Abstract
Purpose
Laparoscopic ventral hernia repair is a well-established technique with satisfying outcomes even at long term for the treatment of incisional and ventral hernia. However, the literature debate is still ongoing regarding the preferred surgical technique. Nowadays, two approaches are commonly adopted: the intraperitoneal onlay mesh repair (sIPOM) and the intraperitoneal onlay mesh reinforcement with defect closure before mesh placement (pIPOM). The aim of this prospective analysis is to compare the postoperative outcomes of patients treated for incisional hernia (IH) with sIPOM and pIPOM after 36 months follow-up in terms of recurrence, quality of life and wound events.
Methods
Patients receiving pIPOM and sIPOM for IH were actively followed up for 36 months. At the outpatient clinic, hernia recurrence (HR), mesh bulging (MB), quality of life with the Gastrointestinal Quality of Life Index (GIQLI) and wound events were assessed.
Results
Between January 2015 and January 2019, 98 patients underwent a pIPOM and 89 underwent an sIPOM. At 36 months, nine patients (4 in pIPOM and 5 in sIPOM) experienced an HR, while MB was recorded in four patients in pIPOM and nine in sIPOM. No statistically significant difference could be identified also in terms of final GIQLI score and wound events.
Conclusions
LVHR with or without fascial closure, also in our study, provides satisfactory results in terms of safety and efficacy. The discordant results in the literature are probably related to independent variables such as the type of mesh, the type of suture and closure technique. Therefore, was the funeral of sIPOM done too early?
Study dataset is available on ClinicalTrials.gov ID
NCT05712213
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The treatment of ventral hernias, either primary or incisional, is often a great challenge for abdominal wall surgeons. Laparoscopic ventral hernia repair (LVHR) is a worldwide well-established technique with satisfying outcomes reported in literature even at long term [1]. However, several considerable controversies regarding the optimal approach and the patient selection have been raised [1,2,3]. Nowadays, two intraperitoneal mesh approaches are commonly used in LVHR: the simple intraperitoneal onlay mesh repair (sIPOM) and the intraperitoneal onlay mesh reinforcement with defect closure before placement of mesh (pIPOM) [2]. The pIPOM has been introduced to reduce the adverse events of incisional hernia (IH) surgery (i.e., seroma formation, recurrences, etc.) possibly associated with laparoscopic hernia repair [3], and satisfactory outcomes have been reported in several studies [3,4,5,6]. In detail, sequelae such as mesh bulging seems to be less associated with pIPOM than sIPOM, even if the latter topic is a matter of intense debate. The pIPOM has been introduced in the guidelines for the laparoscopic treatment of ventral and incisional abdominal wall hernias published by the International Endohernia Society (IEHS) in 2014 [1]. Despite that prospective studies on the quality of IPOM plus are available, the evidence level for the statements in these guidelines remains low [7]. The aim of this prospective analysis is to compare the postoperative outcomes of patients treated for incisional hernia (IH) with sIPOM and pIPOM after 36 months follow-up in terms of recurrence, quality of life and wound events.
Methods
Study design
A prospective, open-labeled, study was conducted to evaluate the effectiveness of pIPOM and sIPOM in patients with IH. This study was reviewed and approved by the local regional ethics committee. It was conducted according to the ethical principles stated in the Declaration of Helsinki. Study dataset is available on clinicaltrial.gov (NCT05712213). We adhered to the CONSORT guidelines in reporting the trial’s results.
Study setting and population
The study was conducted from January 2018 to June 2019 in three departments of general surgery (the “A. Rizzoli” Hospital of Lacco Ameno in the Asl Napoli 2 Nord District, the University of Campania “Luigi Vanvitelli” of Naples and the AORN “A. Cardarelli” of Naples). Inclusion criteria were as follows: IH with length > 3 and < 12 cm (cm) width or length (medium size according to European Hernia Society classification of incisional hernias [8]), a body mass index (BMI) < 35 kg/m2, an age between 18 and 65 years, an elective surgery setting and a clean wound field according to the Centre for Disease Control and Prevention (CDC) wound classification (Grade I) [9]. Exclusion criteria were represented by IH < 3 or > 12 cm, abdominal aortic aneurysm (AAA) disorders, pregnancy or lactation, psychiatric illness, multifocal hernia defect, life expectancy < 2 years, inflammatory bowel disease, emergency setting and not clean wound fields. Written informed consent was obtained from all subjects. All procedures were performed by surgeons with at least 15 years’ experience in general surgery, and with experience of over 100 laparoscopic procedures of hernia repair using meshes.
