Abstract
Background
Laparoscopic complete mesocoloic excision (CME) with central vascular ligation for splenic flexure cancer is technically challenging because of its anatomical complexity. Although embryological and anatomical consideration should be helpful to perform CME in colorectal cancer surgery, such studies on the splenic flexure are lacking.
Methods
The splenic flexure is located embryologically between the terminal portion of the midgut and the beginning of the hindgut, and is supplied by the superior mesenteric and inferior mesenteric arteries. The mesentery of the transverse and descending colon originally is a continuous sheet, although they rotate and partially fuse to each other during development. Our surgical strategy was excision of the transverse and descending mesocolon with ligation of the left colic artery and left branch of the middle colic artery, and extraction of the specimen in an intact package wrapped by the embryological planes.
Results
We performed laparoscopic surgery according to our surgical strategy in 17 patients with splenic flexure colon cancer. There were no conversions to open surgery or serious intraoperative complications. Two patients had pathological stage (pStage) I, 5 pStage II, 9 pStage III, and 1 pStage IV disease. No patient had recurrence except for 1 with pStage IV cancer, with a median follow-up of 16 months.
Conclusions
Our laparoscopic CME technique is feasible for treatment of splenic flexure cancer. Knowledge of anatomy based on embryology is essential to perform this surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Complete mesocoloic excision (CME) with central vascular ligation (CVL) is recommended as an optimal surgical treatment for colon cancer patients because it has been proven to contribute to superior oncological outcomes [1,2,3]. To achieve successful CME with CVL, precise knowledge of the entire regional mesentery to dissect and the supplying vessels to divide is essential. However, the anatomy around the splenic flexure is complicated and difficult to understand well due to embryological adhesion during development. Furthermore, the arterial blood supply and lymphatic drainage at this site vary and the anatomy of the central vessels is uncertain [4,5,6]. Due to these anatomical peculiarities, the optimal surgery for splenic flexure cancer is not standardized either in open or laparoscopic approach. Although several types of procedures have been advocated so far including extended right hemicolectomy, transverse colectomy, and left hemicolectomy [4, 7,8,9], the optimal extent of resection remains controversial. Operative technique including splenic flexure mobilization is also considered complicated and difficult.
Embryological and anatomical consideration is helpful and useful when performing CME in colorectal cancer surgery. Although several anatomical studies based on embryology regarding the right colon are available, such studies on the splenic flexure are rare [10,11,12]. In this study, we illustrated the anatomical and embryological peculiarities of the splenic flexure with diagrams. We also described our technique of laparoscopic CME with CVL for splenic flexure cancer based on embryology and anatomy.
Materials and methods
Patients
We retrospectively analyzed prospectively collected data of patients who underwent laparoscopic colectomy for colon cancer at our institutions between January 2013 and December 2016. A total of 17 patients with splenic flexure colon cancer were enrolled in this study. In all cases, a single surgeon (TM) who was qualified by the endoscopic surgical skill qualification system of the Japan Society for Endoscopic Surgery (JSES) performed the surgery. Inclusion criteria for this study were (1) histologically proven adenocarcinoma, (2) cT2-4 and cN0-2, and (3) elective surgery. The patients with more than one carcinoma in the colon or with concomitant surgery for other organ carcinoma were excluded. Splenic flexure cancer was defined as a tumor located in the distal third of the transverse colon, or in the left colonic angle, or in the proximal descending colon within 10 cm from the flexure [13]. The clinical stage was diagnosed using colonoscopy, barium enema, and contrast-enhanced computed tomography (CT) of the chest and abdomen. Informed consent was obtained from all patients prior to surgery. This study was approved by the ethics committee of the institutional review board.
Embryological background
The primitive gut mainly consists of three sections: the foregut, midgut, and hindgut (Fig. 1A). The midgut elongates rapidly during week 6 of development, resulting in the formation of the primary intestinal loop [14, 15]. The midgut gives rise to the duodenum distal to the entrance of the bile duct and terminates at the junction between the proximal two-thirds and distal one-third of the transverse colon. The hindgut begins immediately distal to its junction. The superior mesenteric artery (SMA) supplies the midgut, while the inferior mesenteric artery (IMA) supplies the hindgut. Therefore, the splenic flexure located between the terminal portion of the midgut and the beginning of the hindgut is supplied by the SMA and IMA (Fig. 1B).
