Abstract
Background
Native liver survival after laparoscopic Kasai portoenterostomy (Lap-PE) for biliary atresia (BA) is controversial. We examined whether a jaundice-free native liver survival rate is comparable between conventional Kasai portoenterostomy (Open-PE) and Lap-PE. Then, the impact of the two types of PE on subsequent living-donor liver transplantation (LTx) was addressed in this study.
Methods
The jaundice-free rate in 1- and 2-year-old patients who underwent Open-PE and Lap-PE from January 2006 to December 2017 was investigated. Additionally, perioperative data (duration from the start of surgery to the completion of hepatectomy and others) of patients aged 2 years or younger who underwent LTx after either Open-PE or Lap-PE from 2006 to 2017 were evaluated.
Results
Thirty-one (67%) out of 46 Open-PE patients and 23 (77%) out of 30 Lap-PE patients showed native liver survival with jaundice-free status at 1 year of age (p = 0.384); 29 (63%) out of 46 Open-PE patients and 19 (70%) out of 27 Lap-PE patients showed native liver survival with jaundice-free status at 2 years of age (p = 0.524); there were no significant differences. Additionally, there were 37 LTx cases after PE within 2 years of birth, including 29 Open-PE and 8 Lap-PE cases. The patients in the Lap-PE group had fewer adhesions and significantly shorter durations of surgery up to the completion of the recipient’s hepatectomy and durations of post-LTx hospital stay compared to the Open-PE group. There were no differences in blood loss or duration of stay in intensive care unit between the Lap-PE and Open-PE groups.
Conclusions
Jaundice-free native liver survival rate has been comparable between Open-PE and Lap-PE. Lap-PE resulted in fewer adhesions, contributing to better outcomes of subsequent LTx compared to Open-PE.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Endoscopic surgery can provide significant benefits to patients, including fast postoperative recovery, less pain than open surgery, and minimal adhesions. It is broadly used even for pediatric surgeries with high technical difficulty, such as those for congenital esophageal atresia or common bile duct dilatation, for which favorable outcomes have been reported [1, 2]. In contrast, endoscopic surgery had not been widely applied to the treatment of biliary atresia (BA), since a lower native liver survival rate was reported after laparoscopic portoenterostomy (Lap-PE) compared to conventional Kasai portoenterostomy (Open-PE) [3, 4]. The number of Lap-PE cases has been gradually accumulating, and they demonstrate outcomes comparable to those of Open-PE, including native liver survival rate. The critical end point of PE, which is jaundice-free native liver survival rate, has been comparable between Open-PE and Lap-PE [5,6,7].
Kasai portoenterostomy (PE) is regarded as the standard initial therapy for BA. Nevertheless, the success rate of Kasai PE as a sole method to resolve BA has not improved for more than 20 years, resulting in 35–60% of the patients requiring liver transplantation (LTx) after PE [8,9,10]. Moreover, 80% of these patients undergo LTx within 2 years of birth [11,12,13]. Since the interval between the last PE and subsequent LTx is relatively short, it is important to evaluate the impact of PE on LTx. However, there are only few reports comparing Lap-PE and Open-PE with regard to the impact on subsequent LTx surgery [4, 13, 14]. Additionally, adhesions, whose minimal occurrence is one of the most important advantages of Lap-PE, were evaluated in a very limited number of cases in comparison with Open-PE, precluding adequate statistical analysis [13].
If the native liver survival rate is comparable between Lap-PE and Open-PE, it is better to select the procedure with lower impact on subsequent LTx. Initially, we evaluated the jaundice-free native liver survival rate between Open-PE and Lap-PE and thereafter determined the impact of Lap-PE on LTx, which is performed in more than 30% of patients receiving PE [15, 16].
Materials and methods
Patients
We obtained approval from the institutional ethics board of Nagoya University Graduate School of Medicine, Nagoya, Japan, for a retrospective review of the medical records of patients diagnosed with BA (approval number: 2015-0094) and progressive study of Lap-PE (approval number: 2014-0400) and consent from patients or their parents.
The jaundice-free native liver survival rate was investigated in 76 1-year-old and 73 2-year-old patients who underwent Open-PE and Lap-PE at our institution from January 2006 to December 2017.