The centers were chosen based on their history of activity over the last 5 years in terms of pIPOM vs sIPOM, with the expectation of obtaining two homogeneous groups in terms of the number of patients.
Preoperative evaluation
Preoperative evaluation included anthropometric measurements (gender, height in cm, weight in kg, BMI in kg/m2), comorbidity evaluation (HbA1c, chronic obstructive pulmonary disease (COPD), hypertension, chronic use of corticosteroid, smoking). All patients underwent a clinical visit and a computed tomography (CT) scan to assess the size and location of the hernia and volume of sac. The presumed volume of the hernial sac was also estimated in all patients through longitudinal and sagittal reconstructions and expressed in cm3. The IH of each patient of both groups was classified according to the European Hernia Society for incisional hernias in small (< 4), medium (> 4 < 10) and large > 10 [10]. Preoperatively, the quality of life was evaluated via the translated version of the Gastrointestinal Quality of Life Index (GIQLI) (11), a 36-item questionnaire [8].
Gastrointestinal Quality of Life Index (GIQLI) questionnaire
The Gastrointestinal Quality of Life Index (GIQLI) is a validated, 36-item, self-administered questionnaire that addresses five domains: upper gastrointestinal symptoms (12 items), lower gastrointestinal symptoms (7 items), physical status (7 items), psychological status (5 items) and social status (5 items). Each item is quoted from 0 to 4; scores range from 0 to 144, with higher scores indicating better function. Correct or incorrect allocation was then evaluated [8].
Surgery
The first steps of both procedures were identical. The pneumoperitoneum (12–15 mmHg) was built up with Veres in the Palmer’ point. The primary optical trocar was set in the left upper abdomen, and two other trocars were set in the left middle and lower abdomen. If necessary, adhesiolysis was first performed. The posterior fascia, where the mesh was located, was exposed by excising the peritoneal fat to prevent seroma formation and, if possible, all hernia sac was removed to facilitate the healing of the hernia defect after laparoscopic suture. This also included the transection of the ligamentum teres hepatis. We reduced the intra-abdominal pressure to approx. 5 mmHg and measured the hernia gap through an intraperitoneal graduated mark. The choice of mesh size was done with an overlap of more than 5 cm (10). In case of pIPOM, before the mesh positioning, the laparoscopic closure of the hernia defect was performed with permanent sutures of Prolene 1/0 (Medtronic GmbH, Meerbusch, Germany) at a distance of 1.5 cm from stich to stich using a laparoscopic suture passer. In sIPOM, the defect was not closed. In both the groups, the final fixation of the mesh took place with non-resorbable tacks (30–90 ProTacksTM, Ti-CronTM 0 Medtronic) and ring of three concentric rings in the triple-crown technique.
Study intervention
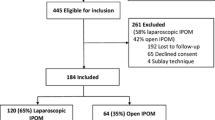
Enrolled subjects were allocated to the pIPOM or sIPOM groups basede on the center’s routine surgical practice. All patients referred to the Rizzoli Hospital underwent pIPOM, while the patients referred to the University of Campania “Luigi Vanvitelli” and the AORN “A. Cardarelli” underwent sIPOM. The enrollment procedure is detailed in Fig. 1. In Group A, laparoscopic IH repair was performed with closure of fascia with non-absorbable suture (pIPOM); in Group B, laparoscopic IH or VH was performed without fascia closure (sIPOM). The mesh used to repair the abdominal wall in both groups was an intraperitoneal Gore-Tex® mesh (GM) (Dual Mesh; W.L. Gore & Associates, Flagstaff, AZ, USA). The choice of the dimensions of the prosthesis was tailored, requiring at least an overlap of 5 cm.
