Abstract
Robotic liver surgery has been considered as a unique opportunity to overcome the traditional limitations of laparoscopy; thus, it can potentially extend the indications of minimally invasive liver surgery. From April 2015 to May 2017, 35 patients underwent fully robotic left hepatectomy. The mean operative time was 315 min (200–445 min) and the mean estimated blood loss was 245 ml (125–628 ml). Pringle maneuver was required in six cases. Cancer was the indication for surgery in all patients (14 liver metastases, 18 hepatocellular carcinomas and 3 cholangiocarcinomas). There were one to four lesions in a patient and the mean lesion size was 39.2 mm (15–85 mm). The average length of hospital stay was 6.5 days (5–14 days). Perioperative morbidity rate was 17.2%. Two patients underwent conversion to open surgery. The 90-day mortality rate was nil. The mean surgical resection margin was 12 (1–22) mm, and R0-resection was reached in 33 out of 35 cases. The robotic left hepatectomy provides interesting surgical outcomes and good oncologic adequacy. It can be safely applied for the management of liver malignancies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Laparoscopic surgery in liver is considered to be technically demanding mainly due to compromised dexterity, physiologic tremors and limited degrees of motion. These result in a steep learning curve and eventually limit the laparoscopic liver surgery to be applied mainly in centers with important experience in both liver and laparoscopic surgery [1].
Several meta-analyses have confirmed that laparoscopic liver surgery offers some benefits regarding the short-term results in comparison to the open technique in terms of blood loss, need for blood transfusion, length of stay and complication rates (both medical and surgical) without compromising the oncologic adequacy [2, 3]. Other meta-analyses which focused on the laparoscopic approach for the resection of hepatocellular carcinoma demonstrated that a rate of positive margins was found to be lower for the laparoscopic group, while overall and disease-free survival outcomes were equal to open approach [4]. Unfortunately, considering the complexity of the procedures, these studies are limited to single-institution case series performed in selected groups of patients which reduce the reproducibility of the above findings. In the I Go MILS (Italian Group of Minimally Invasive Liver Surgery) Registry, data from 1678 minimally invasive liver procedures have been collected to monitor the development and implementation of this surgical approach, but major liver resection constituted only 10% of the series underscoring the challenges of a total laparoscopic major hepatectomy and the complexity of laparoscopic approach for unfavorable tumor location [5].
In this scenario, the robotic surgery due to 3D stereoscopic view, improved dexterity, seven degrees of freedom, elimination of physiologic tremors and favorable ergonomic position can enhance the indication for MIS liver resections and help to overcome the difficulties of laparoscopic approach. The possibility to suture a bleeding vessel or to perform complex hilar dissection and liver resection requiring bilio-enteric reconstruction was crucial for the progressive acceptance of robotic approach.
Unfortunately, although the safety and feasibility of robotic liver resection have been demonstrated [6], the second consensus conference in Morioka in 2014 defined robotic liver surgery as “a development in progress” due to the lack of data necessary for the evaluation and due to the smaller range of instruments available in comparison to laparoscopic or open techniques [7].
To date, only few case series reported robotic major hepatic resection, most of them including different surgical procedures (right, left or extended hepatectomies) and for indications including both benign and malignant tumors.
Herein, we demonstrate our experience in robotic liver surgery describing left hepatectomy procedure.
Methods
We retrospectively reviewed our prospective database of robotic liver surgery. From April 2015 to May 2017, 35 patients underwent robotic-assisted left hepatectomy at Villa Sofia and University Hospital of Palermo (Italy).
All clinical cases were discussed at a preoperative multidisciplinary meeting conference, during which we evaluated the feasibility of MIS treatment. All patients with a preoperative diagnosis or suspicion of malignant lesions of left liver lobe were considered eligible for robotic approach. Lesions with the extensive subcapsular involvement or those invading the major vessels (portal vein branches, inferior vena cava or hepatic veins), or with extensions into the diaphragm were non-eligible for robotic approach. A Child–Pugh score other than A was considered contraindication as well. The size of the lesions was not considered as an obstacle to the robotic approach. All patients requiring simultaneous surgical procedures in other organs were excluded from the study. The contraindications for robotic approach are listed in Table 1.