Additionally, we evaluated the perioperative data of 37 patients (13 male and 24 female) who underwent LTx after PE, aged within 2 years between 2006 and 2017. The following parameters were measured: time elapsed between the start of surgery and the completion of the hepatectomy, blood loss, total duration of surgery, complications during surgery, days of intensive care unit (ICU) stay, and length of post-LTx hospital stay. Because living-donor LTxs were performed, in some cases, the time from the start of surgery to the completion of hepatectomy included the time of waiting for the donor’s liver to be removed. In such cases, the waiting time was subtracted from the analysis. Patients were required to have a diagnosis of BA based on a combination of radiographic findings, uncorrectable surgical findings, and liver histology. Patients with total serum bilirubin (T-bil) levels of 1.2 mg/dl or lower were regarded as having achieved a jaundice-free status.
Laparoscopic Kasai portoenterostomy
All manipulations of the hilar region are done using 3-mm forceps and 5-mm microbipolar forceps. The area between the right porta hepatis, in which the right anterior branch of the hepatic artery and portal vein enter the hepatic parenchyma, and the left porta hepatis, in which the left branch of the portal vein enters the parenchyma, is dissected for anastomosis. The fibrous tissue in the hilar plate is dissected just before exposing the liver parenchyma. The fibrous tissue is not completely resected and is held lightly on the hilar plate after dissection, which is the issue of Kasai portoenterostomy that we are most concerned about. After creating a Roux-en-Y limb with exteriorization via the umbilical incision, end-to-side portoenterostomy is performed laparoscopically [17].
Kasai portoenterostomy revision
We have been actively performing revision of Kasai PE for cases that have lower tendency for jaundice after initial surgery but are not completely jaundice-free. In patients included in the recurrent jaundice or cholangitis group who underwent successful initial PE, we also are on the indication of revision. Cases of intractable ascites and liver failure that show abnormal coagulation are not indicated for revision.
Statistical analysis
Statistical analyses were performed using χ2 test and Wilcoxon rank sum test for continuous variables with SAS version 9.4 (SAS Institute, Cary, NC, USA). A p value < 0.05 was considered statistically significant.
Results
During the study period, PE was conducted in 78 cases at our institution, including 47 Open-PE and 31 Lap-PE cases. We excluded one case from each group. One case with severe congenital heart disease resulting in a hospital transfer was excluded from the laparotomy group. We also excluded cases in which laparoscopy had been converted to laparotomy during reoperation. All other reoperations (revision Kasai PE) were performed in the same manner as that of the initial surgery.
In December 2013, laparoscopic surgery became the standard procedure for BA, and all cases were henceforth performed laparoscopically. Lap-PE was performed in 31 patients by December 2017, and there was an instance when 25 cases reached jaundice-free status after Lap-PE. Thirty-one (67%) out of 46 Open-PE patients and 23 (77%) out of 30 Lap-PE patients showed native liver survival with jaundice-free status at 1 year of age (p = 0.384); 29 (63%) out of 46 Open-PE patients and 19 (70%) out of 27 Lap-PE patients showed native liver survival with jaundice-free status at 2 years of age (p = 0.524); there were no significant differences (Table 1). Eighteen Open-PE (39%) and 8 Lap-PE (27%) cases required subsequent LTx within 2 years of birth. Comparing the Lap-PE group with the Open-PE group, the age of surgery was significantly higher, the operation time was shorter, and the amount of bleeding was greater in the Open-PE group. The meal start time and drain removal time were significantly earlier in the Lap-PE group. This comparison may have been somewhat influenced by the historical background, as the old cases were open and the new ones were laparoscopic (Table 1).
Of the 30 patients who underwent Lap-PE, 9 underwent revision Lap-PE, of whom 8 reached jaundice-free status.
LTx was carried out in 3 cases in the revision Lap-PE group, including 1 case without jaundice-free status, 1 case with initially decreased but subsequently increased jaundice, and 1 case with repeated cholangitis.
