Abstract
Background
Laparoscopic fundoplication is an accepted surgical management of refractory gastro-esophageal reflux disease (GERD). The use of high resolution esophageal manometry (HRM) in preoperative evaluation is often applied to determine the degree of fundoplication to optimize reflux control while minimizing adverse sequela of postoperative dysphagia.
Objective
Assess the role of preoperative HRM in predicting surgical outcomes, specifically risk assessment of postoperative dysphagia and quality of life, among patients receiving laparoscopic Nissen fundoplication for GERD with immediate postoperative (< 4 weeks clinic), short-term (3-month clinic), and long-term (34 ± 10.4 months of telephone) follow-up.
Methods
Retrospective analysis of 146 patients over the age of 18 who received laparoscopic Nissen fundoplication at University of Vermont Medical Center from July 1, 2011 through December 31, 2014 was completed, of which 52 patients with preoperative HRM met inclusion criteria. Exclusion criteria included history of: (a) named esophageal motility disorder or aperistalsis; (b) esophageal cancer; (c) paraesophageal hernia noted intraoperatively.
Results
Elevated basal integrated relaxation pressure (IRP), which is the mean of 4 s of maximal lower esophageal sphincter (LES) relaxation within 10 s of swallowing, was significantly correlated with worsened severity of post-fundoplication dysphagia (r = 0.572, p < 0.0001 with sensitivity and NPV of 100%) and poorer quality of life (r = 0.348, p = 0.018) at up to 3-years follow-up. The presence of preoperative dysphagia was independently related to post-fundoplication dysphagia at short-term (r = 0.403, p = 0.018) and long-term follow-up (r = 0.415, p = 0.005). Also, both elevated mean wave amplitude (r=-0.397, p = 0.006) and distal contractile integral (DCI) (r = − 0.294, p = 0.047) were significantly, inversely correlated to post-Nissen dysphagia. No significant association was demonstrated between other preoperative HRM parameters and surgical outcomes.
Conclusions
Inadequacy of lower esophageal sphincter (LES) relaxation with swallowing as delineated by elevated IRP is significantly predictive of worse long-term postoperative outcomes including dysphagia and quality of life scores. Further assessment of tailoring anti-reflux surgical approach with partial vs. total fundoplication to functionally resistant LES is required.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Despite minimal perioperative morbidity and 30-day postoperative mortality of 0%, surgical fundoplication for reflux control is not without potential adverse outcomes [1]. In addition to the risk of postoperative epigastric pain, postprandial fullness, and increased flatulence with gas bloat, fundoplication is associated with an 8–12% incidence of dysphagia [2,3,4]. Post-fundoplication dysphagia rates at 3 months range from 10 to 40% with long-term rates of up to 10% at 1 year [5,6,7]. The clinical implications of dysphagia following anti-reflux surgery have extensive effects on quality of life outcomes, often resulting in significant weight loss, malnutrition, reoperation rates of 1.8–10.8%, and endoscopic dilatation rates of 0–25% [1]. Persistent dysphagia is rarely due to excessively tight wrap formation and often attributable to recurrent reflux, esophageal stenosis, development of paraesophageal hernia, and wrap migration into the thorax which has a reported incidence of 0.8–26% [1, 8, 9]. Furthermore, it is also possible that long-term dysphagia after anti-reflux surgery is a result of esophageal dysmotility in those who have normal postoperative anatomy.
Multiple surgical modifications have been reported to reduce the incidence of adverse postoperative outcomes which include larger bougie caliber during wrap sizing, shortening the length of fundoplication wrap, and mobilization of the short gastric vessels [1, 10,11,12,13]. However, esophageal function might also be an important predictor of long-term dysphagia after anti-reflux surgery. Current literature does not support the routine use of mandatory preoperative manometry, yet the novel metrics of high resolution manometry (HRM) are often applied to examine preoperative esophageal gastric junction (EGJ) anatomy and esophageal motility [1, 5]. Whereas conventional manometry applies 4–8 sensors spaced at 3–5 cm intervals, HRM uniquely utilizes 36 circumferential sensors spaced at 1-cm intervals thus enabling a higher fidelity evaluation of functional motility spanning an entire esophageal length [20].
