test (P = 0.975) or Begg’s test (P = 0.602).
Other outcomes
The surgical outcomes are shown in Table 5 and in Supplementary Figs. 3, 4, and 5. The operation time was shorter in the OpS group than in the LS group, and the postoperative hospital stay was shorter in the LS group than in the OpS group. The between-group differences in both outcomes were statistically significant (P < 0.01).
The other short-term outcomes are shown in Table 6 and in Supplementary Figs. 6, 7, 8, 9, and 10. The primary anastomosis rate was favored the LS group over OpS group (97.9% [190/194] vs. 91.2% [145/159]) and as was the stoma construction rate (5.5% [10/182] vs. 15.1% [24/159]). The between-group differences for both these outcomes were statistically significant (OR 0.23, 95% CI 0.08–0.66, P = 0.006 for primary anastomosis; OR 0.28, 95% CI 0.13–0.62, P = 0.002 for stoma construction) and without between-study heterogeneity (χ2 = 1.86, I2 = 0%, P = 0.87 and χ2 = 2.90, I2 = 0%, P = 0.41, respectively).
Postoperative anastomotic leakage, wound infection, and ileus were analyzed. The meta-analyses of wound infection demonstrated significantly favorable results in the LS group over OpS group (OR 0.42, 95% CI 0.21–0.84, P = 0.02) without between-study heterogeneity (χ2 = 3.51, I2 = 0%, P = 0.94, respectively). There was no significant between-group difference in the anastomotic leak rate (OR 0.67, 95% CI 0.31–1.45, P = 0.31) or in the frequency of ileus (OR 0.64, 95% CI 0.34–1.21, P = 0.17 for ileus). There was no between-study heterogeneity (χ2 = 2.18, I2 = 0%, P = 0.98, and χ2 = 7.26, I2 = 0%, P = 0.61, respectively).
Long-term outcomes
The long-term outcomes are demonstrated in Figs. 4 and 5. Four studies [23, 30,31,32] reported the 3-year RFS rate and six [20, 23, 29,30,31,32] reported the 3-year OS rate. Data on 3-year RFS were available for 381 patients and data on 3-year OS for 486 patients. There was no significant difference in 3-year RFS (OR 0.78, 95% CI 0.50–1.24, P = 0.30) or 3-year OS (OR 0.68, 95% CI 0.41–1.12, P = 0.13) between the LS and OpS groups or any between-study heterogeneity (χ2 = 1.67, I2 = 0%, P = 0.30 and χ2 = 1.08, I2 = 0%, P = 0.90, respectively). We found no significant publication bias in terms of either outcome by visual inspection of the funnel plot (Supplementary Figs. 11 and 12) or on Egger’s test (P = 0.509) or Begg’s test (P = 1.00) and Egger’s test (P = 0.299) or Begg’s test (P = 0.142).
Discussion
This meta-analysis was performed to obtain an overview of the recent literature on the outcomes of laparoscopic surgery following SEMS placement for OCRC. Although several retrospective studies of laparoscopic surgery following SEMS placement have been published, there have been no RCTs to date, possibly because of the rarity of OCRC, the urgent situation at the time of initial diagnosis, and the oncological safety of BTS itself not having been established [41, 42]. Based on our present findings, an RCT comparing short-term and long-term outcomes between laparoscopic surgery and open surgery following SEMS placement for OCRC would be expected to have a 3-year RFS rate of 30% for open surgery and 20% for laparoscopic surgery. Therefore, a sample size of at least 260 would be required in each group for a statistical power of 80% and a significance level of 0.05 [15, 16]. It would be very difficult to collect such a large number of cases for an RCT. This systematic review and meta-analysis was performed to determine if laparoscopic surgery following SEMS placement is safe and effective for OCRC and drew on as much evidence as possible from previous reports in a sample of adequate size (n = 883).
