Abstract
Purpose
It is important for patients with biliary atresia (BA) to retain the native liver after Kasai portoenterostomy (PE). Laparoscopic PE (Lap-PE) is standard, whereas laparoscopic revision of PE (Lap-revision) is performed as needed. We report the medium-term outcomes of Lap-revision.
Methods
We retrospectively reviewed the demographics and outcomes of 63 patients who underwent Lap-PE between 2013 and 2021. Indications for revision included recurrent jaundice, repeat cholangitis, and persistent jaundice with temporary biliary excretion following the initial PE. We compared liver transplantation (LT) data of patients who underwent Lap-revision with those of patients who did not.
Results
Lap-revision was performed in 20 patients. Of those 17 (excluding the two who were jaundice-free before the age of 1, and the one who underwent open conversion for bleeding), 11 (65%) were jaundice-free 1 year after Lap-revision. The surgical parameters of LT did not differ between patients who underwent Lap-revision and those who did not.
Conclusion
Lap-revision for patients with BA had a limited but positive effect on native liver survival and did not adversely affect subsequent LT. Therefore, Lap-revision could be second-line standard therapy in patients with BA who have demonstrated biliary drainage at least once after initial PE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Biliary atresia (BA) is a progressive fibrous obstructive cholangiopathy of the intrahepatic and extrahepatic biliary tract that leads to liver failure. Although liver transplantation (LT) improves the prognosis of patients with BA, Kasai portoenterostomy (PE) remains the standard initial therapy because of the complications of LT, the medical costs associated with LT, and the shortage of qualified donors [1, 2]. In patients with BA, preservation of the native liver is important after PE. Many reports [3,4,5] have suggested that laparotomic revision of PE could delay the need for LT and help improve survival of the native liver. Laparoscopic PE (Lap-PE) is the standard procedure in our institution, and laparoscopic revision of PE (Lap-revision) is performed as needed. However, neither the outcome of Lap-revision in patients with BA after initial Lap-PE nor the effect of Lap-revision on LT has been extensively reported [6, 7]. We describe the medium-term outcomes after Lap-revision at our institution.
Methods
We obtained approval from the ethics board of our institution for a retrospective review of the medical records of patients in whom BA was diagnosed between December 2013 and October 2021 (approval number: 2021-0409) and consent from patients or their parents to participate in our study.
We evaluated 65 patients in whom BA was diagnosed through a combination of intraoperative cholangiographic findings and histological liver findings. Of these patients, 63 who underwent Lap-PE at our institution were included in this study. We excluded the other two patients, who had undergone open PE; one was ineligible for reasons involving hospital insurance rules, and one had undergone craniotomy for cerebral hemorrhage.
Total serum bilirubin levels lower than 1.5 mg/dl were considered indicative of jaundice-free status; inability to achieve jaundice-free status after initial Lap-PE was indicative of persistent jaundice; and reappearance of jaundice after an initial jaundice-free period was considered recurrent jaundice. In addition, cases of native liver survival and jaundice-free status at the timing of writing were regarded as “native liver with jaundice-free,” and cases of patients with recurrent jaundice and who awaited LT were considered “native liver with jaundice.”
Indications for revision included recurrent jaundice, repeat cholangitis, and persistent jaundice with temporary biliary excretion at one time following the initial PE.
On the other hand, patients in whom jaundice recurred 1 year or more after Lap-PE were candidates for LT without revision, because they had achieved adequate growth and development to safely undergo an LT. We performed revision after we explained the treatment options, including LT, to the patients’ parents and obtained their consent.
We recorded demographic and clinical data, including sex, age, and body weight, total serum bilirubin level at the time of Lap-PE and lowest postoperative total serum bilirubin level, and surgical parameters (operation time, blood loss, and complications). We compared the surgical parameters of patients who underwent Lap-PE alone with those of patients who also underwent Lap-revision. We also investigated the rate of native liver preservation after Lap-PE. In addition, we evaluated the perioperative data of patients who underwent LT after Lap-PE: age, body weight at the time of LT, time elapsed between the start of surgery and completion of hepatectomy, blood loss, and length of post-LT stay in the intensive care unit.