Both Beckingham et al. and Montenovo et al. performed prospective cohort trials in which no statistically significant difference in the prevalence of manometric dysmotility (p = 0.9 [7], p = 0.75 [11]) among patients who developed postoperative dysphagia at up to 1-year follow-up was demonstrated [7, 11]. The lack of correlation between preoperative motility and clinical outcomes was further supported by Booth et al. in a study of 117 patients with normal and ineffective preoperative esophageal motility who underwent laparoscopic Nissen fundoplication for GERD. At 1-year follow-up, 95% of the normal motility cohort and 91% of the ineffective motility cohort reported good/excellent outcome [14]. Scheffer et al. studied HRM in 12 patients among whom significantly elevated intrabolus pressures, a measure of intraesophageal pressure generated by bolus flow, did not correlate with post-fundoplication dysphagia scores [15].
Manometry has been further evaluated in both the intraoperative and postoperative setting to assess surgical outcomes. In a study of 40 patients who underwent intraoperative esophageal manometry, significantly elevated LES pressures after induction of anesthesia were noted among dysphagic patients (47.3 vs. 23.4 cm H20; p = 0.001) [16]. Furthermore, post-fundoplication manometric findings of dual high pressure zones, two regions of high pressure near the LES separated by a lower pressure trough, are predictive of recurrent or persistent reflux symptoms [5, 17]. Yamamoto et al. reported significantly longer length of distal esophagus high pressure zones (p = 0.02) and elevated integrated relaxation pressure (IRP) (p = 0.049), both indicating evidence of outflow obstruction, among post-fundoplication patients with dysphagia [18]. However, Yang et al. demonstrated no association between manometric findings at 3 months and 5 years post-Nissen including LES relaxation pressures and clinical parameters of dysphagia, heartburn, bloat symptoms, or satisfaction [19]. Ultimately, a predominant body of existing evidence regarding the routine use of manometry in the pre- and postoperative settings demonstrate lack of any clinically significant differences in predicting surgical outcome. However, most of these published studies use results from standard manometry, and studies using HRM are contradictory amidst limited distinction of basal vs. residual LES IRP. Today’s high resolution manometry may give some insight into patients who might develop persistent, problematic dysphagia in the long term.
Methods
All patients over the age of 18 years undergoing anti-reflux surgery between July 1, 2011 and December 31, 2014 for symptomatic, refractory GERD were eligible for inclusion. Exclusion criteria included a history of the presence of manometrically proven severe esophageal motility disorder such as achalasia, scleroderma, or aperistalsis, intraoperative finding of esophageal cancer, paraesophageal hernia noted intraoperatively requiring repair, partial posterior, or anterior fundoplication, and lack of preoperative HRM. Of the 146 patients who underwent fundoplication, 52 patients met inclusion criteria.
Among the excluded patients were 48 patients without preoperative HRM either due to workup at an outside facility with conventional manometry or aborted HRM due to poor patient tolerance of the procedure, 28 patients with paraesophageal hernia, 16 patients with a pre-existing esophageal motility disorder, 12 patients who received partial posterior fundoplication, 2 patients who received partial anterior fundoplication, and 1 patient with a history of esophageal cancer.
GERD was diagnosed with a clinical history of typical and/or atypical symptoms of reflux concordant with either evidence of esophageal mucosal injury on EGD or pathologic acid reflux on 24-h ambulatory intraesophageal pH monitoring. Preoperative HRM and assessment of the progression of GERD symptoms was performed with the GERD Health Related Quality of Life (HRQL) questionnaire.
All patients underwent laparoscopic Nissen fundoplication and no conversion to open operation was required. Baseline characteristics of the patient population were notable for a mean patient age of 50.7 ± 11.4 years, 73% female predominance, and 58% rate of preoperative dysphagia of varying severity.