Large-scale RCTs in patients with colon cancer have established that laparoscopic surgery decreases surgical trauma and perioperative complications, allows more rapid recovery, and has a non-inferior oncological prognosis [15,16,17,18]. However, in patients with OCRC, laparoscopic surgery following SEMS placement may be contraindicated because of the limited surgical field as a result of the distended bowel and the peculiarities of tumor size and depth. Morino et al. [13] were the first to describe use of the laparoscopic approach following SEMS placement for OCRC and concluded that the colonic segment was bulkier and more technically difficult to resect by laparoscopy. Thirteen of the studies in this meta-analysis [7, 19, 21,22,23,24,25,26,27, 29,30,31,32] compared baseline characteristics between an LS group and an OpS group. Although only one of the studies reported a significantly higher proportion of men in its LS group [25], there was no significant difference in background characteristics. Twelve studies analyzed data on pathological stage and found no significant between-group difference [7, 20,21,22,23, 25,26,27, 29,30,31,32]. However, one study excluded patients with suspected invasion of other organs from its LS group [26] and another study reported a significantly greater number of patients with pathological T4b disease in its OpS group [31]. Therefore, differences in patient characteristics in the individual studies would not be expected to have much statistical impact on our results.
Many large-scale trials have demonstrated the feasibility and safety of laparoscopic colorectal surgery, particularly a reduction in postoperative complications [15,16,17,18, 43, 44]. Our present meta-analysis found that the risk of postoperative complications was significantly lower in patients who underwent laparoscopic surgery than in those who underwent open surgery (OR 0.47, 95% CI 0.32–0.67, P < 0.001) after BTS for OCRC. Postoperative complications have been widely reported to have a negative oncological impact after digestive cancer surgery [45,46,47,48], and the same finding has been reported for colorectal cancer surgery. Several explanations for this finding have been suggested, including local and systemic activation of proinflammatory cytokines and mediators, delayed or canceled adjuvant chemotherapy, and abdominal implantation of intraluminal cancer cells in patients with anastomotic leakage [49,50,51,52,53]. A significant correlation of postoperative complications with a worse prognosis was also reported in a BTS cohort [54]. Therefore, efforts to minimize postoperative complications are important in BTS for OCRC and choice of laparoscopic surgery may be useful.
This study had several limitations. First, as with all systematic reviews, the strength of our conclusions depends on the quality of the primary studies. Unfortunately, the design and quality of the studies included in this review were not high. Furthermore, no relevant RCTs or prospective studies were available for analysis. RCTs investigating the safety and usefulness of the BTS strategy with an adequate sample size are difficult to perform because of (1) lack of evidence for its use (an RCT is currently underway in Japan) and (2) the fact that a proportion of patients with OCRC have metastasis to other organs, which makes laparoscopic surgery difficult and inevitably introduces significant bias stemming from the surgeon’s level of skill and judgment. Second, there was heterogeneity between studies because of differences in sample size, pathological staging, study design, and follow-up. There was also heterogeneity in the definitions of morbidity and mortality. Moreover, there was considerable heterogeneity in long-term outcomes in terms of pathological staging and postoperative adjuvant therapy. This heterogeneity had a marked effect on our results.
In conclusion, laparoscopic surgery following placement of a SEMS for OCRC significantly reduces the postoperative complication rate. Furthermore, there were no significant differences in long-term outcomes between the two procedures. Our findings suggest that laparoscopic surgery following SEMS placement is a safe and effective treatment option for OCRC.
Disclosures
Shintaro Kanaka, Takeshi Yamada, Akihisa Matsuda, Kay Uehara, Seiichi Shinji, Yasuyuki Yokoyama, Goro Takahashi, Takuma Iwai, Kohki Takeda, Sho Kuriyama, Toshimitsu Miyasaka, and Hiroshi Yoshida have no conflicts of interest or financial ties to disclose.