Development of the primitive gastrointestinal tract. A Lateral view of the primitive gastrointestinal tract at 4–5 weeks of embryonic development. B Lateral view of the primary intestinal loop before rotation. PV portal vein, CA celiac artery, SMA superior mesenteric artery, IMA inferior mesenteric artery, SMV superior mesenteric vein, IMV inferior mesenteric vein
During week 10 of development, the primary intestinal loop rotates 270° counterclockwise around an axis formed by the SMA (Fig. 2A). After rotation, the mesentery of the transverse and descending colon folds and partially fuses to each other, although it originally is a continuous sheet. The anterior sheet of the transverse mesocolon fuses with the posterior wall of the greater omentum while maintaining its mobility. The left edge of its attachment is at the lower pole of the spleen. On the other hand, the posterior sheet of the descending mesocolon fuses with the retroperitoneal wall and the descending colon is fixed to the left abdominal wall in a retroperitoneal position (Fig. 2B). In this way, the splenic flexure of the colon is formed.
Anterior views of the primary intestinal loop after 270° counterclockwise rotation (A) and in the newborn (B). The greater omentum was removed in both figures. The blue and red areas indicate the transverse and descending mesocolons, respectively. SMA superior mesenteric artery, IMA inferior mesenteric artery, MCA middle colic artery; LCA left colic artery, SMV superior mesenteric vein, IMV inferior mesenteric vein (Color figure online)
Surgical strategy
As described above, the splenic flexure cancer can be supplied by the SMA and IMA, suggesting that the dissection of the lymphatic vessels that run into the root of the SMA and IMA would be necessary to achieve radical lymph node (LN) dissection. Therefore, the left colic artery (LCA) from the IMA and the left branch of the middle colic artery (MCA) from the SMA must be divided for CVL. For CME, the transverse and descending mesocolon must be dissected with an intact fascial package. The mesentery of the transverse and descending colon originally is a continuous sheet, although it is rotated and partially fused together during development. Resection of this mesentery with the primary tumor without damage to the embryological planes is required.
Operative procedure
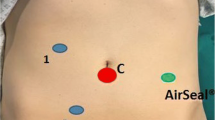
The patient is placed in the Trendelenburg position and the surgery is begun using five ports (Fig. 3).
First, the mesorectum is raised by the first assistant and the retroperitoneal plane is created from the sacral promontory by a medial-to-lateral approach. After identification of the left ureter and gonadal vessels on the dorsal side, the IMA and LCA are exposed. The LCA is isolated and divided at its origin. The inferior mesenteric vein (IMV) is isolated and divided just lateral to the stump of the LCA (Fig. 4A). A medial-to-lateral dissection of the mesentery of the sigmoid colon from the retroperitoneum is performed to the lateral peritoneal reflection. Thereafter, the lateral attachment of the sigmoid colon to the abdominal wall is divided, and the sigmoid colon is completely mobilized.
Intraoperative photos. A The IMA was skeletonized to dissect lymph nodes around its root. The LCA and IMV were divided at origin. B The mesenteric side of the divided vessels was raised by the first assistant, and the descending mesocolon was separated from the retroperitoneal planes. C A gauze was inserted in the dissected space between the descending mesocolon and the retroperitoneal planes. D The transverse mesocolon was divided at the inferior border of the pancreas using the inserted gauze as a landmark. A–D are intraoperative photos in different patients. IMA inferior mesenteric artery, LCA left colic artery, IMV inferior mesenteric vein
Next, the patient’s position is changed to the head-up tilt position to move the small intestine to the caudal side. The mesenteric side of the divided vessels is raised by the first assistant, and the descending mesocolon is separated from the retroperitoneal planes, including Gerota’s fascia, in a medial-to-lateral or caudal-to-cranial manner using the IMV as a landmark (Fig. 4B). This separation is performed laterally to the descending colon attaching to the left abdominal wall. Separation also is performed cranially until the back surface of the pancreas is sufficiently exposed (Fig. 5A). Then, a gauze is inserted in the dissected space (Fig. 4C).