High resolution manometry
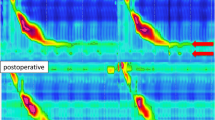
All 52 patients who met inclusion criteria received preoperative HRM prior to fundoplication. HRM was performed by the trans-nasal passage of closely spaced, longitudinal and radially positioned 36 solid-state, circumferential sensors at 1-cm intervals with minimized spatial gaps compared to the 3- to 5-cm spaced sensors of conventional manometry [20]. Ten wet thin liquid swallows of 5 cc each in the supine position were utilized to determine the extent of propagation and amplitude of peristalsis. EGJ pressure morphology was assessed according to the Pandolfino et al. classification and Chicago Classification algorithm, most recently updated v3.0 [20, 21]. A Clouse plot of esophageal pressure topography with HRM was developed as a pressure continuum allowing for enhanced sensitivity of identifying impaired bolus transit secondary to focal breaks in peristalsis or impaired LES relaxation [22].
The parameters assessed by HRM included length from nares to proximal LES, LES length, intraabdominal LES length, basal, and residual LES integrated relaxation pressures (IRP), mean distal contractile integral (DCI), mean wave amplitude, mean wave duration, double-peaked waves, triple-peaked waves, contractile front velocity (CFV), upper esophageal sphincter (UES) mean basal and residual pressure, percentage intact peristalsis, simultaneous peristalsis, hypotensive peristalsis, and failed peristalsis.
Basal LES IRP represents the mean of 4 s of maximal deglutitive EGJ relaxation, whether contiguous or non-contiguous within 10 s of swallowing beginning with UES relaxation [21, 22]. For each patient, mean IRP was calculated for ten swallows and considered normal if 13–43 mmHg. DCI represents the vigor of distal esophageal contraction by incorporating the amplitude, duration, and length of contraction [20,21,22]. Ineffective esophageal motility (IEM) is defined by ≥ 50% ineffective swallows, either failed (DCI < 100 mmHg s cm) or weak (DCI > 100 and < 450 mmHg s cm) peristalsis [20, 21].
Operative technique
A single surgeon performed all operations without conversion. The fundus of the stomach was mobilized by incising the gastrosplenic ligament up to the left crus of the diaphragm in each case. Mediastinal dissection of the esophagus was undertaken for transhiatal mobilization to allow for adequate length of intraabdominal esophagus. The diaphragm crura were reapproximated with 0-non-absorbable suture, and laparoscopic Nissen fundoplication was then performed by creating a 360° wrap over a 54–56 Fr esophageal bougie dilator with 3 interrupted stitches of non-absorbable suture. The wrap was assessed prior to closure for undue tension, twisting, or angulation of the esophagus.
Clinical follow-up
Standardized clinical follow-up of GERD and dysphagia symptoms were completed at set time intervals of the immediate postoperative period within 4 weeks of the date of surgery in clinic, 3 months in clinic, and 34 ± 10.4 months of median telephone follow-up. The already validated GERD Health Related Quality of Life (HRQL) questionnaire was utilized to assess patients at each time point postoperatively with a scale of 0 (no symptoms) to 50 (symptoms incapacitating, unable to perform daily activities). Presence or absence of the following symptoms was sought: heartburn in supine and upright positions, postprandial heartburn, change in diet due to symptoms, nocturnal symptoms of heartburn, dysphagia, odynophagia, bloating, and impact of acid-reducing medication use on daily life.
Dysphagia was defined as difficulty with swallowing or unpleasant sensation of food sticking in the esophagus after swallowing. Patient report of dysphagia was scored on a scale of 0 to 5 (0 = no dysphagia; 1 = dysphagia noticeable, but not bothersome; 2 = symptoms noticeable and bothersome, but not everyday; 3 = symptoms bothersome everyday; 4 = symptoms affect daily activities; 5 = symptoms incapacitating, unable to do daily activities).
One patient was lost to all clinical follow-up postoperatively and one patient died due to unrelated causes prior to any surgical follow-up 2.5 months postoperatively in the setting of palliative care for pancreatic cancer found on CT imaging for refractory, chronic C difficile infection.
Statistical analysis
Statistical analysis was completed using GraphPad Prism Version 6.07 (GraphPad Software, La Jolla California USA). Statistics are expressed as mean ± SD, unless otherwise specified. A level of p < 0.05 was defined as indicating statistical significance. Pearson’s correlation test was used to determine correlation relationships between variables and Mann–Whitney U test was used to compare differences between independent groups after controlling for the remainder variables with multivariate analysis.