The CONSORT flow diagram. Statistical analysis was performed following an intention to treat protocol. sIPOM (intraperitoneal onlay mesh repair), pIPOM (intraperitoneal onlay mesh reinforcement with defect closure before placement of mesh), IH (incisional hernia), AAA (abdominal aortic aneurysm), GIQLI (Gastrointestinal Quality of Life Index)
Postoperative morbidity (scored according to Clavien–Dindo classification [9]), mortality, length of hospitalization and surgical reinterventions were recorded. All patients were actively followed up regularly at 3, 6, 12, 18, 24 and 36 months. During each follow-up visit, anthropometric measurements were performed. Hernia recurrence (HR) and mesh bulging (MB), in pIPOM and sIPOM, were clinically and radiographically evaluated (via ultrasound) on an outpatient basis. In detail, HR was clinically defined as any visible or palpable ‘‘blowout’’ in the abdominal wall. US evaluation was carried out by a radiologist with 15 years of gastrointestinal US experience. An RS85 (Samsung Madison Co Ltd., Seoul, Korea) ultrasound with a convex transducer (CA1-7A) was employed. The ultrasonic criteria of HR were a visible gap within the abdominal wall and/or ‘‘tissue moving through the abdominal wall by Valsalva maneuver’’ and/or a detectable ‘‘blowout’’. The size and location of all ultrasonographically detected HR were registered, as well as any other patient’s complaint. HR was diagnosed and recorded if clinical criteria and/or ultrasound criteria were fulfilled. [7]. MB was defined as any clinically evident protrusion through the hernial defect causing swelling. It was as well clinically and ultrasonographically evaluated at the outpatient visit. In doubtful cases of MB, computerized tomography (CT) was performed. Physicians were blinded about group (pIPOM and sIPOM) allocation. The study was completed at 3 years’ follow-up in each patient. Regarding the secondary end points, the classification of wound events was assigned according to the likelihood and degree of wound contamination at the time of the operation, as stated in the Centre for Disease Control and Prevention (CDC) wound classification (superficial, deep or organ space) [11]. Surgical site events were reported according to the Ventral Hernia Working Group definitions [9, 12]. The difference between seroma and hematoma was made with ultrasound study. Actions for wound events were categorized as follows: antibiotics only, bedside wound interventions, percutaneous maneuvers or surgical debridement.
During the previously scheduled outpatients’ controls, the GIQLI was administered to the patients at 0 and after surgery at 3, 6, 12, 24 and 36 months [8].
At 36 months, cosmesis was assessed by telephone interview or at outpatient clinic, by an operator blinded about the groups’ allocation, asking whether the patient was satisfied about the cosmetic effect of the procedure (response yes or no).
Study outcomes
The primary outcome was to evaluate the HR and the MB rate at 1, 3, 6, 12, 24 and 36 months postoperatively, in the pIPOM and sIPOM groups. The secondary end points included incidence of wound events within the first 30 postoperative days, the evaluation of quality of life during the follow-up period and the cosmesis at 36 months.
Blinding process
Patients, care providers, staff collecting data and those assessing the end points were all blinded to treatment allocation. Because the blinding of the operating surgeons was not feasible, they were not involved in the data collection and outcome assessment. Physicians in charge of patients’ management were not involved in the operating room and blinded to the intervention. The data were collected and analyzed by physicians who were not involved in the patient’s management during the study.