Left hepatectomy was defined as a resection of segments 2, 3 and 4 of the liver. In patients with metastatic disease of the liver, the operation was indicated when more limited resection of the liver parenchyma was not possible for anatomical reasons.
The preoperative work-up included whole-body contrast-enhanced computed tomography (CT), liver gadoxetic acid-enhanced magnetic resonance imaging (MRI), tumor markers, and routine blood examination; the estimated residual liver function was based on the retention rate of indocyanine green (ICG) 15 min after administration. The complications were classified according to the Clavien–Dindo score. Surgical resection margins were considered negative when no tumor was evident along the transection surface.
After the explanation of the robotic technology a written informed consent was signed by all patients. Two surgeons, experts both in open and laparoscopic hepato-pancreato-biliary (HPB) surgery performed all operations employing the Da Vinci Si Surgical System (Intuitive Surgical Inc., Sunnyvale, CA, USA).
A follow-up consultation was scheduled at 1 and 6 months after surgery and yearly thereafter, performing a blood test examination, liver ultrasound and total body CT scan. Additionally, an MRI was performed at 1 year.
Operative technique
The patient is placed in a supine, 15° reverse-Trendelenburg position with legs apart and arms tucked along the body; the table is slightly tilted to the right side where the ultrasound system is located. The scrub nurse also stands at the right side of the patient, while the assistant surgeon is positioned between the patient’s legs. The robotic surgeon operates from the console located in a corner of the operating room. The pneumoperitoneum is induced through a Veress needle inserted in the Palmer’s point, and the abdomen is insufflated until reaching 12 mmHg. The central venous pressure is maintained low (5 cm H2O) during the entire procedure.
We employed five trocars: four robotic and one laparoscopic, with the following disposition (Fig. 1):
-
OPT. 12 mm port is placed above the umbilicus for the 30º camera scope.
-
R1: 8 mm port is located in the right flank along the right anterior axillary line
-
R2: 8 mm port is located in the left pararectal area along the left mid-clavicular line
-
R3: 8 mm port is located in the left flank along the left anterior axillary line
-
ASS: 12 mm assistant port is introduced in the right pararectal area.
Robotic arm 1 corresponding to the surgeon’s right hand manipulates the monopolar curved scissors, while in the robotic arm 2 we insert the Maryland Bipolar forceps. The robotic arm 3, used mostly as a stable retractor, is armed with Cadiere Forceps.
During the procedure we employ a needle holder for suturing and robotic Hem-o-lock clips (Weck, Teleflex Inc.) to achieve hemostasis and vascular control.
We perform an intraoperative ultrasound (IOUS) of the liver employing the ProART Robotic Transducer Type 8826 (BK Medical APS, Peabody, MA) manipulated by the robotic grasper (ProGrasp Forceps, Intuitive Surgical Inc., Sunnyvale, CA) to evaluate the number, size and location of the lesions and define the operative strategy. The patient cart of the Da Vinci system is docked directly over the head of the patient.
First step: we mobilize the left liver lobe dividing the round, falciform and left triangular ligaments up to left hepatic vein. Afterwards, while the third robotic arm lifts up the inferior surface of the liver through a protective gauze; the hepatic pedicle is encircled by inserting the EndoWrist Cadiere Forceps and passing a vessel loop for the Pringle maneuver. The hepatic hilum dissection with employment of the Maryland forceps and monopolar scissors is started and if present, an accessory left hepatic artery of Hyrtl must be identified and ligated in the lesser omentum.
During the dissection of the hepato-duodenal ligament, the left hepatic artery is visualized and tractioned towards the right side with a vessel loop, exposing the left branch of the portal vein. Thus, the portal branch is dissected and both left branches are clamped in to observe a demarcation line on the liver surface. The artery is clipped and divided as well as the left branch of the portal vein (Fig. 2).
Comment: the liver ultrasonography has to be performed once the falciform ligament has been cut, while the caval confluence should not be exposed to avoid artifacts at IOUS. Generally, we do not use Ultracision Harmonic shears during the hepatic hilum dissection, even if it can be a valid option in case of complex or unclear anatomy. We tend to prefer monopolar hook.
A cost-effective system for Pringle maneuver described by Patriti et al. consists of a 20-French chest tube, an umbilical tape and a plug used for occlusion of the Foley catheter. When the inflow occlusion is needed, the on-table surgeon removes the plug and pulls the umbilical tape [8]. Considering the lack of tactile feedback, a direct traction of the vessels with the robotic instrument should be avoided in favor of a selective dissection and control of each vascular structure which allows a safer exposure.