Ethics
The institutional review board at the University of Vermont Medical Center and the University of Vermont Committees on Human Research approved this study.
Results
Among the 52 patients who met inclusion criteria, the severity of postoperative dysphagia declined from the immediate postoperative period to the long-term follow-up time point. By long-term follow-up at 34 ± 10.4 months, of the n = 23 (47%) patients who endorsed preoperative dysphagia (measured by a dysphagia score of 2 or higher), n = 14 (61%) endorsed entirely resolved dysphagia symptoms, n = 5 (22%) experienced improved dysphagia, n = 2 (9%) endorsed worse dysphagia, and n = 2 (9%) endorsed stable dysphagia. Of note, n = 3 (6%) of patients experienced new dysphagia postoperatively and n = 25 (48%) had no preoperative or postoperative dysphagia. Of the 52 patients, one patient denied any long-term postoperative dysphagia in the setting of uncertain preoperative dysphagia symptoms (Table 1).
Notable findings on correlation analysis as delineated in Table 2 include a significant, positive correlation between the presence of preoperative dysphagia (score of 2 or higher) and worsened severity of post-fundoplication dysphagia at 3 months (r = 0.40, p = 0.018) and 34 ± 10.4 months (r = 0.42, p = 0.005) follow-up. Elevated basal LES IRP indicating impaired LES relaxation with swallowing was also significantly associated with more severe dysphagia at long-term follow-up (r = 0.57, p < 0.0001) when controlled for preoperative dysphagia, age, gender, esophagitis (r = 0.65, p < 0.0001). On multivariate analysis, basal LES IRP was significantly elevated among patients with postoperative dysphagia at 34 months to 29.9 mmHg (22.4–37.4) vs. 18.1 mmHg (14.8–21.4) among those without dysphagia, p = 0.0013. The sensitivity of elevated preoperative basal IRP (threshold of 15 mmHg) in predicting long-term postoperative dysphagia among the study population was 100% (95% CI 69.2–100%) given a negative predictive value (NPV) of 100% whereas specificity was 41.7% (95% CI 25.5–59.2%) and positive predictive value (PPV) was 32.3% (95% CI 26.5–38.6%).
Additionally, both elevated mean wave amplitude (p = 0.006) and DCI (p = 0.047) were significantly, inversely correlated to post-Nissen dysphagia at long-term months of follow-up. DCI 1000 mmHg cm s (698–1303) among patients with 34-month dysphagia vs. 2361 mmHg cm s (1631–3091) among patients without dysphagia, p = 0.006. Mean wave amplitude 64.9 mmHg (55.3–74.5) among patients with 34-month dysphagia vs. 110 mmHg (91.9–128) among patients without dysphagia, p = 0.0014. UES mean basal pressure was significantly, positively correlated with worsened dysphagia at 34 ± 10.4 months of follow-up (p = 0.037). No significant association was noted between the remaining high resolution manometric parameters of LES length, CFV, or % failed peristalsis in predicting postoperative dysphagia outcomes (Graph 1).
Relationship between basal LES IRP and dysphagia at 34 ± 10.4 months of follow-up, r = 0.57, p < 0.0001. Basal LES IRP 18.1 mmHg (14.8–21.4) w/the absence of 34-month dysphagia and 29.9 mmHg (22.4–37.4) w/presence 34-month dysphagia, p = 0.0013.
Relationship between mean wave amplitude and dysphagia at 34 ± 10.4 months of follow-up, r = − 0.40, p = 0.006. MWA 110 mmHg (91.9–128) w/the absence of 34-month dysphagia and 64.9 mmHg (55.3–74.5) w/the presence of 34-month dysphagia, p = 0.0014.
Relationship between DCI and dysphagia at 34 ± 10.4 months of follow-up, r = − 0.29, p = 0.047. DCI 2361 mmHg cm s (1631–3091) w/the absence of 34-month dysphagia and 1000 mmHg cm s (698–1303) w/the presence of 34-month dysphagia, p = 0.006.
