Abstract
Background
Despite standardized techniques, anastomotic complications after colorectal resection remain a challenging problem. Among those, anastomotic stricture is a debilitating outcome which often requires multiple interventions and which is prone to recur. The present series investigates the long-term results of endoscopic balloon dilation for stenotic colorectal anastomosis.
Methods
Consecutive patients from a single institution who presented with an anastomotic stenosis after a colorectal resection were identified using a prospective clinical database. Medical records were systematically reviewed to detail patients’ outcomes.
Results
Over 17 years (1988–2015), 2361 consecutive patients underwent a colorectal anastomosis. Of those, 76 patients (3.2 %) suffered a symptomatic anastomotic stenosis within a median of 5 months (interquartile range (IQR) 2–13) of the index procedure. All stenoses were primarily treated by endoscopic balloon dilation. Median follow-up was 11 years (IQR 7–14). In half the patients, one to two attempts at endoscopic balloon dilation definitively relieved the stenosis. Overall, the median number of endoscopic balloon dilation required was 3 (IQR 2–3). Recurrence rates at 1 year, 3 year, and 5 year were 11, 22, and 25 %, respectively. Median time to recurrence was 12 months (IQR 3–24). Ultimately, two patients (2.6 %) underwent an operation due to failure of endoscopic treatment. All other patients (97.4 %) were treated successfully with endoscopic balloon dilation. A total of 12 patients (15.7 %) suffered a complication from endoscopic dilation. Of those, 11 were minor bleeding and one was a perforation at the level of the anastomosis. All complications were managed conservatively, and no emergency procedure was required as a consequence of attempted endoscopic balloon dilation.
Conclusion
Endoscopic balloon dilation is a safe approach to effectively relieve an anastomotic stenosis following a colorectal resection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Anastomotic stenosis is a serious complication following colorectal resection. Its reported incidence amounts up to 30 % [1–4] with a majority of stenosis occurring following stapled anastomosis rather than after a hand-sewn anastomosis [5]. Other known risk factors associated with the occurrence of an anastomotic stenosis include an anastomotic leak, bowel ischaemia, and radiotherapy [6–8].
Patients with symptomatic anastomotic stenosis typically complain about abdominal pain and cramps, constipation, and fractionated bowel evacuation. Symptoms may appear a few weeks until several years after surgery [3].
Endoscopic balloon dilation has become the procedure of choice to address a colorectal stricture. Indeed, most colorectal anastomotic stenosis can be reached with an endoscope and they so become accessible for a minimally invasive endoscopic therapy. Transanal endoscopic balloon dilation is now a widely used technique with a low morbidity and mortality in skilled hands [9, 10].
Symptomatic anastomotic stenoses that do not respond to balloon dilation are usually resected. But those operations are associated with a considerable morbidity and mortality. Hence, major complications were reported in up to 18 % of surgical procedures performed for anastomotic strictures [11–13].
However, there is a paucity of reports about the outcomes of endoscopic balloon dilation for anastomotic stenosis beyond the peri-interventional phase. In particular, long-term results are missing, although anastomotic stenoses are prone to recur. The present series report the results of endoscopic balloon dilation in one of the largest consecutive cohort of patients followed up for up to 17 years.
Materials and methods
Consecutive patients treated at a single tertiary care referral centre (Cantonal Hospital of Winterthur, Winterthur, Switzerland) were identified from a prospective clinical database, which includes all colorectal procedures. Medical records of patients who underwent a colorectal anastomosis between January 1998 and February 2015 were systematically reviewed with regard to anastomotic strictures.
Anastomotic stenoses were identified on clinical grounds or upon routine endoscopic surveillance (e.g. before a planned ostomy reversal or during oncologic follow-up). Anastomotic stenoses were classified at time of endoscopy according to Truong [11]: a grade I stenosis allowed the passage of a 10- to 20-mm probe; a grade II stenosis permitted the passage of a 5- to 9-mm probe; last a Grade III stenosis was identified whenever the bowel lumen was smaller than 5 mm. A bowel lumen greater than 20 mm excluded an anastomotic stenosis. Measurements were taken with a graded probe and photo-documented. All interventions were performed by a senior gastroenterologist trained in interventional procedures.
Endoscopy was performed under conscious sedation with intravenous titrated midazolam (5–10 mg) and pethidin (50–100 mg) as an outpatient procedure. Patients underwent a bowel preparation and/or an enema, as clinically indicated. No routine antibiotic prophylaxis was given.
Wire-guided Hercules balloon dilation catheters (Cook Medical; Limerick, Ireland) with a diameter of 12 mm were used for the initial dilation. If symptoms persisted, a bigger balloon with a diameter up to 20 mm was used in a further session. For distal anastomotic stenosis narrower than 5 mm, Savary–Gilliard bougies were used until use of balloon dilatators was possible.