Second step: the transection line is marked using the monopolar scissors and the parenchymal transection is performed employing the Harmonic Shears and Maryland forceps alternatively, with placement of the figure-of-eight stitches using 0-size absorbable sutures on the left edge of the transection line to perform a wide exposure (Fig. 3). Large venous branches of S4 are controlled selectively using robot-sewn ligation with Vicryl® or clipped by Hem-o-lock® clips and then cut; the left hepatic biliary duct is clipped and divided intraparenchymally. This step is especially important in cirrhotic patients as tissue surrounding the biliary confluence is heavily inflammated in these patients.
Comment: a “rubber band technique” is a valid option to achieve a steady exposure of a straight transection plane. Two bands are introduced in the abdominal cavity, one end is anchored at the left and right resection margins and meanwhile the other end is retracted and fixed outside the abdominal cavity through two additional 2 mm trocarts. The Kelly crush-clamp technique helps to fragmentize the liver preserving the vascular structures and to avoid the systematic use of advanced energy as Harmonic ACE. Further, its wristed capability allows making a curved transection line. In conclusion, the parenchymal transection remains a wicked step of the robotic procedure; we suggest a meticulous progression going layer by layer to the core of liver, exposing the transection line with a calibrate traction and use the Harmonic ACE as vibrating tool whose jaws should met the vessels at 90° angle to reach the best effectiveness.
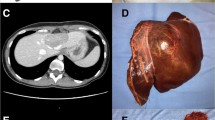
Third step: the left hepatic vein is visualized and divided using a 45-mm vascular load stapler inserted through the 12-mm assistant port (Fig. 4); finally the specimen is inserted in an EndoBag and placed on the right liver surface.
The hemostasis and biliary leak control is achieved; fibrin glue is placed on the resection surface. A drain is inserted below the liver through the Winslow foramen and the specimen is extracted through a Pfannenstiel incision.
Comment: a hanging maneuver can be useful before the transection of the last part of the liver parenchyma surrounding the left hepatic vein [9]. In case of tumor that does not compress left hepatic vein, it is possible to achieve an extrahepatic hepatic vein control using the surgical approach trough ligamentum venosum.
Results
Among 35 patients undergoing robotic left hepatectomy, 22 (62.8%) were males. The mean age was 63.8 years (42–77 years) and the mean BMI was 23.5 kg/m2. Twenty patients (57.1%) were scored as ASA 2. The demographic characteristic is illustrated in Table 2.
The mean operative time was 315 min (200–445 min) and the mean estimated blood loss was 245 ml (125–628 ml). None of the patients required intraoperative blood transfusion. The intraoperative characteristics are depicted in Table 3.
A Pringle maneuver was required in 6 (17%) of patients for a mean of 12.5(5–34) min.
The indications for surgery were: liver metastases (14 patients), HCC (18 patients) and cholangiocarcinoma (3 patients). The mean number of lesions was 1.85 (range 1–4 lesions) and the mean lesion size was 39.2 mm (15–85 mm). A single lesion was detected in 24 out of 35 patients.
The average length of hospital stay was 6.5 (5–14 days), while the morbidity rate was 6/35 (17.2%). Half of the complications were classified as minor and spontaneously solved within the first week as confirmed by monitoring the liver text function in case of liver transient failure observed in patients who underwent to preoperative CHT (chemotherapy) or through chest X-ray in a patient who experimented a pleural effusion.
The major complications were as follows: a biliary leak detected at postoperative day 4 after liver ultrasound and percutaneous biliary drainage (PTC) and finally treated by ERCP (endoscopic retrograde cholangiopancreatography); abdominal collection, in a patient who required a readmission and US-guided percutaneous drainage; a bowel perforation diagnosed at postoperative day 3 in a patient who underwent a colonic resection at postoperative day 5 (Table 4).
Two patients required conversion to open surgery for a bleeding arising form MHV. No 90-day mortality event was registered.