Statistical analysis and sample size calculation
The sample size was calculated by Sealed Envelope Ltd. 2012. It was estimated that 69 subjects per group would be required assuming no difference between the standard and experimental group (90% in both groups) with an equivalence limit of 15% in the primary outcome (HR and the MB rate at 1, 3, 6, 12, 24 and 36 months postoperatively) between the two groups, a two-tailed α of 0.05 and power of 80%. Data analysis was conducted according to an intention-to-treat approach. Statistical analysis was performed via Excel 2011® (Microsoft, Redmond, WA). Categorical data were reported as raw numbers with percentages in parenthesis or vice versa. Continuous data were reported as medians with range in parenthesis, according to the non-normal distribution. The differences between results were compared using the Fisher’s exact test for prevalence data and the Mann– Whitney U test for continuous data. The association between the recurrence rate (dependent variable) and the patients’ characteristics (independent variables) was assessed by the multiple logistic regression analysis. A probability value of less than 0.05 was considered significant. The collected results were analyzed with the Kaplan–Meier method to estimate the probability over the time of the IH recurrence. In particular, the method estimates the survivor functions for the two groups of enrolled subjects; i.e., those treated with simple intraperitoneal onlay mesh repair (sIPOM) and those with intraperitoneal onlay mesh repair after the fascia defect closure (pIPOM). Noteworthy, the eventual recurrence event was evaluated at specific follow-up times: 3, 6, 12, 24 or 36 months. The patients who after 36 months did not report the presence of IH were considered right censored (i.e., subjects for whom the information on their possible future recurrence exceeded the time limit of this study) [R#2–11]. In such an approach, the underlying distribution of the first outcome variable can be assessed in its dependence on some independent variables, such as age, BMI (classified in proper classes), gender, diabetes mellitus, ASA and COPD. Concerning the classes used to classify the patients, regarding age, it was considered the median of the enrolled subjects, younger or older than 55 years; regarding BMI, standard classes were considered: underweight (< 18.5, 3.2% of subjects in both treatments), normal weight (> = 18.5 and < = 24.9, 9.1% of subjects), overweight (> = 25 and < = 29.9, 62.9%) and obesity (> = 30, 24.8%). A further analysis was then conducted on the GIQLI index; in this case, the mean values were observed for patients before the interventions and after 3 or 36 months follow-up.
Results
Study population
Between January 2015 and January 2019, out of 245 patients assessed for eligibility, 187 (65.1%) met the inclusion criteria and were enrolled in the current study (Fig. 1). Of these, 98 (52.4%) patients underwent a pIPOM and 89 (47.5%) underwent an sIPOM (Fig. 1) and were included in the modified intention-to-treat analyses.
Baseline characteristics of the two groups are summarized in Table 1. Median additional operating time required for laparoscopic defect closure was 18 (11–26) min in the pIPOM group. The median duration of the hospital stay was 2 (1–8) days in both groups (p = 1; Mann–Whitney U test). In eight patients (5 in pIPOM and 3 in sIPOM) intraoperative complications occurred during surgery: one meso-ileal bleeding during adhesiolysis in the sIPOM group and seven ileal or colic lesions requiring intracorporeal suturing without the need for conversion (3 in pIPOM and 4 in sIPOM group). Two patients were laparoscopically re-operated for complications not related to abdominal wall closure within 30 days from the operation (1 in pIPOM group for occlusion; 1 in sIPOM group for bowel leak); these patients were excluded from the study. There was no 30-day mortality in either group. Intraoperative and postoperative complications until and after 30 days are reported in Table 2. Among all the enrolled patients, 19 (10.1%) (11 in pIPOM and 8 in sIPOM) were lost to follow-up and 168 (87 in Group A and 81 in Group B) completed the entire scheduled follow-up evaluation.
Primary outcome
Table 3 shows the recurrence rate at each follow-up point of both groups. No statistically significant differences were found between groups. At 36 months follow-up, a total of nine (4 in pIPOM and 5 in sIPOM, p = 0.624) HR had been reported across both groups. All the recurrences had a diameter of less than 5 cm on ultrasound imaging, with no statistically significant difference between the groups. In details, at 36 months, all the four patients (4.1%) in the pIPOM, who had developed an HR, were diagnosed by clinical examination confirmed by ultrasound examination. In sIPOM five patients (5.7%) developed an HR 36 months after surgery; the hernia was clinically evident in five cases (100%). The multivariate analysis confirmed the role of comorbidity in increasing the risk of HR. In detail, male sex (OR 6.52, 1.6–29.1; p < 0.01), diabetes mellitus (OR 9.4, 1.6–59.5; p < 0.001) and smoking (OR 7.16; 1.198–45.04; p < 0.001) were risk factors for the development of HR.
Table 4 shows the prevalence of mesh bulging at each follow-up point in both groups. At 36 months, of a total of 13 patients who developed an MB [4 (4.1%) patients in pIPOM and 9 (10.1%) in sIPOM], 10 (76.9%) were diagnosed by clinical examination and confirmed by ultrasound examination (4 in pIPOM and 6 in sIPOM). In four patients, all undergoing sIPOM, MB was not clinically evident, but diagnosed by US imaging and confirmed by CT scan. These patients had an abundant subcutaneous tissue at the site of the primary defect below the umbilical line. All patients with MB underwent abdomen CT to confirm the diagnosis.