Laparoscopic Kasai portoenterostomy
The patient was placed in the supine position. Then, we made a Mercedes incision in the umbilicus to widen the orifice as much as possible [8]. We inserted a multichannel port with a 5-mm camera port through the incision, two 3-mm ports into the right paraumbilical region and the left upper abdomen each, and a 3-mm port into the right upper abdomen. For all manipulations in the hilar region, we used 3-mm forceps and 3-mm bipolar forceps. The area between the right porta hepatis, in which the right anterior branch of the hepatic artery and portal vein entered the hepatic parenchyma, and the left porta hepatis, in which the left branch of the portal vein entered the parenchyma, was dissected for anastomosis. The fibrous tissue in the hilar plate was dissected just before the liver parenchyma was exposed. The fibrous tissue was not completely resected; it was held lightly on the hilar plate after dissection. After we created a retrocolic Roux limb with exteriorization via the umbilical incision, we performed end-to-side portoenterostomy laparoscopically [9, 10].
Laparoscopic revision of Kasai portoenterostomy
In Lap-revision, the ports were placed as in the initial Lap-PE without an additional skin incision. After intraoperative peritoneal adhesiolysis, the anastomosed Roux limb was completely dissected adjacent to the porta hepatis. To avoid unexpected excessive bleeding, the tissues were manipulated carefully. In recurrent and persistent jaundice, the newly developed fibrous extrahepatic tissue was removed, and the hilar plate was superficially dissected just before the liver parenchyma was exposed. In repeat cholangitis, the fibrous tissue was dissected more deeply, and the newly developed bile lake was opened. We performed end-to-end PE laparoscopically after trimming the tail of the Roux limb [6].
Statistical analysis
Medians and interquartile ranges were calculated for continuous measures, and frequencies and percentages were calculated for categorical measures. We used Fisher’s exact test and the Mann–Whitney U test for categorical and continuous variables, respectively. Values of p < 0.05 were considered statistically significant. To calculate survival rates, we used the Kaplan–Meier estimator. The Kaplan–Meier survival curves reflected the days after initial Lap-PE. We used the log-rank test to compare the survival curves between patients who underwent Lap-PE and those who did not undergo Lap-revision.
Results
The demographic and clinical characteristics of the 63 patients who underwent Lap-PE are summarized in Table 1. The median follow-up period was 4 years, ranging from 7 months to 8 years. In 46 patients (73%), total serum bilirubin levels were transiently normalized after initial Lap-PE. Among the patients, we found no significant differences in age, total serum bilirubin levels at the time of surgery, or surgical parameters.
Patient selection and grouping in this study are summarized in Fig. 1. Lap-PE was performed in 63 patients, all of whom had an operative definitive diagnosis of BA. Lap-revision was performed in 20 patients (10 with persistent jaundice, 8 with recurrent jaundice, and 2 with repeat cholangitis). Of those 20 patients, 14 achieved jaundice-free status at least once. To date, of the 20 patients who underwent Lap-revision, 4 retained the native liver and continue to be jaundice-free. LT was performed in 27 patients. Seven patients who suffered recurrent jaundice (four who underwent Lap-PE alone and three who underwent Lap-revision) continue to wait for LT to date.
The surgical parameters of the 63 patients are listed in Table 2. Amounts of blood loss and rates of open conversion did not differ between patients who underwent Lap-PE alone and those who underwent Lap-revision. Data from one patient who underwent open conversion revision for bleeding were excluded from subsequent analysis. The patient who underwent open conversion and were initially jaundice-free but later developed recurrent jaundice underwent LT. Lap-revision was significantly shorter than initial Lap-PE (p < 0.001).
Demographic and clinical characteristics of the 19 patients who underwent Lap-revision (excluding the patient in whom the procedure was converted to open laparotomy) are summarized in Table 3. Of those 19, 14 (74%; 6 with persistent jaundice, 6 with recurrent jaundice, and 2 with repeat cholangitis) were transiently jaundice-free after Lap-revision. We found no significant differences in patient background (age, interval from the initial to revision, and total serum bilirubin level) and surgical parameters (operation time, blood loss, and postoperative complication) between the patients who were transiently jaundice-free and those who were not.