During the study period, 38 patients underwent LTx within 2 years of birth, including 11 patients who underwent PE at another hospital. We excluded one case of conversion from laparoscopy to laparotomy. Among the 37 cases included, 29 patients underwent LTx after Open-PE and 8 patients underwent LTx after Lap-PE. Lap-PE cases exhibited fewer adhesions and had significantly shorter durations of surgery up to the completion of the recipient’s hepatectomy (median 136 min; range 117–210 min) compared with to Open-PE cases (median 232 min; range 141–334 min; p = 0.0003; Figs. 1, 2). The duration of post-LTx hospital stay was significantly shorter in the Lap-PE cases (median 47 days; range 29–138 days) than in the Open-PE cases (median 87 days; range 30–384 days; p = 0.022). There were no significant differences in blood loss or duration of ICU stays between the Lap-PE (median 598 ml; range 161–2472 ml, and median 6 days; range 2–43 days, respectively) and the Open-PE groups (median 1337 ml; range 145–5684 ml, and median 5 days; range 1–62 days, respectively). There was one intraoperative complication, inferior vena cava injury, in the Open-PE group. There were no intraoperative complications in the Lap-PE group (Table 2).
Revision Open-PE was performed in 9 of 29 patients who underwent open surgery. Open-PE in revision patients had significantly longer durations of surgery up to the completion of the recipient’s hepatectomy (median 263 min; range 144–291 min) in contrast to Open-PE without revision cases (median 219 min; range 141–334; p = 0.043; Table 3). Revision Lap-PE was performed in 3 out of the 8 patients who underwent laparoscopic surgery. There were no significant differences between the Lap-PE with revision (median 125 min; range 121–210 min) and Lap-PE without revision groups (median 140 min; range 117–185 min; Table 4) in terms of the duration of surgery up to the completion of the recipient’s hepatectomy.
To exclude the effects of adhesions due to double open surgery, we compared Open-PE with revision and Lap-PE with revision as well as Open-PE without revision and Lap-PE without revision. Lap-PE without revision patients had significantly shorter durations of surgery up to the completion of the recipient’s hepatectomy (median 140 min; range 117–185 min) in contrast to Open-PE without revision patients (median 219 min; range 141–334 min; p = 0.003) (Table 5). Lap-PE with revision patients had significantly shorter durations of surgery up to the completion of the recipient’s hepatectomy (median 125 min; range 121–210 min) in contrast to Open-PE with revision patients (median 263 min; range 144–291 min; p = 0.021; Table 6).
Discussion
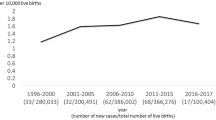
LTx for BA has dramatically improved patient survival rates [18]. Treatment of BA always includes the possibility of LTx. Nevertheless, it is best for the patient to survive with a native liver without jaundice. Therefore, it is important to perform surgery that does not interfere with future LTx while also avoiding LTx to the greatest extent possible. This premise is indispensable in determining the treatment protocol for BA, including laparotomy, laparoscopy, or revision PE. We hypothesized that if the result of Lap-PE is not different from that of Open-PE, the former would be better for BA by allowing subsequent LTx to be easier due to reduced adhesions and more rapid recovery. Thus, we conducted this study to analyze this hypothesis. Since this study aimed to evaluate the influence of PE on LTx, the period from PE to LTx was compared in cases where surgery was performed in patients younger than 2 years of age. Oetzmann von Sochaczewski et al. [16] compared the impact on subsequent LTx between 11 Open-PE cases and 8 Lap-PE cases and reported no differences in their end points, including the surgical duration up to the completion of the recipient’s hepatectomy. In contrast, our evaluation demonstrated a significantly shorter duration for hepatectomy [16]. The outcome of Lap-PE for BA has remained controversial [3, 5, 6, 13, 19]. Although there are some reports in the literature arguing against the effectiveness of Lap-PE, its outcome has compared favorably with that of Open-PE at our institution and also in other standard Open-PE reports [8]. We encountered 76 Open-PE cases at our hospital during the period from 1996 through 2013, in which a jaundice-free native liver survival rate was 63% (48/76 cases). Revision PE was required in 7 out of 48 cases [20]. The jaundice-free rate in our hospital was generally comparable with other reports, although direct comparison is impossible due to differences in study design [8, 15]. In this study, we compared the results of Open and Lap-PE surgeries from 2006 to 2017 in our hospital. There was a significant difference in the age at which surgery was performed between the two groups. Since 2011, stool color information was added in maternal handbooks in Japan for early detection of BA. This information makes it faster for visiting hospital. As laparoscopic surgery became the standard procedure for BA since December 2013, all cases were henceforth performed laparoscopically; hence, the patients in the Open-PE group were older than those in the Lap-PE group, making age difference an unsuitable basis for comparison of surgical results. However, according to a study of 3160 patients with BA in Japan by Nio [21], the results of surgery up to the age of 80 days are not affected by the age at surgery. Comparison of the Lap-PE group (with 37 patients, excluding 9 patients who were 80 days or older)with the Open-PE group revealed no significant difference in the jaundice-free native liver survival rates between the two groups at 1 year and 2 years of age (at 1 year of age: Open-PE, 27/37, 73%; Lap, 23/30, 77%, p = 0.730; at 2 years of age: Open, 25/37, 68%; Lap, 19/27, 70%, p = 0.811).