Figure 2 depicts the estimated survivor functions for both treatments; despite that sIPOM seems to decrease more than the other, the evidence of a possible difference in survival curves at longer times is not confirmed due to the value of the log-rank significance test and its associated p value (test = 0.79, p-value = 0.37).
Table 5 reports the results of the log-rank tests carried out on the independent variables to identify those able to affect the survival time for both groups; considering a p value threshold of 0.05, the following variables were significant: COPD, diabetes mellitus, oncologic disease.
During the study, five patients (3 in pIPOM, 2 in sIPOM) required reoperation within 12 months for different diseases. No differences were found among these patients in terms of peritoneal adhesions. Two patients in each group underwent surgery for recurrent incisional hernia during follow-up.
Secondary outcomes
Morbidity 30 days after surgery is summarized in Table 6. Subclinical wound seroma was reported in seven (7.1%) and eight (8.9%) patients in the pIPOM and sIPOM, respectively (p = 0.642). All seromas were diagnosed by ultrasound imaging. They did not impair wound healing in any patient. In three patients in pIPOM, the seroma was aspirated 10 days after operation, with complete resolution obtained within 20 days in all the cases. Deep infection was not reported in any patient.
Hematoma was reported in eight (8.2%) and two (2.2%) patients in pIPOM and sIPOM respectively (p = 0.072). All hematomas were diagnosed clinically and confirmed by ultrasound imaging. In four patients in pIPOM, the hematoma was aspirated 20 days after operation, with complete resolution obtained within 30 days in all cases.
The GIQLI index showed a great improvement after the surgery in both groups without any statistical difference in the different follow-up periods (Table 7), except for the results at 3 months with 101.84 ± 5.52 in the pIPOM group vs 109.37 ± 4.55 in the sIPOM group (p < 0.05). In the next follow-up times, it appeared to increase, reaching more than 130 points on average at 36 months (131.3 ± 6.1).
Regarding the cosmetic effect, 91 patients out of 98 in pIPOM (92.8%) and 79 out of 89 in sIPOM (88.7%) answered affirmatively regarding the cosmetic result of the intervention (p = 0.330).
Discussion
The results of the present prospective analysis at 3-year follow-up were comforting both in terms of HR and MB with no statistically significant differences between the two groups, although the MB data are higher in the sIPOM group and certainly not negligible. Laparoscopic approach for the treatment of hernias of various districts has become a consolidated surgical option. Several studies in literature have confirmed the safety and efficacy of laparoscopic treatment compared to the traditional one for VH and IH in terms of recurrences [1, 5, 11, 14,15,16]. In detail, some reports associated sIPOM with a higher recurrence rate than pIPOM [14]. However, the literature debate is ongoing.
In the current series on 98 (52.4%) patients undergoing a pIPOM and 89 (47.5%) undergoing an sIPOM, no statistically significant differences were found between groups in terms of hernia recurrence at any follow-up period, with 4 (4.1%) patients in pIPOM and 5 (5.7%) patients in sIPOM (p = 0.624) experiencing this sequela. All the recurrences had a diameter of less than 5 cm on ultrasound imaging, but it is worth commenting that the size of the incisional hernia is a dynamic time-depending event. Therefore, the current limited follow-up of 36 months could affect this data.
The randomized controlled trial by Lambrecht et al. [14] mainly analyzed the surgical outcomes of primary versus secondary ventral (incisional) hernia repair and also compared pIPOM and sIPOM for these two subsets of hernias. The study concluded that the defect closure with absorbable suture was associated with a higher overall complications risk (OR 3.42; CI 1.25–9.33) and no long-term benefits. Conversely, Mitura and Pawlak et al.’s [15] studies reported an incidence of recurrence in patients who underwent pIPOM statistically lower than those who underwent sIPOM. An explanation for these discordant data could be related to the type of implanted material and the technique used to close the sheets and the fixation of the mesh. The above-mentioned implanted material could be an important variable in the analysis of the results. In several studies, in fact, meshes were used with mechanical resistance < 35 N/cm2 and the non-closure of hernia defect seems to significantly stretch the mesh due to the lack of a support in its central portion; this aspect should be taken into consideration in the analysis of the literature results. In this study, a mesh with a mechanical resistance to the implant greater than 42 N/cm2 was used and fixed with non-resorbable tacks. Probably, these two aspects could have played a protective role in patients without fascia defect closure. Moreover, the 5 cm overlap also reduces the chances of mesh “shrinkage” affecting the incidence of recurrence.