Operative procedures for laparoscopic CME. A After division of the LCA and IMV, the descending mesocolon was separated from the retroperitoneal tissues using a medial-to-lateral approach. B After opening the omental bursa, the transverse mesocolon was divided at the inferior border of the pancreas. The splenic flexure was completely mobilized. C The left branches of the MCA and IMV were divided. The specimen was excised in a package
Finally, the omental bursa is opened wide by dissecting the greater omentum at the gastro-colic ligament with preservation of the gastroepipoloic arcade. An additional port is inserted at the epigastric region if necessary. The transverse mesocolon is divided at the inferior border of the pancreas using the inserted gauze as a landmark (Fig. 4D). The transverse mesocolon is divided to the inferior pole of the spleen. The lateral attachment of the descending colon is divided from the left abdominal wall, and mobilization of the splenic flexure is completed (Fig. 5B). The IMV is divided again at the inferior border of the pancreas. The left branch of the MCA also is divided. The accessory MCA, if any, is divided at the inferior border of the pancreas. It is ready for the specimen to be excised in a package by transection of the colon (Fig. 5C).
The transverse and descending colon, including the splenic flexure tumor, is pulled out through a small incision at the umbilicus and transected using linear staplers. Anastomosis is performed extracorporeally using a functional end-to-end anastomosis technique.
Follow-up
Follow-up was performed every 3 months in the first 2 years and every 6 months thereafter. Tumor markers including CEA and CA19-9 were examined on each follow-up, and CT (chest to abdomen) was performed every 6 months. Total colonoscopy was performed every 2 years.
Results
Patient and tumor characteristics and surgical outcomes are summarized in Table 1. Only 2 patients had a tumor located in the left colonic angle. The median operative time and intraoperative blood loss were 237 min and 20 g, respectively. The median number of harvested LNs was 17. There were no conversions to open surgery or serious intraoperative complications. There were 9 patients with positive LN metastasis. One patient with distal transverse colon cancer had LN metastasis along the left branch of the MCA, while the other 8 had LN metastasis only in the pericolic regions. No patient had recurrence except for 1 with pStage IV disease, with a median follow-up of 16 months.
Discussion
Laparoscopic surgery for splenic flexure cancer performed with CME and CVL is considered difficult because of its anatomical complexity. Its low frequency also is another problem precluding its standardization. Although embryological consideration sometimes is useful for better understanding of surgical anatomy [10,11,12], few studies have focused on the anatomy and embryology of the splenic flexure. In this study, we illustrated the anatomy of the splenic flexure from the embryological point of view. Our laparoscopic technique of CME and CVL based on embryology also was described.
The optimal extent of LN dissection or mesocoloic excision depends mainly on the supplying vessels of the tumor. In cases of right-sided colon cancer, the supplying vessels always originate from the SMA and it is well known that LN dissection along the surgical trunk would be sufficient [16]. In cases of sigmoid colon or upper rectal cancer, mesocoloic or mesorectal excision with high ligation of the IMA should be optimal as radical surgery for advanced disease [17, 18]. However, as described above, the arterial supply of splenic flexure cancers can be from the SMA and IMA, and the optimal extent of lymphatic dissection remains uncertain. Nakagoe et al. [4] reported that LN metastasis in patients with splenic flexure cancer developed along the LCA and the left branch of the MCA, suggesting that dissection of lymphatic vessels with ligation of the LCA and the left branch of the MCA might be necessary for treatment of advanced cancer.
To perform such surgery in accordance with CME, keeping the embryological fascial planes intact during dissection is important. However, the anatomy of the splenic flexure, including its corresponding mesentery and surrounding organs, is very complicated due to torsion and fusion of the primitive gut during development. Surgical techniques that overcome this anatomical complexity must be established. Our technique enables laparoscopic CME with CVL of the LCA and the left branch of the MCA while keeping the embryological planes intact.
Recently, preoperative analysis of vascular anatomy using three-dimensional computed tomography (3D-CT) is making remarkable progress. Although several precise studies on vascular anatomy using 3D-CT for colorectal cancer surgery have been published [19,20,21], most focused on the right colon or rectum, and such data on the splenic flexure are limited. Among our 17 patients, 6 underwent preoperative 3D-CT to evaluate the blood supply to the splenic flexure. Three of the 6 patients had an accessory MCA, which had been reported as a left accessory aberrant colic artery by Rusu [22], as the supplying artery from the SMA to the splenic flexure instead of the left branch of the MCA. On the other hand, the LCA distributed flow to the splenic flexure in all 6 patients. In a previous study on lymphatic flow patterns using indocyanine green fluorescence by Watanabe et al. [23], lymphatic flow of the splenic flexure was observed either in the LCA or the left branch of the MCA. None of their 31 patients exhibited lymphatic flow in both areas. On the other hand, all of our patients underwent lymphatic dissection of both areas. More precise preoperative evaluation of the vascular anatomy and the distribution of lymphatic flows may enable simplification of the operative procedure or shortening of the operative time.