References
Carraro PGS, Segala M, Cesana BM, Tiberio G (2001) Obstructing colonic cancer: failure and survival patterns over a 10 year follow up after one stage curative surgery. Dis Colon Rectum 44:243–250
De Salvo GL, Gava C, Pucciarelli M (2004) Curative surgery for obstruction from primary left colorectal carcinoma: primary or staged resection? Cochran Database Syst Rev. https://doi.org/10.1002/14651858.CD002101
Manceau G, Voron T, Mege D, Bridoux V, Lakkis Z, Venara A, Beyer-Berjot L, Abdalla S, Sieleznef I, Lefèvre JH, Karoui M, AFC (French Surgical Association) Working Group (2019) Prognostic factors and patterns of recurrence after emergency management for obstructing colon cancer: multivariate analysis from a series of 2120 patients. Langenbecks Arch Surg 404:717–729
Saida Y, Sumiyama Y, Nagao J, Uramatsu M (2003) Long-term prognosis of preoperative “bridge to surgery” expandable metallic stent insertion for obstructive colorectal cancer: comparison with emergency operation. Dis Colon Rectum 46(10 Suppl):S44–S49
Amelung FJ, Draaisma A, Consten ECJ, Siersema PD, ter Borg F (2017) Self-expandable metal stent placement versus emergency resection for malignant proximal colon obstructions. Surg Endosc 31:4532–4541
Dohmoto M, Rupp KD, Hohlbach G (1990) Endoscopicallyimplanted prosthesis in rectal carcinoma. Dtsch Med Wochenschr 115:915
Yang SY, Park YY, Han YD, Cho MS, Hur H, Min BS, Lee KY, Kim NK (2019) Oncologic outcomes of self-expandable metallic stent as a bridge to surgery and safety and feasibility of minimally invasive surgery for acute malignant colonic obstruction. Ann Surg Oncol 26:2787–2796
Matsuda A, Miyashita M, Matsumoto S, Matsutani T, Sakurazawa N, Takahashi G, Kishi T, Uchida E (2015) Comparison of long-term outcomes of colonic stent as “bridge to surgery” and emergency surgery for malignant large-bowel obstruction: a meta-analysis. Ann Surg Oncol 22:497–504
Allievi N, Ceresoli M, Fugazzola P, Montori G, Coccolini F, Ansaloni L (2017) Endoscopic stenting as bridge to surgery versus emergency resection for left-sided malignant colorectal obstruction: an updated meta-analysis. Int J Surg Oncol. https://doi.org/10.1155/2017/2863272
Erichsen R, Horváth-Puhó E, Jacobsen JB, Nilsson T, Baron JA, Sørensen HT (2015) Long-term mortality and recurrence after colorectal cancer surgery with preoperative stenting: a Danish nationwide cohort study. Endoscopy 47:517–524
Cwikiel W, Andrén-Sandberg A (1993) Malignant stricture with colovesical fistula: stent insertion in the colon. Radiology 186:563–564
Kye B-H, Kim J-H, Kim H-J, Lee YS, Lee I-K, Kang WK, Cho H-M, Ahn C-H, Seong-Taek Oh (2020) The optimal time interval between the placement of self-expandable metallic stent and elective surgery in patients with obstructive colon cancer. Sci Rep 10:9502
Morino M, Bertello A, Garbarini A, Rozzio G, Repici A (2002) Malignant colonic obstruction managed by endoscopic stent decompression followed by laparoscopic resections. Surg Endosc 16:1483–1487
van Hooft JE, Veld JV, Arnold D, Beets-Tan RGH, Everett S, Götz M, van Halsema EE, Hill J, Manes G, Meisner S, Rodrigues-Pinto E, Sabbagh C, Vandervoort J, Tanis PJ, Vanbiervliet G, Arezzo A (2020) Self-expandable metal stents for obstructing colonic and extracolonic cancer: European society of gastrointestinal endoscopy (ESGE) guideline-update 2020. Endoscopy 52:389–407
Lacy AM, García-Valdecasas JC, Delgado S, Castells A, Taurá P, Piqué JM, Visa J (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet 359:2224–2229
