Abstract
Background
Most liver resections are currently performed using an open approach. Robotic hepatectomy has been suggested as a safe and effective approach for hepatocellular carcinoma; however, studies regarding oncological and surgical outcomes are still limited. Accordingly, we performed this study to compare the surgical and oncological outcomes between robotic and open approaches.
Methods
Between June, 2013 and July, 2016, a total of 63 HCC patients undergoing robotic hepatectomy, and 177 patients undergoing open hepatectomy were included in this study to assess the surgical and oncological outcomes after hepatectomy. The data of demographic, clinical features, hepatitis profile, tumor characters, TNM stage, surgical type, pathological outcomes, and postoperative results were collected prospectively and analyzed retrospectively.
Results
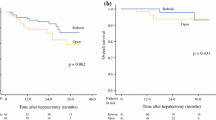
The demographic and clinical features of patients with HCC in both groups were statistically comparable. The robotic group had longer operative times (296 ± 84 vs. 182 ± 51 min, p = 0.032). The postoperative complications rate was slightly lower in the robotic group (11.1 vs. 15.3%, p = 0.418). The rate of Ro resection was similar in both groups (93.7 vs. 96%, p = 0.56). The length of hospital stay was significantly shorter in the robotic group (6.21 ± 2.06 vs. 8.18 ± 6.99 days, p = 0.001). The overall recurrence rate of HCC was lower in the robotic group (27 vs. 37.3%, p = 0.140). The 1, 2, 3 year disease-free survival rates were 72.5, 64.3, and 61.6%, respectively, for the open group, while they were 77.8, 71.9, and 71.9%, respectively, for the robotic group, (p = 0.325). The 1, 2, 3 year overall survival rates were 95.4, 92.3, and 92.3%, respectively, for the open group, while they were 100, 97.7, and 97.7%, respectively, for the robotic group (p = 0.137).
Conclusion
Robotic surgery is a safe and feasible procedure for liver resection in selected patients. The oncological and surgical outcomes of robotic hepatectomy were comparable to open surgery. The robotic hepatectomy carried significantly shorter length of hospital stay.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Possible curative therapy for HCC includes liver resection, liver transplantation, and local ablation [1,2,3]. Resections remain the standard treatment of resectable HCC [4]. Open liver resection has traditionally been considered the gold standard procedure to treat HCC. Surgeons and patients, however, are interested in minimally invasive surgery. Minimally invasive liver surgery is associated with reduced postoperative pain, reduced postoperative complications, and lessened length of hospital stay, and improved cosmeses without compromising oncological outcomes [5,6,7,8].
Robotic hepatic resection is a growing option in the field of hepatic surgery with acceptable morbidity and mortality [9].
Currently, the robotic platform has controls and ergonomics that closely mimic the movements of open surgery; improved three-dimensional visualization, seven-degrees of freedom, and allowing for precise dissection and intracorporeal suturing, thus expanding the scope and complexity of cases compared to conventional laparoscopy [10,11,12].
The literature demonstrates that in properly selected patients, performed by surgeons trained in open and liver surgery that are skilled in minimally invasive techniques, robotic liver resection is a feasible and safe option [13, 14]. Many studies have been conducted to compare the clinical and oncological outcomes between robotic and laparoscopic approaches, Qiu et al. [15] drew the conclusion in a systematic review that robotic hepatectomy and laparoscopic hepatectomy both display similar safety, feasibility, and effectiveness for liver resection. However, the accuracy of robotic instruments even in a limited space can facilitate biliary reconstruction, while it is usually considered a significant obstacle to laparoscopy [16, 17] Lai et al. [18] demonstrated the robotic approach is an acceptable alternative to laparoscopic liver resection for hepatocellular carcinoma. With the potential advantage of robotic system in performing major hepatectomy and resection of tumor in difficult segments, robotic surgery may have an impact on the therapeutic strategy of HCC.
Most surgeons are still reluctant to adopt robotic liver surgery due to not only the complexity of the operation and the technical expertise required, but also concern about the capability for adherence to safe and oncologically appreciated resection [19, 20]. In this study, the surgical and oncologic outcomes are compared between robotic and open liver resection. We attempted to demonstrate that the robotic platform is safe and effective, does not compromise oncological outcome, and is a reasonable alternative when compared to the open approach.