Further correlation analysis of HRM parameters in relation to GERD quality of life scores demonstrated a significant association between poor preoperative quality of life scores and worse quality of life scores at immediate postoperative follow-up within 4 weeks (r = 0.35, p = 0.02), when controlled for preoperative dysphagia, age, gender, esophagitis (r = 0.33, p = 0.039). As with dysphagia, elevated basal IRP was significantly associated with worse quality of life outcomes at long-term follow-up (r = 0.35, p = 0.018). UES mean basal pressure was significantly, positively correlated with worse quality of life at 34 ± 10.4 months of follow-up (r = 0.412, p = 0.004).
Discussion
Despite higher fidelity sensors with HRM compared to conventional manometry, manometric evaluation remains a relatively poor predictor of postoperative dysphagia risk stratification among laparoscopic Nissen fundoplication patients. Predicting susceptibility to post-fundoplication dysphagia in relation to pre-existing clinical variation in esophageal function including pressure and bolus movement spatiotemporal relationships is inherently challenging. The findings of this retrospective analysis demonstrate a significant association between elevated basal LES IRP and worsened severity of long-term post-Nissen dysphagia. Furthermore, patients with long-term dysphagia had lower distal contractile integral and mean wave amplitudes than patients without dysphagia. A potential mechanism for this finding may include the exacerbation of pre-existing elevated basal IRP by fundoplication-induced increased resistance at the EGJ. Of note, low or normal basal IRP in the preoperative setting was a reliable predictor of the absence of long-term postoperative dysphagia thus demonstrating the high sensitivity of basal IRP for post-Nissen dysphagia. Therefore, augmentation of a manometrically intact LES may induce postoperative dysphagia secondary to impaired LES relaxation that is most clinically evident at long-term follow-up of up to 3 years postoperatively.
Also, limited vigor of peristaltic contraction with reduced DCI and mean wave amplitude further contributes to such postoperative dysphagia likely due to inability to overcome LES pressure. Nevertheless, the remainder of novel HRM metrics such as CFV and failed peristalsis have no demonstrable influence on surgical outcome. Preoperative manometry is often indicated to rule out contraindications to anti-reflux surgery such as alternate diagnoses of severe motility disorders including achalasia, scleroderma, and aperistalsis. However, such non-GERD etiologies of dysphagia are justifiably identified with a detailed history of symptomatology suggestive of an esophageal motility disorder. Subclinical esophageal dysfunction discovered on preoperative manometry may manifest as prolonged dysphagia postoperatively as an inherent function of the hiatal anatomic alterations created by a fundoplication.
In concordance with our findings, multiple studies have noted the impact of elevated IRP and impaired LES relaxation as a predictor of dysphagia after fundoplication. Marjoux et al. demonstrated that the only manometric parameter significantly associated with postoperative dysphagia was elevated postoperative IRP at 2–3 months following laparoscopic Nissen-Rossetti fundoplication in 21 patients (5.1 mmHg without vs. 10.2 with dysphagia, p < 0.02) [5]. Elevated EGJ resting pressures and IRPs have been demonstrated as expected post-fundoplication manometric changes [19, 23]. IRP and DCI ranges are higher following Nissen (5.1–24.4 mmHg, 357–4947 mmHg s cm, respectively) than after Toupet fundoplication (3.1–15.0 mmHg, 68–2177 mmHg s cm, respectively) [23]. Such impaired LES relaxation and enhanced vigor of esophageal contraction is likely secondary to circular muscle adaptation to overcome elevated EGJ pressures at relaxation. This compensatory elevation of intrabolus pressure to augment compression has been reported as an adaptive response to increased outflow resistance with restricted hiatal diameter [15].
Residual IRP greater than 15 mmHg (upper limit of normal) in the absence of diagnostic criteria for achalasia and clear esophageal body peristalsis is indicative of EGJ outflow obstruction. In contrast to conventional manometry, IRP is a novel metric which distinguishes the contribution of LES pressure and the crural diaphragm on intraluminal EGJ pressure [15, 22]. Special distinction should be made between residual and basal IRP. Basal IRP is the lowest mean LES pressure recorded for 4 s in the first 10 s after swallowing, while residual IRP is the resting LES pressure between swallows.