One of the important concerns when performing this surgery is division of the IMV. In this surgery, the IMV must be divided twice. The IMV is divided first at the same level as division of the LCA. After mobilization of the splenic flexure, the IMV must be divided again. Although the IMV generally drains to the splenic vein (SV), it sometimes enters the SMV or the confluence between the SV and SMV [24]. In our technique, the IMV was divided again at the inferior border of the pancreas regardless of the drainage patterns of the IMV. Importantly, as shown in our figures, a main drainage vein of the primitive gut originally was the IMV but not the SMV. There were three main vessels (the LCA, the left branch of the MCA, and the IMV) in the mesentery to be dissected. Therefore, to perform CME for splenic flexure cancer, the IMV must be removed together with the LCA and the left branch of the MCA in a package. Watanabe et al. [23]. reported that 19 of 31 patients (61.3%) exhibited lymphatic flow to the area of the root of the IMV. In addition to the embryological background of the IMV, their findings also support the importance of dissection of the IMV in this surgery.
In conclusion, we described the anatomical peculiarities of the splenic flexure from the embryological point of view. Knowledge of anatomy based on embryology is helpful and essential to perform laparoscopic CME with CVL successfully for splenic flexure cancer.
References
Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S (2009) Standardized surgery for colonic cancer: complete mesocoloic excision and central ligation–technical notes and outcome. Colorectal Dis 11:354–364 (discussion 364–365)
West NP, Hohenberger W, Weber K, Perrakis A, Finan PJ, Quirke P (2010) Complete mesocolic excision with central vascular ligation produces an oncologically superior specimen compared with standard surgery for carcinoma of the colon. J Clin Oncol 28:272–278
West NP, Kobayashi H, Takahashi K, Perrakis A, Weber K, Hohenberger W, Sugihara K, Quirke P (2012) Understanding optimal colonic cancer surgery: comparison of Japanese D3 resection and European complete mesocoloic excision with central vascular ligation. J Clin Oncol 30:1763–1769
Nakagoe T, Sawai T, Tsuji T, Jibiki M, Ohbatake M, Nanashima A, Yamaguchi H, Yasutake T, Kurosaki N, Ayabe H, Ishikawa H (2001) Surgical treatment and subsequent outcome of patients with carcinoma of the splenic flexure. Surg Today 31:204–209
Perrakis A, Weber K, Merkel S, Matzel K, Agaimy A, Gebbert C, Hohenberger W (2014) Lymph node metastasis of carcinomas of transverse colon including flexures. Consideration of the extramesocoloic lymph node stations. Int J Colorectal Dis 29:1223–1229
Pisani Ceretti A, Maroni N, Sacchi M, Bona S, Angiolini MR, Bianchi P, Opocher E, Montorsi M (2015) Laparoscopic colonic resection for splenic flexure cancer: our experience. BMC Gastroenterol 15:76
Rouffet F, Hay JM, Vacher B, Fingerhut A, Elhadad A, Flamant Y, Mathon C, Gainant A (1994) Curative resection for left colonic carcinoma: hemicolectomy vs. segmental colectomy. A prospective, controlled, multicenter trial. French Association for surgical research. Dis Colon Rectum 37(7):651–659
Odermatt M, Siddiqi N, Johns R, Miskovic D, Khan O, Khan J, Parvaiz A (2014) The short- and long-term outcomes for patients with splenic flexure tumours treated by left versus extended right colectomy are comparable: a retrospective analysis. Surg Today 44(11):2045–2051
Nakashima M, Akiyoshi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, Konishi T, Noaki R, Yamakawa K, Nagasue Y, Kuroyanagi H, Yamaguchi T (2011) Colon cancer in the splenic flexure: comparison of short-term outcomes of laparoscopic and open colectomy. Surg Laparosc Endosc Percutan Tech 21(6):415–418