The standard treatment algorithm for patients with BA consists of PE followed by LTx if PE fails; revision of PE has tended to be viewed negatively because of the possibility of future LTx [22,23,24]. In our review, the transplant surgeon reported that adhesions were mild, even in cases where revision was performed in the Lap-PE group. For Open-PE patients, but not in Lap-PE cases, the effects of revisions were observed at the time of completion of hepatectomy. This may help challenge the common belief that revision hinders LTx and should not be done. Although it is a short-term result, in the Lap-PE group, 6 (67%) out of 9 patients survived jaundice-free with a native liver after revision; therefore, there is a possibility that the adoption of revision surgery may be expanded by applying Lap-PE. Future research is needed to confirm the advantage of Lap-PE seen in the current study and also to ascertain that this advantage is retained even if revision is performed.
Limitations
Several limitations of the current study should be considered. First, no objective evaluation procedure for the severity of adhesions is available; therefore, the severity of adhesions in this study was determined based on the operative record alone. Since adhesions affect the duration of surgery up to the completion of the recipient’s hepatectomy, the association between the adhesions and the period to hepatectomy completion was objectively evaluated. However, this evaluation may not accurately reflect the severity of the adhesions. Second, no established indicators of revision PE efficacy exist, and the revision could potentially influence the LTx outcomes. Finally, since Lap-PE was introduced relatively recently, the follow-up period was limited, precluding the capability to evaluate potential long-term complications, warranting further long-term and thorough evaluation with a larger study size.
Conclusions
In this study, jaundice-free native liver survival rate has been comparable between Open-PE and Lap-PE. Lap-PE cases had a significantly shorter surgical duration up to the completion of the recipient’s hepatectomy during LTx in comparison to Open-PE cases. This study demonstrated that Lap-PE has a favorable advantage over Open-PE in terms of subsequent LTx, possibly due to reduced adhesions.
References
van der Zee DC, Gallo G, Tytgat SHA (2015) Thoracoscopic traction technique in long gap esophageal atresia: entering a new era. Surg Endosc 29:3324–3330
Le DM, Woo RK, Sylvester K, Krummel TM, Albanese CT (2006) Laparoscopic resection of type 1 choledochal cysts in pediatric patients. Surg Endosc 20:249–251
Ure B, Kuebler J, Schukfeh N, Engelmann C, Dingemann J, Petersen C (2011) Survival with the native liver after laparoscopic versus conventional Kasai portoenterostomy in infants with biliary atresia: a prospective trial. Ann Surg 253:826–830
Dutta S, Woo R, Albanese C (2007) Minimal access portoenterostomy: advantages and disadvantages of standard laparoscopic and robotic techniques. J Laparoendosc 172:258–264
Murase N, Hinoki A, Shirota C, Tomita H, Shimojima N, Sasaki H, Nio M, Tahara K, Kanamori Y, Shinkai M, Yamamoto H, Sugawara Y, Hibi T, Ishimaru T, Kawashima H, Koga H, Yamataka A, Uchida H (2019) Multicenter, retrospective, comparative study of laparoscopic and open Kasai portoenterostomy in children with biliary atresia from Japanese high-volume centers. J Hepatobiliary Pancreat Sci 26:43–50
Chan KWE, Lee KH, Wong HYV, Tsui SYB, Mou JWC, Tam YHP (2019) Ten- year native liver survival rate after laparoscopic and open Kasai portoenterostomy for biliary atresia. J Laparoendosc Adv Surg Tech. https://doi.org/10.1089/lap.2018.0350
Li Y, Gan J, Wang C, Xu Z, Zhao Y, Ji Y (2019) Comparison of laparoscopic portoenterostzomy and open portoenterostomy for the treatment of biliary atresia. Surg Endosc. https://doi.org/10.1007/s00464-019-06905-9