The mean surgical resection margin was 12 (1–22) mm, and we achieved the R0-resection rate in 33 cases. Patients were followed-up of for a mean of 31.5 months. During the follow-up, three patients developed recurrent disease and died at 18, 22 and 26 months after surgery. In the first case, a patient who at admission had four colorectal metastases in the left liver manifested with a new colorectal metastasis in the right lobe (segment 7) being further treated by radiofrequency ablation. In the second case, a patient developed another hepatocellular carcinoma of 2.5 cm with the localization of a new lesion in the caudate lobe; in this regard, a robotic-isolated caudate lobe resection was performed—the experimented exitus for peritoneal carcinomatosis. The last case was a systemic recurrence involving both lungs. The 3-year disease-free survival for the analyzed group at 3 years is 65.5%; meanwhile the overall survival was 86%. One patient was lost to follow-up.
Discussion
The robotic liver surgery is progressively gaining attention from surgical community. A recent review of 29 studies suggests that despite the longer operative time, the robotic-assisted hepatic resection is a feasible, safe and effective technique with an acceptably morbidity (11.36%) [10]. As shown in the experience of a Taiwan group, it was possible to increase the case number of minimally invasive liver resections by two-fold for patients with fresh HCC during their robotic experience, at the same time the percentage of major robotic hepatectomy has risen from 15 to 44% with a conversion rate (6%) and morbidity rate (8%) comparable to those of laparoscopic approach [11]. This technology provides higher feasibility and improved outcomes in more complex liver procedures such as biliary reconstruction [12]. At the same time, some concerns still persist regarding the lack of tactile feedback in robotic surgery. Laparoscopy seems to give the opportunity to have a better assessment in case of small metastasis or nodules located in a cirrhotic parenchyma, but as confirmed by our findings, we achieved a good oncologic adequacy nevertheless our initial experience.
As concluded by an updated review, most of the minimally invasive hepatectomies are non-anatomical resections, and consequently, considering the comparable surgical outcomes and the longer operative time, the use of expensive surgical instruments does not seem to be justified [13]. The number of major hepatectomies reported in the literature is in fact limited, representing the 47% of total robotic liver cases [10].
As showed by Packiam et al. and Kim et al., for the left lateral sectionectomy, there were no differences in perioperative outcomes, but the operating time was longer in robotic compared to laparoscopic liver surgery; furthermore, the robotic costs were significantly higher than laparoscopic ($8183 vs $5190). Therefore, the authors concluded that robotic approach should be mainly implemented in complex cases [14, 15].
Although only a few series addressed the issue of major hepatectomies, the robotic approach for these procedures not only seems to be feasible, but also provides an enhanced control of the operative field. Our findings in terms of mean operative time (315 min), estimated blood loss (245 ml), length of stay (6.5 days) and morbidity rate (17.2%) were similar to the data previously published by expert authors confirming that a good training program and patient selection are the key points in the initial phase of the learning curve [11, 16,17,18,19,20].
In contrast with the previously mentioned series, we have investigated a cohort of patients who underwent left robotic hepatectomy only for malignant disease to avoid the possible clinicopathological effects on surgical outcomes. The encouraging results observed in this paper can improve the applications of this technology for the malignant pathologies.
In our initial experience, we have recognized the importance of the appropriate tissue manipulation and management of the intraoperative complications (such as bleeding control) that can occur during a complex procedure. The type of complications we have seen in our series was similar to those reported in the literature [10]. The Endo-wristed instrumentation helped us to achieve an extraparenchymal selective control over the portal pedicle without a systematic use of the intermittent Pringle maneuver as demonstrated in the experience of Pesi et al. [21].
The outcomes of robotic liver resection presented in the literature are similar to laparoscopic surgery. It is especially interesting if we bare in mind that we are investigating a new, recently adopted technology.
The robotic approach offers an enhanced feasibility in challenging settings potentially increasing the percentage of major hepatectomies to be performed in a purely mini-invasive fashion also in patients with cirrhotic liver disease [22]. It also gives the opportunity to approach the unfavorable tumor location (postero-superior segments) and to perform an atypical resection with angulated transection line avoiding the unnecessary straight-line right hepatectomy [23].
The initial experiences of robotic-assisted partial caudate lobe resection confirm the advantages of the technique on short-term outcomes in comparison to laparoscopic approach advocating the indication of MIS technique even in anatomically challenging areas [24].
As previously reported, the dual console and the robotic simulator can be helpful in improving the skill and competence of a young surgeon, as well as in involving the trainees in more complex steps of the procedure when some tasks are performed under the supervision [25, 26].