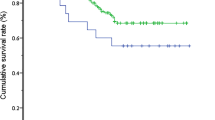
The Kaplan–Meier curves for native liver survival are shown in Fig. 2. All patients, including those who underwent only Lap-PE and those who underwent Lap-revision, were compared, and no significant differences were found. Of the 17 patients out of 19, excluding the two cases with less than 1 year after Lap-revision, 11 (5 with persistent jaundice, 4 with recurrent jaundice, and 2 with repeat cholangitis) were jaundice-free 1 year after Lap-revision (Table 4). Moreover, of 16 patients whose native livers were preserved, 3 (2 with persistent jaundice and 1 with recurrent jaundice) were jaundice-free 4 years or more after Lap-revision (Table 4).
Kaplan–Meier curves, showing the length of native liver survival from initial laparoscopic portoenterostomy (Lap-PE). The vertical dashes represent patients who underwent liver transplantation. The solid curve represents the whole patient population; the widely dashed curve represents those who underwent only Lap-PE, and the narrowly dashed curve represents those who underwent Lap-revision
Characteristics and surgical parameters of 26 patients who underwent LT (12 who had undergone Lap-revision and 14 who had not) were evaluated. Indications for LT included jaundice in 21 cases and portal hypertension in 5 cases (1 pulmonary hypertension and 4 recurrent gastrointestinal bleeding). No significant differences were found between the two groups (Table 5). LTs were performed at three institutions, and the results were not significantly affected by differences in institutions.
Discussion
It is best for patients to retain the native liver without jaundice, although LT has dramatically improved rates of survival among patients with BA [11]. The necessity of and indications for revision in patients with insufficient biliary drainage after PE are controversial [1, 4, 12, 13]. According to the Japanese Biliary Atresia Registry (n = 2630), revision of PE was performed in 552 patients (21%), and among those patients, the bilirubin concentration was normalized in 193 (35%) [1]. The efficacy of laparotomic revision of PE has also been reported. Bondoc et al. [4] reported that among 24 patients who underwent revision of PE, the native liver was preserved in 46% (11 patients) at a maximum follow-up of 15 years. Shirota et al. also reported that revision of PE could have a positive effect in preserving the native liver [5].
A recent retrospective cohort study demonstrated that of 25 patients who had good bile drainage after initial Lap-PE, 20 (80%) achieved normal bilirubin concentrations after Lap-revision [7]. These good results were attributed to the rigorous selection of patients after the initial Lap-PE. The authors did not perform Lap-revision in patients with poor reduction of jaundice after Lap-PE; in fact, Lap-revision has not been recommended for such patients in some reports [4, 14]. To the best of our knowledge, none of the earlier reports have focused on the use of Lap-revision for the treatment of persistent jaundice after Lap-PE. We performed Lap-revision even in patients with initial poor biliary drainage (persistent jaundice), and in some of these patients, the native liver was preserved and jaundice was alleviated after the procedure. In our study, among the ten patients who underwent Lap-revision for persistent jaundice after initial Lap-PE, six (60%) became transiently jaundice-free (Table 3). Moreover, five patients (50%) were transiently jaundice-free 1 year after Lap-revision, and two (25%) retained the native liver with freedom from jaundice (for 7 and 4 years at the timing of writing; Table 4). These results suggest that Lap-revision may be beneficial in the treatment of persistent jaundice after Lap-PE.
In 46 of the 63 (73%), total serum bilirubin levels transiently decreased lower than 1.5 mg/dl after initial Lap-PE. Lap-revision was performed as needed. Including those who underwent Lap-revision, 34 (67%) patients achieved native liver survival with jaundice-free 1 year after initial Lap-PE. In addition, the native liver was preserved in 25% of jaundice-free patients and 17% of patients with persistent or recurrent jaundice after initial Lap-PE over 4 years old (Table 4). These results are similar to that in a previous retrospective cohort study of long-term outcomes after laparotomic revision of PE [5]. Although long-term follow-up of these cases is necessary, Lap-revision could have a limited but positive effect on native liver survival in patients with BA who have recurrent or persistent jaundice and who have undergone initial Lap-PE.