Acar HI, Comert A, Avsar A, Celik S, Kuzu MA (2014) Dynamic article: surgical anatomical planes for complete mesocoloic excision and applied vascular anatomy of the right colon. Dis Colon Rectum 57:1169–1175
Matsuda T, Iwasaki T, Sumi Y, Yamashita K, Hasegawa H, Yamamoto M, Matsuda Y, Kanaji S, Oshikiri T, Nakamura T, Suzuki S, Kakeji Y (2017) Laparoscopic complete mesocoloic excision for right-sided colon cancer using a cranial approach: anatomical and embryological consideration. Int J Colorectal Dis 32:139–141
Stelzner S, Hohenberger W, Weber K, West NP, Witzigmann H, Wedel T (2016) Anatomy of the transverse colon revisited with respect to complete mesocoloic excision and possible pathways of aberrant lymphatic tumor spread. Int J Colorectal Dis 31:377–384
Steffen C, Bokey EL, Chapuis PH (1987) Carcinoma of the splenic flexure. Dis Colon Rectum 30(11):872–874
Sadler TW (2012) Langman’s medical embryology, 12th edn. Lippincott, Philadelphia
Standring S (2015) Gray’s anatomy-the anatomical basis of clinical practice, 41st edn. Elsevier, Philadelphia
Kanemitsu Y, Komori K, Kimura K, Kato T (2013) D3 lymph node dissection in right hemicolectomy with a no-touch isolation technique in patients with colon cancer. Dis Colon Rectum 56:815–824
Kapiteijn E, Putter H, van de Velde CJ (2002) Impact of the introduction and training of total mesorectal excision on recurrence and survival in rectal cancer in The Netherlands. Br J Surg 89:1142–1149
Martling AL, Holm T, Rutqvist LE, Moran BJ, Heald RJ, Cedemark B (2000) Effect of a surgical training programme on outcome of rectal cancer in the County of Stockholm. Stockholm Colorectal Cancer Study Group, Basingstoke Bowel Cancer Research Project. Lancet 356:93–96
Fukuoka A, Sasaki T, Tsukikawa S, Miyajima N, Ostubo T (2016) Evaluating distribution of the left branch of the middle colic artery and the left colic artery by CT angiography and colonography to classify blood supply to the splenic flexure. Asian J Endosc Surg 10:148–153
Miyamoto R, Nagai K, Kemmochi A, Inagawa S, Yamamoto M (2016) Three-dimensional reconstruction of the vascular arrangement including the inferior mesenteric artery and left colic artery in laparoscope-assisted colorectal surgery. Surg Endosc 30:4400–4404
Ogino T, Takemasa I, Horitsugi G, Furuyashiki M, Ohta K, Uemura M, Nishimura J, Hata T, Mizushima T, Yamamoto H, Doki Y, Mori M (2014) Preoperative evaluation of venous anatomy in laparoscopic complete mesocoloic excision for right colon cancer. Ann Surg Oncol 21(Suppl 3):S429–435
Rusu MC, Vlad M, Voinea LM, Curca GC, Sisu AM (2008) Detailed anatomy of a left accessory aberrant colic artery. Surg Radiol Anat 30:595–599
Watanabe J, Ota M, Suwa Y, Ishibe A, Masui H, Nagahori K (2017) Evaluation of lymph flow patterns in splenic flexural colon cancers using laparoscopic real-time indocyanine green fluorescence imaging. Int J Colorectal Dis 32:201–207
Al-Asari SF, Lim D, Min BS, Kim NK (2013) The relation between inferior mesenteric vein ligation and collateral vessels to splenic flexure: anatomical landmarks, technical precautions and clinical significance. Yonsei Med J 54:1484–1490
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Takeru Matsuda, Yasuo Sumi, Kimihiro Yamashita, Hiroshi Hasegawa, Masashi Yamamoto, Yoshiko Matsuda, Shingo Kanaji, Taro Oshikiri, Tetsu Nakamura, Satoshi Suzuki, and Yoshihiro Kakeji have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Matsuda, T., Sumi, Y., Yamashita, K. et al. Anatomical and embryological perspectives in laparoscopic complete mesocoloic excision of splenic flexure cancers. Surg Endosc 32, 1202–1208 (2018). https://doi.org/10.1007/s00464-017-5792-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5792-6