A recent study has reported a three-phase learning curve in robotic hepatectomy each composed of 15, 25 and 52 cases; with a clear operative time and length of stay reduction after the initial stage. The authors suggest a shorter learning curve for robotic surgery than for laparoscopy [27].
The further implementation of the robotic platform with Indocyanine Green (ICG) fluorescence and augmented reality can lead to better outcomes. For example TilePro™ software (Intuitive Surgical Inc., Sunnyvale, CA) includes multiple data sources into the robotic operative view providing the surgeon a more reliable system to integrate all anatomical data.
The US probe can overcome the lack of tactile feedback, the use of ICG can help surgeon to recognize vascular and biliary anatomy, differentiate the hepatic lesions according to their vascular pattern, thus increasing the safety of the procedure and the accuracy of lesion detection [28].
In conclusion, robotic liver surgery still has important limitations mainly regarding the lack of specific instruments and we believe an international register database is required to have a wider perception of its impact on surgical outcomes.
Despite those limitations, the evolution of robotic system is continuing. This platform in fact allows sharing and integrating the information from different sources enabling a real-time image-guided surgery, and thus representing a fundamental step toward a safer and more efficient technique.
The massive use of robotic surgery for all kinds of HPB procedures is not cost-effective. On the other hand the establishment of high-volume centers with specialized robotic units and training of dedicated operating room staff increases the effectiveness of the multidisciplinary robotic approach. A rise in the use of the technique can break down the cost and change the future scenario. The industry competition may provide the reduction of the instrumentation price, but until that time one important question we should ask to ourselves: should we limit implementation of robotic platform only because of its higher cost? The results presented in this paper seem to confirm some important benefit of this approach without giving the decisive answer.
References
Komorowski AL, Mituś JW, Wysocki WM, Bała MM (2017) Laparoscopic and open liver resection—a literature review with meta-analysis. Arch Med Sci 13(3):525–532
Sotiropoulos GC, Prodromidou A, Kostakis ID, Machairas N (2017) Meta-analysis of laparoscopic vs open liver resection for hepatocellular carcinoma. Updates Surg 69(3):291–311
Mirnezami R, Mirnezami AH, Chandrakumaran K, Abu Hilal M, Pearce NW, Primrose JN, Sutcliffe RP (2011) Short- and long-term outcomes after laparoscopic and open hepatic resection: systematic review and meta-analysis. HPB (Oxford) 13(5):295–308
Fancellu A, Rosman AS, Sanna V, Nigri GR, Zorcolo L, Pisano M, Melis M (2011) Meta-analysis of trials comparing minimally-invasive and open liver resections for hepatocellular carcinoma. J Surg Res 171(1):e33–e45
Aldrighetti L, Ratti F, Cillo U, Ferrero A, Ettorre GM, Guglielmi A, Giuliante F, Calise F, Italian group of minimally invasive liver surgery (I GO MILS) (2017) Diffusion, outcomes and implementation of minimally invasive liver surgery: a snapshot from the I Go MILS (Italian group of minimally invasive liver surgery) registry. Updates Surg 69(3):271–283
Milone L, Daskalaki D, Fernandes E, Damoli I, Giulianotti PC (2013) State of the art in robotic hepatobiliary surgery. World J Surg 37(12):2747–2755
Wakabayashi G, Cherqui D, Geller DA et al (2015) Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 261(4):619–629
Patriti A, Ceccarelli G, Bartoli A, Casciola L (2011) Extracorporeal Pringle maneuver in robot-assisted liver surgery. Surg Laparosc Endosc Percutan Tech 21(5):242–244
Nanashima A, Nagayasu T (2016) Development and clinical usefulness of the liver hanging maneuver in various anatomical hepatectomy procedures. Surg Today 46(4):398–404