With regard to the histopathological findings of the hilar plate resected at Lap-revision, fibrous connective tissue was observed in all cases with preserved histopathological findings. The bile duct was observed in only one of nine LT cases and in three of four native livers that survived without jaundice. As reported previously [15], the presence of bile duct tissue in the hilar plate at the time of Lap-revision might be associated with the subsequent jaundice-free rate.
Intraoperative bleeding is a complication of revision that occurs, because the vessels around the porta hepatis are separated and exposed during PE. The amount of blood loss in laparoscopic procedures is generally less than that in laparotomic procedures. However, during laparoscopy, oozing of blood from the remains of the hilar fibrous plate is sometimes difficult to stop. Moreover, accidental portal hemorrhage is quite dangerous. In the event of uncontrolled hemorrhage, open conversion should be implemented without additional risks to ensure the safety of patients. In our study, the amount of blood loss and the rate of conversion among patients undergoing Lap-revision were not significantly different from those among patients who underwent Lap-PE alone; on the contrary, Lap-revision was significantly shorter than Lap-PE. Lap-revision may be shorter, because the Roux limb is not created, which is a time-consuming step in Lap-PE.
In the treatment of BA, the need for LT is always a possibility. Therefore, the surgery that is performed must not hamper future LT. Some surgeons hesitate to perform revision of PE, because multiple abdominal procedures are thought to cause adhesions and increase the surgical risks during subsequent LT [12, 13]. Murase et al. [6] reported that hepatectomy during LT took significantly longer in patients who had undergone open revision of PE than in patients who had not undergone laparotomic revision of PE. Moreover, in laparotomic revision of PE, the adhesions around the porta hepatis were dense, and adhesiolysis took a long time [6]. On the other hand, Shirota et al. reported that patients who underwent Lap-PE had fewer adhesions, and surgery was significantly shorter up to the completion of the recipients’ hepatectomy, in comparison with cases of laparotomic PE [5]. In our study, neither LT duration nor blood loss of LT significantly differed between patients who underwent Lap-revision and those who did not (Table 5). These results indicate that Lap-revision, which is relatively minimally invasive, could be a second-line standard therapy for patients with BA who eventually require LT, because the postoperative adhesions are less severe.
Our study had several limitations. First, to examine the significance of Lap-revision, it is necessary to conduct a prospective study by dividing the patients into two treatment groups, one with a Lap-revision protocol from the beginning and the other without a Lap-revision protocol. However, given the small number of cases and difficulty in assigning patients to the no Lap-revision protocol, a prospective study would also be challenging. At our institution, 22/76 (29%) patients underwent laparotomic revision before 2012, and the lap-revision results are similar to those of laparotomic revision [5]. Lap-revision could have a positive effect on the survival of the native liver in patients with BA. Second, the follow-up period was short, which precluded the evaluation of long-term survival of the native liver in patients who remained jaundice-free. We continue to track three patients (two with persistent jaundice and one with recurrent jaundice) who retained their native livers and became jaundice-free (Table 4). Third, only a few cases were available for evaluation, which could have led to statistical errors; larger populations are needed in future studies. Fourth, the severity of adhesions was evaluated on the basis of the operative record alone. Moreover, the duration up to hepatectomy includes the time spent waiting for donor hepatectomy. In cases wherein the time spent waiting for donor hepatectomy was obvious, we tried to remove that time. As far as we could investigate, there were no cases wherein the recipient had a long waiting time. A more accurate comparison could have been made by the amount of blood loss up to the hepatectomy. However, only the total intraoperative blood loss was compared, because the amount of blood loss up to hepatectomy was not available on the operative record. Although adhesions affect the duration of surgery up to the completion of the recipients’ hepatectomy, our findings may not reflect the severity of the adhesions.
Conclusion
Lap-revision for recurrent and persistent jaundice after initial Lap-PE in patients with BA, who have demonstrated biliary drainage at least once after initial PE, had a limited but positive effect on native liver preservation. Thus, some patients with BA might benefit from Lap-revision and preservation of the native liver. Therefore, Lap-revision could be regarded as the second-line standard therapy for patients with BA who require future LT, because Lap-revision does not cause severe postoperative adhesions. Further studies must involve larger numbers of patients and longer follow-up.