The absence of statistically significant differences in the two groups could be also related to the technique used (Laparoscopic Suture Passer Storz Type 2.1 mm) for the closure of the defect. It determines a non-tension-free closure, which has poor effectiveness already at a follow-up of 3 months, as confirmed by the US results. Moreover, in the multivariate analysis it was found that the horizontal and vertical dimension ratio is more important than the area of the defect. Probably, the greater distance between the sheets determines greater tension and therefore the possibility that the points could yield.
Multivariate analysis confirmed the role of comorbidity in increasing the risk of incisional herniation. Especially smokers, who have a worse outcome, and certainly the increase in intra-abdominal pressures in a bridge technique play an important role, as reported by many in the literature [5,6,7]. According to our results, although no statistically significant differences were recorded for MB between the two groups at any period of follow-up (p = 0.105 at 36 months), it cannot be denied that fascia closure appears to have a protective effect, with a lower rate of its incidence (4.1% vs 10.1% at 36 months).
In literature controversial results are reported [14, 16,17,18]. Removing the peritoneal sac, closure of the dead space after closure of the defect and/or decreased mesh contact with the sac seem to reduce the risk of seroma formation [13]. In our study although the incidence of both clinical and US seroma is higher in the sIPOM group than in the pIPOM group (7.1% vs 9.2%, p = 0.609), no seroma was detected after 6 months of follow-up also in the sIPOM group. One patient of pIPOM had an ischemia of skin. Therefore, the sac excision in our experience does not appear to protect against seroma formation and appears important to highlight that when the patient’ abdominal wall is not thick enough, it can cause ischemia of the skin and dehiscence, as elsewhere reported [14].
In three patients (2 group sIPOM, 1 group pIPOM), the seroma was perceived like a recurrence, but after the US diagnosis, it was easily drained without sequelae.
Furthermore, regarding seroma our results showed that the size of the hernial sac in cm3 could play a prominent role rather than the dimensions of the wall defect in length or width. Probably, the greater “empty space” is a condition favoring seroma formation. The incidence of hematoma and infection in our data was lower in the sIPOM group (8.2% vs 2.2% and 3.1% vs 1.1%), but without any statistical significance. The use of the suture passer could have influenced the rate of the hematoma, while the removal of the sac could have been caused the access to subcutaneous fat in pIPOM. However, no patient required any invasive therapy and was conservatively treated. Three patients of the pIPOM group vs one patient of sIPOM presented a superficial wound infection, which did not require surgical therapy and were administered with oral antibiotics. Probably, the extracorporeal closure of the fascia would seem to play a role in this issue.
Regarding the estimated survivor functions for both treatments, despite the sIPOM seems to be more decreasing than the other, the evidence of a possible difference in survival curves at longer times is not confirmed due to the value of the log-rank significance test and of its associated p value (test = 0.79, p value = 0.37). In other words, it is possible to confirm that the differences between treatments depend only on random factors and they do not affect the HR.
At 3 months, there was a statistically significant difference in the quality of life measured with the GIQLI index, more favorable for sIPOM group (109.37 ± 4.55 vs 101.84 ± 5.52, < 0.05). The closure of fascia in a no-tension free fashion seems to increase pain and paresthesia in the first postoperative period. However, at the other follow-up times, no difference was detected. In literature, few studies have investigated this outcome [13] and similarly did not show significant difference in pain scores. Noteworthy, methods and type of recording pain were highly variable between studies, limiting comparison of the results.