Materials and methods
This is a retrospective review of previously collected data. This study was approved by the Institutional Review Board in this hospital. From June 2013 to July 2016, patients with primary, newly diagnosed HCC were selected for this study. Radiologic studies for HCC were reviewed in a multidisciplinary case management meeting held weekly.
Two hundred and two cases with primary HCC undergoing open hepatectomy; and 63 cases with primary HCC undergoing robotic hepatectomy were collected for this study.
The principles that we chose the patients to receive robotic liver resection were based on the following: (1) According to the consensus statements, 5 cm or less, located in peripheral liver segments II–VI. The international position on laparoscopic liver surgery: the Louisville statement, 2008 [4]. (2) Those who are willing to pay the expensive charge for robotic surgery. The charge is about USD 8000 for every robotic liver surgery. It is not covered by NHI (National Healthcare Insurance) in Taiwan. (3) There is no history of upper abdominal surgery which could cause severe adhesion around the liver and perihilar region.
These procedures were performed by two experienced surgeons. We excluded 15 cases with right lobectomy, two cases with right extended lobectomy in the open group to match with the type of liver resection of the robotic group; also excluded seven cases of TNM stage 3C and one case stage 4B in the open group to match with the TNM stage of the robotic group.
Finally, 177 HCC cases with open hepatectomy and 63 HCC cases with robotic hepatectomy were included in this study. The data of demographic preoperative clinical features, hepatitis profile, tumor character, TNM staging, surgical type, pathological results, and postoperative outcome were collected and analyzed. All the patients were followed up until June 30 2017; the follow-up period was 786.10 ± 248 days for the open group and 791.05 ± 323.48 days for the robotic group. All the robotic procedures were performed using the da Vinci S and Si surgical system (Intuitive surgical, Sunnyvale, CA, USA). Intraoperative ultrasound assessment was conducted with the laparoscopic ultrasound (Xario 100-PET-805LA, Toshiba, Tokyo) to localize the lesion and identify the resection margin. The type of liver resection was adopted according to the Brisbane 2000 classification [21]. Surgeons attempted to allow a 1 cm gross margin during tumor resection in both groups, with a R0 resection margin being defined as complete resection with histologically negative resection margin. Postoperative complications were recorded and classified according to the Clavien–Dindo system and major complication was defined as Clavien–Dindo classification ≥ 3 [22].
All patients were followed monthly for the first 6 months following the operation and then quarterly if no recurrence was found. Enrolled patients underwent tumor evaluation for efficacy by α-fetoprotein level and liver ultrasound on a bimonthly basis for both two groups. A suspected recurrence due to the above examination was confirmed by dynamic computed tomography or magnetic resonance imaging or if necessary, with tissue sampling.
Statistical analysis
The baseline characteristics of patients were expressed as mean standard deviation (M ± SD). The X2 test or Fisher’s exact test was used to compare the discrete variables. Student’s t test or one-way ANOVA was used to compare the continuous variables. The disease-free survival and overall survival rate of both groups were presented by Kaplan–Meier curve. A comparison of survival analysis was performed by the log-rank test. Independent risk factors analysis for HCC recurrence was assessed by multivariate Cox regression model. p < 0.05 was considered statistically significant. A statistical analysis was performed by using SPSS ver. 180 (SPSS, Chicago, IL, USA).
Results
The demographic and clinical features of patients with HCC in both groups were statistically comparable. No significant HCC characteristics difference were noted between the two groups including α-fetoprotein, hepatitis profiles, tumor location, tumor size, tumor number, TNM stage, and postoperative anti-viral treatment (Table 1).
The surgical outcomes and pathologic features are shown in Table 2. Most of the patients in the robotic group, however, underwent partial liver resection when compared to that of the open group (66.7 vs. 45.2%; p = 0.012). The operative time for robotic group was 296 ± 84 min, longer than the open group time of 182 ± 51 min (p = 0.032). The amount of blood loss was comparable (Robotic 206 ± 105 ml vs. open 267 ± 180 ml, p = 0.724) in both groups. Fifty-eight (93.7%) out of 63 robotic liver resections were Ro resection, comparable to the open group (96%) (p = 0.361). The resection margin was also comparable in both groups (open 6.38 ± 6.79 mm vs. robotic 5.85 ± 5.15 mm, p = 0.586). The pathologic results, including histological grade, microscopic vascular invasion, satellite nodule, and Ishak’s score were all equivalent in both groups (p > 0.05). The most common histological grading was grade 2 (robotic 76.2 vs. open 73.4%).