Nio M, Sasaki H, Wada M, Kazama T, Nishi K, Tanaka H (2010) Impact of age at Kasai operation on short- and long-term outcomes of type III biliary atresia at a single institution. J Pediatr Surg 45:2361–2363
Ibrahim M, Miyano T, Ohi R, Saeki M, Shiraki K, Tanaka K, Kamiyama T, Nio M (1997) Japanese biliary atresia registry, 1989 to 1994. Tohoku J Exp Med 181:85–957
Toyosaka A, Okamoto E, Okasora T, Nose K, Tomimoto Y (1993) Outcome of 21 patients with biliary atresia living more than 10 years. J Pediatr Surg 28:1498–1501
Qiao G, Li L, Cheng W, Zhang Z, Ge J, Wang C (2015) Conditional probability of survival in patients with biliary atresia after Kasai portoenterostomy: a Chinese population-based study. J Pediatr Surg 50:1310–1315
Muraji T, Nishijima E, Higashimoto Y, Tsugawa C (1997) Biliary atresia: current management and outcome. Tohoku J Exp Med 181:155–160
Hussain MH, Alizai N, Patel B (2017) Outcomes of laparoscopic Kasai portoenterostomy for biliary atresia: a systematic review. J Pediatr Surg 52:264–267
Martinez-Ferro M, Esteves E, Laje P (2005) Laparoscopic treatment of biliary atresia and choledochal cyst. Semin Pediatr Surg 14:206–215
Wong ZH, Davenport M (2019) What happens after Kasai for biliary atresia? A European multicenter survey. Eur J Pediatr Surg 29:1–6
Oetzmann von Sochaczewski C, Petersen C, Ure BM, Osthaus A, Schubert KP, Becker T, Lehner F, Kuebler JF (2012) Laparoscopic versus conventional Kasai portoenterostomy does not facilitate subsequent liver transplantation in infants with biliary atresia. Laparoendosc Adv Surg Tech 22(4):408–412
Murase N, Uchida H, Ono Y, Tainaka T, Yokota K, Tanano A, Shirota C, Shirotsuki R (2015) A new era of laparoscopic revision of Kasai portoenterostomyfor the treatment of biliary atresia. Biomed Res Int 2015:173014
Gallo A, Esquivel CO (2013) Current options for management of biliary atresia. Pediatr Transplant 17:95–98
Nakamura H, Koga H, Cazares J, Okazaki T, Lane GJ, Miyano G, Okawada M, Doi T, Urao M, Yamataka A (2016) A comprehensive assessment of prognosis after laparoscopic portoenterostomy for biliary atresia. J Pediatr Surg 32(2):109–112
Shirota C, Uchida H, Ono Y, Murase N, Tainaka T, Yokota K, Oshima K, Shirotsuki R, Hinoki A, Ando H (2016) Long-term outcomes after revision of Kasai portoenterostomy for biliary atresia. J Hepatobiliary Pancreat Sci 23:715–720
Nio M (2017) Japanese biliary atresia registry. Pediatr Surg Int 33:1319–1325
Nio M, Sasaki H, Tanaka H, Okamura A (2013) Redo surgery for biliary atresia. Pediatr Surg Int 29:989–993
Mendoza MM, Chiang JH, Lee SY, Kao CY, Chuang JH, Tiao MM, Hsieh CS (2012) Reappraise the effect of redo-Kasai for recurrent jaundice following Kasai operation for biliary atresia in the era of liver transplantation. Pediatr Surg Int 28:861–864
Sumida W, Uchida H, Tanaka Y, Tainaka T, Shirota C, Murase N, Oshima K, Shirotsuki R, Chiba K (2017) Review of redo-Kasai portoenterostomy for biliary atresia in the transition to the liver transplantation era. Nagoya J Med Sci 79:415–420
Funding
No funding was provided for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Chiyoe Shirota, Naruhiko Murase, Yujiro Tanaka, Yasuhiro Ogura, Hideya Kamei, Nobuhiko Kurata, Masahiro Nakatochi, Akinari Hinoki, Takahisa Tainaka, Wataru Sumida, Kazuki Yokota, Satoshi Makita, Kazuo Oshima, and Hiroo Uchida have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shirota, C., Murase, N., Tanaka, Y. et al. Laparoscopic Kasai portoenterostomy is advantageous over open Kasai portoenterostomy in subsequent liver transplantation. Surg Endosc 34, 3375–3381 (2020). https://doi.org/10.1007/s00464-019-07108-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07108-y