References
Nio M, Sasaki H, Tanaka H, Okamura A (2013) Redo surgery for biliary atresia. Pediatr Surg Int 29:989–993. https://doi.org/10.1007/s00383-013-3396-3
Hartley JL, Davenport M, Kelly DA (2009) Biliary atresia. Lancet 374:1704–1713. https://doi.org/10.1016/S0140-6736(09)60946-6
Mendoza MM, Chiang J-H, Lee S-Y et al (2012) Reappraise the effect of redo-Kasai for recurrent jaundice following Kasai operation for biliary atresia in the era of liver transplantation. Pediatr Surg Int 28:861–864. https://doi.org/10.1007/s00383-012-3154-y
Bondoc AJ, Taylor JA, Alonso MH et al (2012) The beneficial impact of revision of Kasai portoenterostomy for biliary atresia: an institutional study. Ann Surg 255:570–576. https://doi.org/10.1097/SLA.0b013e318243a46e
Shirota C, Uchida H, Ono Y et al (2016) Long-term outcomes after revision of Kasai portoenterostomy for biliary atresia. J Hepatobiliary Pancreat Sci 23:715–720. https://doi.org/10.1002/jhbp.395
Murase N, Uchida H, Ono Y et al (2015) A new era of laparoscopic revision of Kasai portoenterostomy for the treatment of biliary atresia. Biomed Res Int 2015:173014. https://doi.org/10.1155/2015/173014
Ji Y, Zhang X, Chen S et al (2021) Medium-term outcomes after laparoscopic revision of laparoscopic Kasai portoenterostomy in patients with biliary atresia. Orphanet J Rare Dis 16:193. https://doi.org/10.1186/s13023-021-01835-z
Amano H, Uchida H, Kawashima H et al (2015) The umbilical Benz incision for reduced port surgery in pediatric patients. JSLS 19(e2014):00238. https://doi.org/10.4293/JSLS.2014.00238
Uchida H, Shirota C, Tainaka T (2021) Operative procedures: laparoscopic kasai procedure. In: Nio M (ed) Introduction to biliary atresia. Springer, Singapore, pp 147–156
Shirota C, Hinoki A, Tainaka T et al (2022) Laparoscopic Kasai portoenterostomy can be a standard surgical procedure for treatment of biliary atresia. World J Gastrointest Surg 14:56–63. https://doi.org/10.4240/wjgs.v14.i1.56
Gallo A, Esquivel CO (2013) Current options for management of biliary atresia. Pediatr Transplant 17:95–98. https://doi.org/10.1111/petr.12040
Urahashi T, Ihara Y, Sanada Y et al (2013) Effect of repeat Kasai hepatic portoenterostomy on pediatric live-donor liver graft for biliary atresia. Exp Clin Transplant 11:259–263. https://doi.org/10.6002/ect.2012.0188
Sugawara Y, Makuuchi M, Kaneko J et al (2004) Impact of previous multiple portoenterostomies on living donor liver transplantation for biliary atresia. Hepatogastroenterology 51:192–194
Shneider BL, Brown MB, Haber B et al (2006) A multicenter study of the outcome of biliary atresia in the United States, 1997 to 2000. J Pediatr 148:467–474. https://doi.org/10.1016/j.jpeds.2005.12.054
Mukhopadhyay SG, Roy P, Chatterjee U et al (2014) A histopathological study of liver and biliary remnants in the long-term survivors (>10 years) of cases of biliary atresia. Indian J Pathol Microbiol 57:380. https://doi.org/10.4103/0377-4929.138722
Author information
Authors and Affiliations
Contributions
DK participated in the planning, conducting of the study, interpretation of data, collection, and writing of manuscript. HU contributed to interpretation and critically reviewed the manuscript. All the authors approved the final submitted draft of this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests that are relevant to the content of this article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent to participate in the study was obtained from the parents of all individual participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kato, D., Uchida, H., Amano, H. et al. Laparoscopic revision of Kasai portoenterostomy after initial laparoscopic portoenterostomy in patients with biliary atresia: a limited but positive effect on native liver survival. Pediatr Surg Int 38, 1821–1827 (2022). https://doi.org/10.1007/s00383-022-05235-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-022-05235-7