The postoperative complications rate was slightly higher in the open group, not statistically significant (15.3% open vs. 11.1% robotic, p = 0.418), while major complication rates were similar between the two groups (1.6% robotic vs. 2.6% open, p = 1.0). One (0.6%) case of hepatic failure and 4 (2.3%) cases of bile leakage occurred in the open group, while 1 (1.6%) case in the robotic group needed endoscopic retrograde biliary drainage (ERBD) (Table 3).
The length of hospital stay was significantly shorter for the robotic group than the open group (6.21 ± 2.06 day vs. 8.16 ± 6.99 days, p = 0.001).
The robotic group had better short-term oncological outcomes, although it did not reach statistically significant difference. During the follow-up period, 17 (27%) cases of the robotic group were found to have HCC recurrence, as did 66 (37.3%) cases for the open group (p = 0.140).
Time to HCC recurrence was also comparable between the two groups (robotic 585.40 ± 353.06 days vs. open 540.08 ± 315.80 days; p = 0.346). The difference of survival period was not statistically significant, although the robotic group had longer survival time (760.47 ± 317.94 days vs. 686.89 ± 271.81 days, p = 0.115). Most of the recurrence of HCC occurred in the liver itself; however, there was neither recurrence on the surgical stump nor the port site. The location of recurrence was also similar in both groups (Table 4). The 1, 2, 3 year disease-free survival rates were 77.8, 71.9, and 71.9%, respectively, for the robotic group, while it was 72.5, 64.3, and 61.6%, respectively, for the open group (p = 0.325) (Fig. 1). The 1, 2, 3 year overall survival rate was 100, 97.7 and 97.7%, respectively, for the robotic group and 95.4, 92.3, and 92.3%, respectively, for the open group (p = 0.37) (Fig. 2). No conversion to open or laparoscopic approach was necessary in the robotic group, while no surgical mortality case was found in either group.
We performed risk factors analysis for HCC recurrence using Cox regression model in this study, the multivariate analysis showed that the independent risk factors for HCC recurrence were Child–Pugh classification B (HR = 5.89, p = 0.005 95% CI 1.712–20.307), presence of satellite module (HR = 2.46, p = 0.02 95% CI 1.409–4.286), and Ishak score 6 (HR = 1.942, p = 0.010 95% CI 1.175–3.207); while the TNM stage and surgical procedure (open vs. robotic) were not risk factors for HCC recurrence (Table 5).
Discussion
In this study, after matching with the type of liver resection and tumor stage, the demographic features, tumor characters, TNM stage, liver function, and hepatitis profile were similar in both groups and were statistically comparable (p > 0.05), although the case number was largely discrepant between the two groups.
Our comparisons showed that the robotic group had significantly longer operative time when compared with the open group (p = 0.0032). Longer operative time was also found in many investigations [23,24,25]. The robotic group requiring longer operative time could be caused by the requirement to dock the robot, exchange instruments, and dissect delicately under magnified views [26, 27].
Our experience demonstrated the safety profile of the two groups was comparable. Amount of blood loss and rates of major complications (Clavien–Dindo Classification IIIa or more) were similar. The reported complication rate of the robotic approach ranged from 10.9 to 22%. Our data were comparable with previous reports [28,29,30].
The R0 resection rate and resection margin were also equivalent in both groups in this study. The Ro resection rate for the robotic approach was 93.7% in this series, which is comparable with previous reports of 93 to 96% [18, 31, 32].
The commonly reported advantage of robotic liver resection when compared to open resection is shorter length of hospital stay [23, 25, 28, 32,33,34]. Our analysis confirmed the reports of significantly shorter length of hospital stay in comparison with the open group.