Cosmesis was assessed at 36 months follow-up by telephone interview or at outpatient clinic by operator blinded to the groups’ allocation. Our results showed full satisfaction in 91 patients out of 98 in pIPOM (92.8%) and 79 out of 89 in sIPOM (88.7%) (p = 0.330)). However, the similar rate of non-satisfaction percentages in both groups was not negligible. This aspect should be taken into consideration because, perhaps, the expectations of laparoscopic surgery are very high in patients. Moreover, often the patient’s feeling and comfort after the surgical treatment of benign pathologies are more important than the objective result itself. Probably, surgeons should be sure that the patient understands the difference between an abdominal wall repair and its reconstruction, thus allowing a more informed choice and a better understanding of the possible surgery outcome. This aspect must be taken into account, as the patient satisfaction is one of the most important goals of this kind of surgery.
This study has several limitations: even if the design is prospective, it is not randomized; the interventions were not performed by a single surgeon and the surgical technique was chosen according to their routine practice, determining a selection bias that should take into account. The patients with multiple hernia defects or obese patients were excluded to maximize the homogeneity of the two cohorts. Moreover, the number of patients and the follow-up length are limited.
Conclusion
Despite the differences in etiology, laparoscopic ventral hernia repair (LVHR) with or without fascial closure, also in our study, provides satisfactory results in terms of safety and efficacy suggesting that LVHR with synthetic mesh is safe and effective in both surgical techniques, plus and standard. The discordant results in the literature are probably related to independent variables such as the type of mesh used and the type of suture and closure technique used in the pIPOM. Therefore, was the funeral of sIPOM done too early?
Data availability
Study dataset is available on ClinicalTrials.gov ID: NCT05712213.
References
Bittner R, Bain K, Bansal VK, Berrevoet F, Bingener-Casey J, Chen D, Chen J, Chowbey P et al (2019) Update of guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (international endohernia society (IEHS)-part A. Surg Endosc. 33(10):3069–3139. https://doi.org/10.1007/s00464-019-06907-7
Köckerling F, Simon T, Adolf D, Köckerling D, Mayer F, Reinpold W, Weyhe D, Bittner R (2019) Laparoscopic IPOM versus open sublay technique for elective incisional hernia repair: a registry-based, propensity score-matched comparison of 9907 patients. Surg Endosc. 33(10):3361–3369. https://doi.org/10.1007/s00464-018-06629-2
ChelalaE BarakeH, Estievenart J, Dessily M, ChararaF AJL (2016) Long-term outcomes of 1326 laparoscopic incisional and ventral hernia repair with the routine suturing concept: a single institution experience. Hernia 20:101–110. https://doi.org/10.1007/s10029-015-1397-y
Orenstein SB, Dumeer JL, Monteagudo J, Poi MJ, Novitsky YW (2011) Outcomes of laparoscopic ventral hernia repair with routine defect closure using ‘shoelacing’ technique. Surg Endosc 25:1452–1457. https://doi.org/10.1007/s00464-010-1413-3
Tandon A, Pathak S, Lyons NJ, Nunes QM, Daniels IR, Smart NJ (2016) Meta-analysis of closure of the fascial defect during laparoscopic incisional and ventral hernia repair. Br J Surg 103(12):1598–1607. https://doi.org/10.1002/bjs.10268
Hellinger A, Wotzlaw F, Fackeldey V, Pistorius G, Zdichavsky M, Jünemann R, Buia A (2016) Development of an open prospective observational multicentre cohort study to determine the impact of standardization of laparoscopic intraperitoneal onlay mesh repair (IPOM) for incisional hernia on clinical outcome and quality of life (LIPOM-Trial). Contemp Clin Trials Commun. 11(4):118–123. https://doi.org/10.1016/j.conctc.2016.08.001
Suwa K, Okamoto T, Yanaga K (2016) Closure versus non-closure of fascial defects in laparoscopic ventral and incisional hernia repairs: a review of the literature. Surg Today. 7:764–773. https://doi.org/10.1007/s00595-015-1219-y