Similar to the findings of our study, Wilshire et al. reported significantly greater basal IRP values (16.2 vs. 11.1 mmHg, p = 0.05) among symptomatic compared to asymptomatic post-Nissen patients with dysphagia [24]. Elevated postoperative relaxation pressures, preoperative dysphagia, and female gender were independently associated with postoperative dysphagia [24]. Therefore, such post-Nissen dysphagia is often considered a result of the functional abnormality of increased residual pressure and failure of complete LES relaxation in the post-fundoplication hiatus. More recently, in a retrospective review of 43 patients, Yamamoto et al. also demonstrated that higher IRP values on HRM are associated with post-Nissen fundoplication dysphagia (p = 0.049) [18].
Furthermore, parallel with our study, evidence of preoperative dysphagia serves as an independent predictor of postoperative dysphagia. Wilshire et al. demonstrated that post-Nissen patients experiencing dysphagia were twice as likely to have experienced preoperative dysphagia [24]. Similarly, Montenovo et al. reported that 77% of post-fundoplication dysphagia patients had pre-existing dysphagia prior to surgery whereas 23% had new onset dysphagia, p < 0.01 at median follow-up of 18 months [11]. In contrast, in a retrospective study of 276 patients who underwent either total or partial fundoplication, Fumagalli et al. found no correlation between preoperative and postoperative persistent dysphagia (p = 0.067) [9].
While concordant with existing literature, our study is limited by the retrospective design and relatively small sample size of female-predominant patients available for analysis which inevitably limits power. In the setting of a heterogeneous patient population amidst the predominant use of a Nissen fundoplication approach, the underlying anatomic and physiologic cause of post-Nissen dysphagia varies among individual patients limiting the ability to define a single manometric parameter that universally predicts surgical outcome. The lack of consensus of scoring post-fundoplication dysphagia inherently impacts comparability of studies. Despite these limitations, our analyses demonstrate that an individual’s risk of developing postoperative dysphagia is significantly related to preoperatively impaired LES relaxation with swallowing whereas preoperative normal LES relaxation is associated with the absence of post-Nissen dysphagia.
Recorded values of DCI and MWA on preoperative manometry fell in the lower “normal” range for many patients who developed postoperative long-term dysphagia. These values may not be “normal” for patients undergoing Nissen fundoplication, and surgeons should proceed with some caution when offering anti-reflux surgery to these patients with borderline low values of DCI and MWA. This is also reflected in the relatively weaker correlation relationships ascertained between DCI, MWA, and postoperative dysphagia.
A main outcome for anti-reflux surgery is how GERD impacts a patient’s quality of life. We obtained a quality of life score utilizing the validated GERD-HRQL questionnaire. Interestingly, dysphagia was not associated with a worse quality of life for patients in our study. The only preoperative parameter predictive of worse quality of life outcomes was preoperative upper esophageal sphincter basal pressure. It is possible that those patients with preoperative globus sensation or other atypical symptoms might have worse quality outcomes as the underlying cause of the symptoms may persist even after anti-reflux surgery.
Further clinical research is required to define the role of HRM in preoperative evaluation of the fundoplication patient. Among these include in-depth application of HRM metrics such as the presence of small (2–5 cm) and large breaks (> 5 cm length) in peristalsis as well as means for enhancing the diagnostic yield of HRM with multichannel intraluminal impedance manometry to evaluate effectiveness of bolus clearance, multiple rapid swallows to determine peristaltic reserve, and solid test meal to fully challenge esophageal function [4, 11, 22, 25].