In our series, the pathologic outcomes, including histological grade, microvascular invasion, satellite nodule, and Ishak’s score were equivalent to that of open resection. These results were also consistent with a previous report [25]. The robotic group had a trend towards better disease-free and overall survival rates; however, the difference did not reach statistical significance. The disease-free survival rate was better in the robotic group vis-à-vis the open group, although the difference was not statistically significant (robotic 72.2 vs. open 61.6% at 3 year, p = 0.325); also, as was the overall survival rate (robotic 97.7 vs. open 92.3%, p = 0.137) in this study. These results were also consistent to the previous reports from Chen et al. [25] and Lai et al. [31].
Performance of a large liver resection can be done safely without mortality. Chen et al. [25] demonstrated more than half of their cases underwent major liver resection and among them, 15 cases had major liver resection for living-related liver donor.
However, in a study of case-matched comparisons, Kingham et al. [28], using the robotic approach, favored minor liver resection and demonstrated that a tumor in segment 7 was removed via a segment 7 wedge resection or segmentectomy, as opposed to a posterior section resection or even a right hepatectomy.
In the current study, 38% of HCC cases were located in the posterior and superior segment, 66.7% of cases underwent partial liver resection, and right lobectomy was never performed in the robotic group. This is a reflection of our patient’s population that is dominated by patients with HBV or HCV hepatitis and liver cirrhosis who need small parenchyma-preserving resections and careful patient selection.
In the recent literature, Kingham et al. [28] and Casciola et al. [34] demonstrated the feasibility and safety of parenchyma-sparing liver surgery using the robotic approach. There were a high number of non-anatomic wedge resections in the robotic group, suggesting that parenchyma preservation was upheld when using robotic technique [28, 35,36,37].
Wider surgical margin is not justified to prevent HCC recurrence [38]. Recent evidence supports change of a standard anatomical or major liver resection for HCC. Matsui et al. [39] demonstrated that limited resection with no margin did not affect the HCC recurrence and overall survival rates. Dahiya et al. [40] observed the extent of resection for HCC did not seem to affect HCC recurrence and long-term survival.
Recently, this trend has been enhanced by progress in ultrasound-guided liver resection, reducing the need for major hepatectomies even in complex situations such as tumor invasion of the hepatic vein [41]. In their study, Torzill et al. [42] concluded that the systematic use of intraoperative ultrasonography allowed sparing of the liver parenchyma without tumor recurrence and enabled safe operation while maintaining adequate oncological radicality and broadening the indication for surgery. In our series, intraoperative ultrasound-guided liver resection was done for every case in both groups, especially for HCC lesion located in posterior and superior segments. By this technique, parenchyma-preserving liver resection became more feasible and safe.
The limitations of this study included its retrospective basis, the small size series, and limited cases of major liver resection; however, it clearly shows the potential of robotic techniques vis-a-vis outcomes of open liver resection. We have demonstrated that robotic and open approaches appear similar in the important areas of surgical and oncological outcomes. As the experience grows, we believe additional advantages of the robotic platform will be demonstrated.
In conclusion, robotic surgery is a safe and feasible procedure for liver resection. The surgical and oncological outcomes are comparable between robotic and open hepatectomy, the robotic platform is effective, does not compromise oncological outcome, and is a reasonable alternative when compared to the open approach.