Leung KL, Kwok SPY, Lam SCW, Lee JFY, You RYC, Ng SSM, Lai PBS, Lau WY (2004) Laparoscopic resection of rectosigmoid carcinoma: prospective randomised trial. Lancet 363:1187–1192
Weeks JC, Nelson H, Gelber S, Sargent D, Schroeder G, Clinical Outcomes of Surgical Therapy (COST) Study Group (2002) Short-term quality-of-life outcomes following laparoscopic-assisted colectomy vs open colectomy for colon cancer: a randomized trial. JAMA 287:321–328
Kitano S, Inomata M, Sato A, Yoshimura K, Moriya Y, for the Colorectal Cancer Study Group (CCSG) of Japan Clinical Oncology Group (2005) Randomized controlled trial to evaluate laparoscopic surgery for colorectal cancer: Japan Clinical Oncology Group Study JCOG 0404. Jpn J Clin Oncol 35:475–477
Balagué C, Targarona EM, Sainz S, Montero O, Bendahat G, Kobus C, Garriga J, Gonzalez D, Pujol J, Trias M (2004) Minimally invasive treatment for obstructive tumors of the left colon: endoluminal self-expanding metal stent and laparoscopic colectomy. Preliminary results Dig Surg 21:282–286
Olmi S, Scaini A, Cesana G, Dinelli M, Lomazzi A, Croce E (2007) Acute colonic obstruction: endoscopic stenting and laparoscopic resection. Surg Endosc 21:2100–2104
Stipa F, Pigazzi A, Bascone B, Cimitan A, Villotti G, Burza A, Vitale A (2008) Management of obstructive colorectal cancer with endoscopic stenting followed by single-stage surgery: open or laparoscopic resection? Surg Endosc 22:1477–1481
Chung TS, Lim SB, Sohn DK, Hong CW, Han KS, Choi HS, Jeong SY (2008) Feasibility of single-stage laparoscopic resection after placement of a self-expandable metallic stent for obstructive left colorectal cancer. World J Surg 32:2275–2280
Zhou JM, Yao LQ, Xu JM, Xu MD, Zhou PH, Chen WF, Shi Q, Ren Z, Chen T, Zhong YS (2013) Self-expandable metallic stent placement plus laparoscopy for acute malignant colorectal obstruction. World J Gastroenterol 19:5513–5519
Watanabe T, Ike H, Mikayama Y, Tsuchida K, Mushiake H, Hasegawa S, Fukushima T, Kyo R, Tokoro C, Hishiki S, Kawana I, Rino Y, Masuda M, Imada T (2014) Outcomes of laparoscopic surgery after preoperative metallic stent placement for obstructive colorectal cancer (in Japanese). Gan To Kagaku Ryoho 41:1482–1484
Tanaka T, Yoshida S, Nishikawa T, Tanaka J, Kiyomatsu T, Hata K, Kawai K, Nozawa H, Kazama S, Narita A, Sasaki T, Yamaguchi H, Ishihara S, Sunami E, Isayama H, Koike K, Watanabe T (2014) Self-expandable metal stent placement as a bridge to laparoscopic or open surgery for obstructive colorectal cancer: short-term outcomes of nineteen consecutive cases. Gastroenterol Hepatol 1:20–25
Shimada M, Lee K, Oka H, Takayama S, Kanazawa A, Ueno G, Ichikawa Y, Hagi T, Ishikawa S (2015) Treatment outcomes of preoperative self-expandable metalic stent (SEMS) placement as a bridge to laparosopic-assisted surgery (BTLS) for obstructive colon cancer (in Japanese). Nihon fukubukyukyu igakkai zasshi (in Japanese) 35:707–713
Enomoto T, Saida Y, Takabayashi K, Nagao S, Takeshita E, Watanabe R, Takahashi A, Nakamura Y, Asai K, Watanebe M, Nagao J, Kusachi S (2016) Open surgery versus laparoscopic surgery after stent insertion for obstructive colorectal cancer. Surg Today 46:1383–1386
Matsushima H, Adachi T, Hamada T, Moriuchi H, Yamaguchi T, Ichinose H, Goto T, Iwata T, Eguchi S (2017) Elective surgery after endoscopic self-expandable metallic stent placement for patients with obstructive colon cancer: preoperative systemic evaluation and management. Int Surg 102:21–28