Selective application of manometry in the setting of a positive history of dysphagia, odynophagia, or abnormal motility on videofluoroscopy preoperatively in 628 patients prior to anti-reflux surgery demonstrated no impact on surgical approach, cost savings of 615,600 USD, and 0.8% persistent postoperative dysphagia rate [26]. The selective use of preoperative manometry has been advocated as reserved for patients with a history of dysphagia, atypical GERD symptoms, and poor response to PPI therapy [7]. While tailoring the anti-reflux procedure to specific anatomic or functional esophageal abnormalities has been refuted by multiple studies,[1, 14, 27] further evaluation of the impact of surgical modifications to limit adverse complications is needed. Among these include minimizing extensive dissection for crural exposure as well as potential intraoperative manometry to titrate IRP to acceptable ranges among patients with impaired LES relaxation at baseline [1, 8]. Further evaluation of the effect of partial vs. total fundoplication with a particular focus among those patients with elevated preoperative basal IRP is indicated especially amidst the highly sensitive metric of IRP.
In summary, our study demonstrates that post-Nissen fundoplication dysphagia is independent of most preoperative manometry findings with the exception of impaired LES relaxation, reduced vigor of peristaltic contraction, and limited mean wave amplitude, all of which were significantly associated with dysphagia on long-term follow-up at approximately 3 years. Esophageal manometric findings of peristaltic or LES dysfunction have relatively limited applicability to select a total vs. partial fundoplication operative approach. Ultimately, fundoplication is rooted in a need to balance the risk of recurrent reflux with adverse sequela of dysphagia both of which have significant quality of life implications.
References
Stefanidis D, Hope WW, Kohn GP, Reardon PR, Richardson WS, Fanelli RD (2010) Guidelines for surgical treatment of gastroesophageal reflux. Surg Endosc 24:2647–2669
Booth MI, Stratford J, Jones L, Dehn TCB (2008) Randomized clinical trial of laparoscopic total (Nissen) versus posterior partial (Toupet) fundoplication for gastro-oesophageal reflux disease based on preoperative oesophageal manometry. Br J Surg 95:57–63
Broeders JAJL, Mauritz FA, Ali UA, Draaisma WA, Ruurda JP, Gooszen HG, Smout AJPM, Broeders IAMJ, Hazebroek EJ (2010) Systematic review and meta-analysis of laparoscopic Nissen (posterior total) versus Toupet (posterior partial) fundoplication for gastro-oesophageal reflux disease. Br J Surg 97:1318–1330
Koch OO, Kaindlstorfer A, Antoniou SA, Spaun G, Pointner R, Swanstrom LL (2013) Subjective and objective data on esophageal manometry and impedance pH monitoring 1 year after endoscopic full-thickness plication for the treatment of GERD by using multiple plication implants. Gastrointest Endosc 77:7–14
Marjoux S, Roman S, Juget-Pietu F, Robert M, Poncet G, Boulez J, Mion F (2012) Impaired postoperative EGJ relaxation as a determinant of post-laparoscopic fundoplication dysphagia: a study with high-resolution manometry before and after surgery. Surg Endosc 26:3642–3649
Dıaz de Liano A, Oteiza F, Ciga MA, Aizcorbe M, Trujillo R, Cobo F (2003) Nonobstructive dysphagia and recovery of motor disorder after antireflux surgery. Am J Surg 185:103–107
Beckingham IJ, Cariem AK, Bornman PC, Callanan MD, Louw JA (1998) Oesophageal dysmotility is not associated with poor outcome after laparoscopic Nissen fundoplication. Br J Surg 85:1290–1293
Del Genio G, Rossetti G, Brusciano L, Limongelli P, Pizza F, Tolone S, Fei L, Maffettone V, Napolitano V, del Genio A (2007) Laparoscopic Nissen-Rossetti fundoplication with routine use of intraoperative endoscopy and manometry: technical aspects of a standardized technique. World J Surg 31:1099–1106
Fumagalli U, Bona S, Battafarano F, Zago M, Barbera R, Rosati R (2008) Persistent dysphagia after laparoscopic fundoplication for gastro-esophageal reflux disease. Dis Esophagus 21:257–261