References
Forner A. Llovet JM, Bruix J (2012) Hepatocellular carcinoma. Lancet 379:1245–1255
Bruix J, Sherman M, American Association for the Study of Liver Diseases (2011) Management of hepatocellular carcinoma: an update. Hepatology 53: 1020–1022
Rahbari NN, Mehrabi A, Mollberg NM, Muller SA, Koch M, Buchler MW, Weitz J (2011) Hepatocellular carcinoma: current management and perspectives for the future. Ann Surg 253:453–469
Buell JF, Cherqui D, Geller DA, O’Rourke N, Iannitti D, Dagher I, Koffron AJ, Thomas M, Gayet B, Han HS, Wakabayashi G, Belli G, Kaneko H, Ker CG, Scatton O, Laurent A, Abdalla EK, Chaudhury P, Dutson E, Gamblin C, D’Angelica M, Nagorney D, Testa G, Labow D, Manas D, Poon RT, Nelson H, Martin R, Clary B, Pinson WC, Martinie J, Vauthey JN, Goldstein R, Roayaie S, Barlet D, Espat J, Abecassis M, Rees M, Fong Y, McMasters KM, Broelsch C, Busuttil R, Belghiti J, Strasbery S, Chari RS (2009) The international position on laparoscopic liver surgery: the Louisville Statement 2008. Ann Surg 250:825–830
Clinical Outcomes of Surgical Therapy Study G (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350: 2050–2059
Guillou PJ, Quirke P, Thorpe H et al (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASPCC trial): multicentre, randomized controlled trial. Lancet 36:1718–1726
Martek G, Boushey RP (2006) Laparoscopic colon surgery: past, present and future. Surg Clin North Am 86:867–897
Jayne DG, Guillou PJ, Thorpe H et al (2007) Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol 25:3061–3068
Giulianotti PC, Coratti A, Angelini M et al (2003) Robotic in general surgery: Personal experience in a large community hospital. Arch Surg 138:777–784
Diana M, Marescaux J (2015) Robotic surgery. Br J Surg 102:e15–e28
Giulianotti PC, Coratti A, Sbrana F, Addeo P, Bianco FM, Buchs NC, Annechiarico M, Benedetti E (2011) Robotic liver surgery: results for 70 resections. Surgery 149:29–39
Bagante F, Spolverato G, Strasgerg SM, Gan Fi, Thompson V, Hall BL, Bentrem DJ, Pitt HA, Pawlik TM (2016) Minimally invasive vs. open hepatectomy: a comparative analysis of the national surgical quality improvement program database. J Gastronintest Surg 20:1608–1617
Tranchart H, Ceribelli C, Ferreti S, Dagher I, Patriti A (2014) Traditional versus robot-assisted full laparoscopic liver resection: a matched-pair comparative study. World J Surg 38:29.4–29.9
Croner RS, Perrakis A, Hohenberger W, Brunner M (2016) Robotic liver surgery for minor hepatic resections: a comparison with laparoscopic and open standard procedures. Langenbecks Arch Surg 401:707–714
Qiu J, Chen S, Chengyou D (2016) A systematic review of robotic-assisted liver resection and meta-analysis of robotic versus laparoscopic hepatectomy for hepatic neoplasms. Surg Endosc 30:862–875
Bonapasta SA, Bartomini I, Checcacci P, Guerra F, Coratti A (2015) Indications for liver surgery: laparoscopic or robotic approach. Surg 67:117–122
Nguyen KT, Gamblin TC, Geller DA (2009) World review of laparoscopic liver resection-2804 patients. Ann Surg 250:831–884
Lai EC, Tang CN (2016) Long-term survival analysis of robotic versus conventional laparoscopic hepatectomy for hepatocellular carcinoma: a comparative study. Surg Laparosc Endosc Percutan Tech 26:162–166
Ocuin LM, Tsung A (2015) Robotic liver resection for malignancy: current status, oncologic outcomes, comparison to laparoscopy and future applications. J Surg Oncol 112:295–301
Ho CM, Wakanayahi G, Nitta H, Itl N, Hasegawa Y, Takahara T (2013) Systematic review of robotic liver resection. Surg Endosc 27:732–739
Strasberg SM (2005) Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg 12:351–355
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann surg 240:205–213
Morel P, Jung M, Cornateanu S, Buehler L, Majno P, Toso C, Buchs NC, Rubbia-Brandt L, Hagen ME (2017) Robotic versus open liver resections: a case-matched comparison. Int J Med Robot. https://doi.org/10.1002/rcs.1800 (Epub ahead of print)
Sham JG, Richards MK, Seo YD, Pillariaetty VG, Yeung RS, Park JO (2016) Efficacy and cost of robotic hepatectomy: is the robotic cost-prohibitive? J Robotic Surg 10:307–313