Chinswangwatanakul V, Angkurawaranon C, Metasate A, Trakarnsanga A, Jirawat S, Phalanusithepha C, Akaraviputh T (2017) Comparison of laparoscopic versus open surgery after insertion of self-expandable metallic stents in acute malignant colorectal obstruction: a case-matched study. Siriraj Med J 69:57–64
Bae SU, Yang CS, Kim S, Lim DR, Jeong WK, Kim DD, Kim JH, Shin EJ, Lee YJ, Lee JY, Kim NK, Baek SK (2019) Long-term oncologic outcomes of laparoscopic versus open resection following stent insertion for obstructing colon cancer: a multi-center retrospective study. Surg Endosc 33:3937–3944
Tajima JY, Matsuhashi N, Takahashi T, Mizutani C, Iwata Y, Kiyama S, Kubota M, Ibuka T, Araki H, Shimizu M, Doi K, Yoshida K (2020) Short-and long-term outcomes after colonic self-expandable metal stent placement for malignant large-bowel obstruction as a bridge to surgery focus on the feasibility of the laparoscopic approach: a retrospective, single center study. World J Surg Oncol 18:265
Kim MH, Kang SI, Lee J, Oh HK, Ahn S, Kim DW, Kang SB, Shin R, Heo SC, Youk EG, Park SC, Sohn DK, Oh JH, Kim MJ, Park JW, Ryoo SB, Jeong SY, Park KJ, Seoul Colorectal Research Group (SECOG) (2022) Oncologic safety of laparoscopic surgery after metallic stent insertion for obstructive left-sided colorectal cancer: a multicenter comparative study. Surg Endosc 36:385–395
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 29(372):n71
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P, Ga SW, Zello G, Petersen J (2014) The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available at: http://www.ohri.ca/programs/clinical_ epidemiology/oxford.asp. Cited 26 August 2015
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716. https://doi.org/10.1046/j.1445-2197.2003.02748.x
Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, Vist GE, Falck-Ytter Y, Meerpohl J, Norris S, Guyatt GH (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64:401–406
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Egger M, Smith GD, Schneider M, Minderet C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Abramson JH (2011) WINPEPI updated: computer programs for epidemiologists, and their teaching potential. Epidemiol Perspect Innov 8:1–9
van Hooft JE, Bemelman WA, Oldenburg B, Marinelli AW, Lutke Holzik MF, Grubben MJ, Sprangers MA, Dijkgraaf MG, Fockens P, Collaborative Dutch Stent-In Study G (2011) Colonic stenting versus emergency surgery for acute left-sided malignant colonic obstruction: a multicentre randomised trial. Lancet Oncol 12:344–352
Kye BH, Kim JH, Kim HJ, Lee YS, Lee IK, Kang WK, Cho HM, Ahn CH, Oh ST (2010) The optimal time interval between the placement of self-expandable metallic stent and elective surgery in patients with obstructive colon cancer. Sci Rep 10:9502
Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M, Stryker SJ, Beart RW Jr, Hellinger M, Flanagan R Jr, Peters W, Ota D, Clinical Outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AMH, Heath RM, Brown JM, MRC CLASICC trial group (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365:1718–1726
Matsuda A, Yamada T, Ohta R, Sonoda H, Shinji S, Iwai T, Takeda K, Yonaga K, Ueda K, Kuriyama S, Miyasaka T, Yoshida H (2023) Surgical site infections in gastroenterological surgery. J Nippon Med Sch Mar 90:2–10
Okada K, Uemura K, Ohge H, Iseki M, Mizuma M, Shinkawa H, Takahata R, Aoki T, Makino K, Arai H, Miyake T, Takeda S, Yokoyama Y, Yaguchi Y, Kobayashi M, Matsuda A, Shiomi H, Watanabe M, Akagi S, Inoue T, Tanemoto K, Maruyama H (2022) Prognostic impact of postoperative infection in patients with pancreatic cancer: a multicenter cohort study. Surgery 172:1768–1775