Qiu J, Chen S, Chengyou D (2016) A systematic review of robotic-assisted liver resection and meta-analysis of robotic versus laparoscopic hepatectomy for hepatic neoplasms. Surg Endosc 30(3):862–875
Wu YM, Hu RH, Lai HS, Lee PH (2014) Robotic-assisted minimally invasive liver resection. Asian J Surg 37(2):53–57
Chen KH, Chen SD, Chen YD, Chang YJ, Lin TC, Siow TF, Chio UC, Huang SY, Wu JM, Jeng KS (2014) Robotic left hepatectomy with revision of hepaticojejunostomy. Asian J Surg 37(2):106–109
Memeo R, Pisopiso V (2017) Present and future in robotic hepatectomies. Ann Laparosc Endosc Surg 2:98
Packiam V, Bartlett DL, Tohme S, Reddy S, Marsh JW, Geller DA, Tsung A (2012) Minimally invasive liver resection: robotic versus laparoscopic left lateral sectionectomy. J Gastrointest Surg 16(12):2233–2238
Kim JK, Park JS, Han DH, Choi GH, Kim KS, Choi JS, Yoon DS (2016) Robotic versus laparoscopic left lateral sectionectomy of liver. Surg Endosc 30(11):4756–4764
Tsung A, Geller DA, Sukato DC, Sabbaghian S, Tohme S, Steel J, Marsh W, Reddy SK, Bartlett DL (2014) Robotic versus laparoscopic hepatectomy: a matched comparison. Ann Surg 259(3):549–555
Giulianotti PC, Coratti A, Sbrana F, Addeo P, Bianco FM, Buchs NC, Annechiarico M, Benedetti E (2011) Robotic liver surgery: results for 70 resections. Surgery 149(1):29–39
Spampinato MG, Coratti A, Bianco L, Caniglia F, Laurenzi A, Puleo F, Ettorre GM, Boggi U (2014) Perioperative outcomes of laparoscopic and robot-assisted major hepatectomies: an Italian multi-institutional comparative study. Surg Endosc 28(10):2973–2979
Choi GH, Choi SH, Kim SH, Hwang HK, Kang CM, Choi JS, Lee WJ (2012) Robotic liver resection: technique and results of 30 consecutive procedures. Surg Endosc 26(8):2247–2258
Lai EC, Yang GP, Tang CN (2013) Robot-assisted laparoscopic liver resection for hepatocellular carcinoma: short-term outcome. Am J Surg 205(6):697–702
Pesi B, Moraldi L, Bartolini I, Tofani F, Guerra F, Annecchiarico M, Coratti A (2018) Pringle maneuver in robotic liver surgery: preliminary study. Minerva Chir. https://doi.org/10.23736/S0026-4733.18.07599-5
Chen PD, Wu CY, Hu RH, Chou WH, Lai HS, Liang JT, Lee PH, Wu YM (2017) Robotic versus open hepatectomy for hepatocellular carcinoma: a matched comparison. Ann Surg Oncol 24(4):1021–1028
Boggi U, Caniglia F, Vistoli F, Costa F, Pieroni E, Perrone VG (2015) Laparoscopic robot-assisted resection of tumors located in posterosuperior liver segments. Updates Surg 67(2):177–183
Lai EC, Tang CN (2014) Robot-assisted laparoscopic partial caudate lobe resection for hepatocellular carcinoma in cirrhotic liver. Surg Laparosc Endosc Percutan Tech 24(3):e88–e91
Marino MV, Shabat G, Potapov O, Gulotta G, Komorowski AL (2018) Robotic pancreatic surgery: old concerns, new perspectives. Acta Chir Belg 8:1–8
Marino MV, Shabat G, Guarrasi D, Gulotta G, Komorowski AL (2018) Comparative study of the initial experience in performing robotic and laparoscopic right hepatectomy with technical description of the robotic technique. Dig Surg. https://doi.org/10.1159/000487686
Chen PD, Wu CY, Hu RH, Chen CN, Yuan RH, Liang JT, Lai HS, Wu YM (2017) Robotic major hepatectomy: is there a learning curve? Surgery 161(3):642–649
Giulianotti PC, Bianco FM, Daskalaki D, Gonzalez-Ciccarelli LF, Kim J, Benedetti E (2016) Robotic liver surgery: technical aspects and review of the litterature. Hepatobiliary Surg Nutr 5(4):311–321
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare they have no conflict of interest or disclosures.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
An informed consent was obtained from all patients involved in the study.
Rights and permissions
About this article
Cite this article
Marino, M.V., Gulotta, G. & Komorowski, A.L. Fully robotic left hepatectomy for malignant tumor: technique and initial results. Updates Surg 71, 129–135 (2019). https://doi.org/10.1007/s13304-018-0560-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-018-0560-2