Chen PD, Wu CY, Hu RH, Chou WH, Lai HS, Liang JH, Lee PO, Wu YM (2017) Robotic versus open hepatectomy for hepatocellular carcinoma: a matched comparison. Ann Surg Oncol 24:1021–1028
Anvari M, Birch DW, Bamehriz F, Gryfe R, Chapman T (2004) Robotic-assisted laparoscopic colorectal surgery. Surg Laparosc Endosc Percutan Tech 14:311–315
Hanly EJ, Talamini MA (2004) Robotic abdominal surgery. Am J Surg 188:19S–26S
Kingham TP, Leung U, Kuk D, Gonen M, D’Angelica M, Allen P, DeMatteo R, Laudone VP, Jarnagin WR, Fong Y (2016) Robotic liver resection: a case-matched comparison. World J Surg 40:1422–1428
Patriti A, Cipriani F, Ratti F, Bartoli A, Ceccarelli G, Casciola L, Aldrighetti L (2014) Robotic-assisted versus open liver resection in the right posterior section. JSLS 18:1–6
Daskalaki D, Gonzalez-Heredia R, Brown M, Bianco FM, Tzvetanov I, Davis M, Kim J, Benedetti E, Giulianotti PC (2017) Financial impact of the robotic approach in liver surgery: a comparative study of clinical outcomes and costs between the robotic and open technique in a single institution. J Laparoendosc Adv Surg Tech 27:375–382
Lai E, Yang GC, Tang CN (2013) Robotic-assisted laparoscopic liver resection for hepatocellular carcinoma: short-term outcome. Am J Surg 205:697–702
Tsung A, Geller DA, Sukato DC, Sabbaghian S, Tohme S, Steel J, Marsh W, Reddy SK, Bartlett DL (2014) Robotic versus laparoscopic hepatectomy: a matched comparison. Ann Surg 259:549–555
Han DH, Choi SH, Park EJ, Kang DR, choi GH, Choi JS (2016) Surgical outcomes after laparoscopic or robotic liver resection in hepatocellular carcinoma: a propensity-score matched analysis with conventional open liver resection. Int J Med Robot 12:735–742
Casciola L, Patriti A, Ceccarelli G, Bartoli A, Ceribelli C, Spaziani A (2011) Robotic-assisted parenchymal-sparing liver surgery including lesions located in the posterosuperior segments. Surg Endosc 25:3815–3824
Roberto Montaliti R, Scuderi V, Patriti A, Vivarelli M (2016) Robotic versus laparoscopic resections of posterosuperior segments of the liver: a propensity score-matched comparison. Surg Endosc 30:1004–1013
Troisi R, Patriti A, Montalti R, Casciola L (2013) Robot assistance in liver surgery: a real advantage over a fully laparoscopic approach? Results of a comparative bi-institutional analysis. Int J Med Robot 9:160–166
Nota CL, Borel IH, Molenaar IQ, van Santvoort HC, Fong Y, Hagendoom J (2016) Robot-assisted laparoscopic liver resection: a systematic review and pooled analysis of minor and major hepatectomy. HBP 18:113–120
Lee KT, Wang SN, Chen HY, Shi HY, Ker CG, Chiu HC (2012) Is wider surgical margin justified for better clinical outcomes in patients with resectable hepatocellular carcinoma? J Formos Med Assoc 111:160–170
Matsui Y, Terakawa N, Satoi S, Kaibori M, Kitade H, Takai S, Kwon AH, Kamiyama Y (2007) Postoperative outcomes in patients with hepatocellular carcinomas resected with exposure of the tumor surface. Arch Surg 142:596–602
Dahiya D, Wu TJ, Lee CF, Chan KM, Lee WC, Chen MF (2010) Minor versus major hepatic resection for small hepatocellular carcinoma (HCC) in cirrhotic patients: a 20-year experience. Surgery 147:676–685
Torzilli G, Montorsi M, Donadon M, Palmisano A, Fabbro DD, Gambetti A, Olivari N, Makunchi M (2005) “Radical but conservative” is the main goal for ultrasonography-guided liver resection: prospective validation of this approach. J Am Coll Surg 201:517–528
Torzilli G, Montorsi M, Del Fabbro A, Palmisano M, Donadon, Makunchi M (2006) Ultrasonographically guided surgical approach to liver tumors involving the hepatic veins close to the caval confluence. Br J Surg 93:1238–1246
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Authors Wen-Hsiuan Wang, Kung-Kai Kuo, Shen-Nien Wang, King-Teh Lee have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, WH., Kuo, KK., Wang, SN. et al. Oncological and surgical result of hepatoma after robot surgery. Surg Endosc 32, 3918–3924 (2018). https://doi.org/10.1007/s00464-018-6131-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6131-2