Pizza F, D’Antonio D, Ronchi A, Lucido FS, Brusciano L, Marvaso A, Dell’Isola C, Gambardella C (2021) Prophylactic sublay non-absorbable mesh positioning following midline laparotomy in a clean-contaminated field: randomized clinical trial (PROMETHEUS). Br J Surg 108(6):638–643. https://doi.org/10.1093/bjs/znab068. (PMID: 33907800)
DeBord J, Novitsky Y, Fitzgibbons R, Miserez M, Montgomery A (2018) SSI, SSO, SSE, SSOPI: the elusive language of complications in hernia surgery. Hernia. https://doi.org/10.1007/s10029-018-1813-1
Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E, Dietz UA, Eker HH, El Nakadi I, Hauters P, Hidalgo Pascual M, Hoeferlin A, Klinge U, Montgomery A, Simmermacher RK, Simons MP, Smietański M, Sommeling C, Tollens T, Vierendeels T, Kingsnorth A (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13(4):407–414. https://doi.org/10.1007/s10029-009-0518-x
O’Hara LM, Thom KA, Preas MA (2018) Update to the centers for disease control and prevention and the healthcare infection control practices advisory committee guideline for the prevention of surgical site infection (2017): a summary, review, and strategies for implementation. Am J Infect Control 46(6):602–609. https://doi.org/10.1016/j.ajic.2018.01.018
Hodgkinson JD, Worley G, Warusavitarne J, Hanna GB, Vaizey CJ, Faiz OD (2021) Evaluation of the ventral hernia working group classification for long-term outcome using english hospital episode statistics: a population study. Hernia 25(4):977–984. https://doi.org/10.1007/s10029-021-02379-8. (Epub 2021 Mar 13)
Suwa K, Okamoto T, Yanaga K (2016) Closure versus non-closure of fascial defects in laparoscopic ventral and incisional hernia repairs: a review of the literature. Surg Today. 46(7):764–773. https://doi.org/10.1007/s00595-015-1219-y
Lambrecht JR, Vaktskjold A, Trondsen E, Øyen OM, Reiertsen O (2015) Laparoscopic ventral hernia repair: outcomes in primary versus incisional hernias: no effect of defect closure. Hernia 19(3):479–486. https://doi.org/10.1007/s10029-015-1345-x
Pawlak M, Tulloh B, de Beaux A (2020) Current trends in hernia surgery in NHS England. Ann R Coll Surg Engl. 102(1):25–27. https://doi.org/10.1308/rcsann.2019.0118
Burger JW, Luijendijk RW, Hop WC et al (2004) Long term follow up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–583. https://doi.org/10.1097/01.sla.0000141193.08524.e7
Sharma A, Mehrotra M, Khullar R, Soni V, Baijal M, Chowbey PK (2011) Laparoscopic ventral/incisional hernia repair: a single centre experience of 1242 patients over a period of 13 years. Hernia 15:131–139. https://doi.org/10.1007/s10029-010-0747-z
Schoenmaeckers EJP, Wassenaar EB, Raymakers JTFJ, Rakic S (2010) Bulging of the mesh after laparoscopic repair of ventral and incisional hernias. JSLS 14:541–546. https://doi.org/10.4293/108680810x12924466008240
Acknowledgements
Nothing to declare.
Funding
No funds were requested or obtained.
Author information
Authors and Affiliations
Contributions
FP: conceptualization, methodology, software, data curation, writing—original draft preparation. DD’A, AB and FMM: visualization, investigation. LB and LD: supervision. FSL, ST: software, validation, AM, CD, CG: reviewing, editing.
Corresponding author
Ethics declarations
Conflict of interest
Francesco Pizza1 MD, PhD, Dario D’Antonio1 MD, Francesco Saverio Lucido2 MD, Luigi Brusciano2 MD, PHD, Federico Maria Mongardini2 MD, Chiara Dell’Isola3 MD, Antonio Brillantino4 MD, PhD, Ludovico Docimo2 MD, PhD and Claudio Ganbardella2 MD, PhD declare that they have no competing interests. The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the research ethics board of the ASL NAPOLI 2 Nord, Naples.
Human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals per- formed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The paper is not based on a previous communication to a society or meeting.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pizza, F., D’Antonio, D., Lucido, F.S. et al. IPOM plus versus IPOM standard in incisional hernia repair: results of a prospective multicenter trial. Hernia 27, 695–704 (2023). https://doi.org/10.1007/s10029-023-02802-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-023-02802-2