Iseki M, Mizuma M, Unno M, Maruyama H, Akagi S, Shimoda M, Uemura K, Inoue T, Shiomi H, Watanabe M, Kobayashi M, Matsuda A, Mizuuchi Y, Aoki T, Shinkawa H, Takahata R, Makino K, Arai H, Yokoyama Y, Takeda S, Yaguchi Y, Kitagawa Y (2023) Prognostic impact of postoperative infection after resection of biliary malignancy: a multicenter retrospective cohort study. Surgery. https://doi.org/10.1016/j.surg.2023.05.019
Matsuda A, Maruyama H, Akagi S, Inoue T, Uemura K, Kobayashi M, Shiomi H, Watanabe H, Fujita T, Takahata R, Takeda S, Fukui Y, Toiyama Y, Hagiwara N, Kaito A, Matsutani T, Yasuda T, Yoshida H, Tsujimoto H, Kitagawa Y (2023) Survival impact of surgical site infection in esophageal cancer surgery: a multicenter retrospective cohort study. Ann Gastroenterol Surg 7:603–614
Artinyan A, Orcutt ST, Anaya DA, Richardson P, Chen GJ, Berger DH (2015) Infectious postoperative complications decrease long-term survival in patients undergoing curative surgery for colorectal cancer: a study of 12,075 patients. Ann Surg 261:497–505
Law WL, Choi HK, Lee YM, Ho JW (2007) The impact of postoperative complications on long-term outcomes following curative resection for colorectal cancer. Ann Surg Oncol 14:2559–2566
Alonso S, Pascual M, Salvans S, Mayol X, Mojal S, Gil MJ, Grande L, Pera M (2015) Postoperative intra-abdominal infection and colorectal cancer recurrence: a prospective matched cohort study of inflammatory and angiogenic responses as mechanisms involved in this association. Eur J Surg Oncol 41:208–214
Salvans S, Mayol X, Alonso S, Messeguer R, Pascual M, Mojal S, Grande L, Pera M (2014) Postoperative peritoneal infection enhances migration and invasion capacities of tumor cells in vitro: an insight into the association between anastomotic leak and recurrence after surgery for colorectal cancer. Ann Surg 260:939–943 (discussion 943-4)
Tevis SE, Kohlnhofer BM, Stringfield S, Foley EF, Harms BA, Heise CP, Kennedy GD (2013) Postoperative complications in patients with rectal cancer are associated with delays in chemotherapy that lead to worse disease-free and overall survival. Dis Colon Rectum 56:1339–1348
Matsuda A, Yamada T, Takahashi G, Matsumoto S, Yokoyama Y, Sonoda H, Ohta R, Shinji S, Sekiguchi K, Kuriyama S, Kanaka S, Yoshida H (2023) Postoperative infectious complications have a negative oncological impact in patients after stent placement with malignant large bowel obstruction. Int J Colorectal Dis 38:2
Acknowledgements
We thank Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Funding
None.
Author information
Authors and Affiliations
Contributions
Study concept and design: SK, TY, AM, KU, and SS. Literature search and data collection: SK and AM. Statistical analysis and interpretation of data: SK, YY, GT, TI, KT, SK, and TM. Drafting of the manuscript: SK. Revising the manuscript: AM and TY. Study supervision: TY and HY. All authors read and approved the final version of the manuscript.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kanaka, S., Yamada, T., Matsuda, A. et al. Short-term and three-year long-term outcomes of laparoscopic surgery versus open surgery for obstructive colorectal cancer following self-expandable metallic stent placement: a meta-analysis. Surg Endosc (2024). https://doi.org/10.1007/s00464-024-11187-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00464-024-11187-x