DeMeester TR, Bonavina L, Albertucci M (1986) Nissen fundoplication for gastroesophageal refux disease. Evaluation of primary repair in 100 consecutive patients. Ann Surg 204:9–20
Montenovo M, Tatum RP, Figueredo E, Martin AV, Vu H, Quiroga E et al (2009) Does combined multichannel intraluminal esophageal impedance and manometry predict postoperative dysphagia after laparoscopic Nissen fundoplication? Dis Esophagus 22:656–663
Watson DI, Jamieson GG, Pike GK, Davies N, Richardson M, Devitt PG (1999) Prospective randomized double-blind trial between laparoscopic Nissen fundoplication and anterior partial fundoplication. Br J Surg 86:123–130
Baigrie RJ, Cullis SNR, Ndhluni AJ, Cariem A (2005) Randomized double-blind trial of laparoscopic Nissen fundoplication versus anterior partial fundoplication. Br J Surg 92:819–823
Booth M, Stratford J, Dehn TCB (2002) Preoperative esophageal body motility does not influence the outcome of laparoscopic Nissen fundoplication for gastroesophageal reflux disease. Dis Esophagus 15:57–60
Scheffer RC, Samsom M, Haverkamp A, Oors J, Hebbard GS, Gooszen HG (2005) Impaired bolus transit across the esophagogastric junction in postfundoplication dysphagia. Am J Gastroenterol 100:1677–1684
Khan M, Smythe A, Elghellal K, Ackroyd R (2010) Can intraoperative manometry during laparoscopic fundoplication predict postoperative dysphagia? Surg Endosc 24:2268–2272
Tatum RP, Soares RV, Figueredo E, Oelschlager BK, Pellegrini CA (2010) High resolution manometry in evaluation of factors responsible for fundoplication failure. J Am Coll Surg 210:611–619
Yamamoto SR, Akimoto S, Hoshino M, Mittal SK (2015) High-resolution manometry findings in symptomatic post-Nissen fundoplication patients with normal endoscopic configuration. Dis of Esophagus. doi:10.1111/dote.12392
Yang H, Watson DI, Kelly J, Lally CJ, Myers JC, Jamieson GG (2007) Esophageal manometry and clinical outcome after laparoscopic Nissen fundoplication. J Gastrointest Surg 11:1126–1133
Pandolfino JE, Ghosh SK, Rice J, Clarke JO, Kwiatek MA, Kahrilas PJ (2008) Classifying esophageal motility by pressure topography characteristics: a study of 400 patients and 75 controls. Am J Gastroenterol 103:27–37
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJPM, Pandolfino JE (2015) The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 27:160–174
Clarke JO, Gyawali CP, Tatum RP. High resolution manometry. Ann N Y Acad Sci 2011;349–357
Weijenborg PW, Savarino E, Kessing BF, Roman S, Costantini M, Oors JM, Smout AJPM, Bredenoord AJ (2015) Normal values of esophageal motility after antireflux surgery; a study using high-resolution manometry. Neurogastroenterol Motil 27:929–935
Wilshire CL, Niebisch S, Watson TJ, Litle VR, Peyre CG, Jones CE, Peters JH (2012) Dysphagia postofundoplication: more commonly hiatal outflow resistance than poor esophageal body motility. Surgery 152:584–594
Wang YT, Tai LF, Yazaki E, Jafari J, Sweis R, Tucker E, Knowles K, Wright J, Ahmad S, Kasi M, Hamlett K, Fox MR, Sifrim D (2015) Investigation of dysphagia after antireflux surgery by high-resolution manometry: impact of multiple water swallows and a solid test meal on diagnosis, management and clinical outcome. Clin Gastroenterol Hepat 13:1575–1583
Frantzides CT, Carlson MA, Madan AK, Stewart ET, Smith C (2003) Selective use of esophageal manometry and 24 h pH monitoring before laparoscopic fundoplication. J Am Coll of Surg 197:358–364
Rydberg L, Ruth M, Abrahamsson H, Lundell L (1999) Tailoring antireflux surgery: a randomized clinical trial. World J Surg 6:612–618
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Sonam Kapadia, MD, Edward Borrazzo, MD, Turner Osler, MD, Allen Lee, MD have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Kapadia, S., Osler, T., Lee, A. et al. The role of preoperative high resolution manometry in predicting dysphagia after laparoscopic Nissen fundoplication. Surg Endosc 32, 2365–2372 (2018). https://doi.org/10.1007/s00464-017-5932-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5932-z