The sequence of dilation was as follows: a guidewire was passed through the stenosis under combined endoscopic and fluoroscopic control. The balloon (or the bougie) was pushed through the stricture over the guidewire and positioned in the centre of the stenosis. The balloon was slowly inflated using diluted contrast agent, and the pressure was gradually increased (up to 150–200 kPa) until the waist of the stenosis was clearly delineated. The stenosis was dilated once per session by a maximum of 5 mm to minimize the risk of an intestinal perforation.
The procedure was repeated a few days later when required by the symptoms of the patient or the endoscopic findings. Success of endoscopic balloon dilation was defined by clinical improvement together with the straight passage of a regular colonoscope (≥20 mm). Once endoscopic dilation was deemed successful, further endoscopy was only performed in patients with a recurrent stenosis on clinical grounds, respectively, for the purpose of oncologic surveillance.
The primary outcome measure was the recurrence rate of strictures over time. Secondary outcome variables were the number of dilations, any peri-interventional complications, and any change in bowel habits before and after dilation. Patients were clinically followed up by the surgeon and gastroenterologist until complete resolution of symptoms. Thereafter, long-term follow-up was completed by a telephone interview taking advantage of a structured survey. For patients who died during follow-up, the general practitioner was asked to provide information pertaining to the cause of death and the clinical follow-up until death, in particular any potential stenosis recurrence after successful balloon dilation.
Continuous data were reported as median and interquartile range (IQR). Fisher’s exact was used to compare proportions and the Mann–Whitney U test to compare continuous data. Clinical predictors for anastomotic stenosis were then assessed in multivariable logistic regression with backward variable selection. Recurrence-free probability was calculated with a Cox proportional hazard model. Two-sided p values of less than 0.05 were considered statistically significant. Statistical analysis was conducted using SPSS, version 21 for Mac (SPSS Inc, New York, USA). This study was approved by the Ethical Review Board of Zurich, Switzerland, Ref.Nr. EK:07/06.
Results
A total of 76 consecutive patients with an anastomotic stenosis following a colorectal resection performed between 1988 and 2015 were retrieved. Strictures were diagnosed either on the basis of abdominal symptoms of the patients (n = 61) or during routine endoscopy before a planned stoma reversal (n = 15). All patients were primarily treated by endoscopic balloon dilation, and none presented with a closed-loop bowel obstruction.
Median age of those 43 women (57 %) and 33 men (43 %) was 72 years (IQR 61–82). The primary colorectal procedure was performed for diverticular disease (34 patients, 45 %), neoplasia (27 patients, 35 %), inflammatory bowel disease (two patients, 3 %), or another condition (13 patients, 17 %). More than half of the patients (n = 39, 51 %) underwent an open rectosigmoid resection, more than one-fifth (n = 17, 23 %) had a laparoscopic rectosigmoid resection, while another fifth (n = 16, 21 %) had a low anterior resection of the rectum. Segmental colectomies accounted for 5 % of the resections performed (n = 4). Table 1 provides further demographic details.
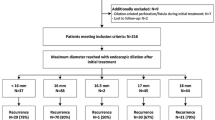
Overall, anastomotic stenoses became apparent at a median of 5 months (IQR 2–3) after the index surgery. Those that became clinically apparent were diagnosed at a median of 5 months (IQR 2–14) after surgery, whereas the median time to endoscopic diagnosis of a stenosis prior to a planned stoma reversal was 5 months (IQR 2–8), too. The severity of the stenosis was graded according to Truong as grade I in 28 patients (37 %), grade II in 22 patients (29 %), and grade III in 26 patients (34 %). Almost half of the patients (n = 37, 49 %) required more than two balloons dilations to achieve a definitive relief of the anastomosis stenosis, whereas 51 % (n = 39) were successfully treated by one to two endoscopic balloon dilations (Fig. 1).
A total of 12 patients (15.7 %) suffered a complication from endoscopic dilation. Of those, 11 were minor bleeding and one (1.3 %) was a perforation at the level of the anastomosis. All complications were managed conservatively, and no emergency procedure was required as a consequence of attempted endoscopic balloon dilation. Success rate in terms of definitive relief of the anastomotic stenosis was 100 % in those patients who suffered a complication after endoscopic dilation.
A quarter of the patients (n = 19) suffered from a recurrent stenosis with a median time to recurrence of 12 months (IQR 3–24). Recurrence rates increased with time from 11 % at 1 year, 22 % at 2 years, and 25 % at 5 years (Fig. 2). Overall, 97 % (n = 74) of the anastomotic stenosis could be permanently relieved by means of endoscopic balloon dilation. Two patients (3 %) failed repeated endoscopic balloon dilation, which was attempted for a total of 4 and 12 times, respectively. An anastomotic resection was considered in each of those two refractory stenoses. However, a stent was placed in one patient with recurrent end-stage disease and a colostomy was elected in a second patient due to considerable comorbidities.
A number of possible risk factors for the recurrence of an anastomotic stenosis were tested in univariate analysis (Table 1). The grade of anastomotic stenosis, the number of attempted dilations, and the anastomosis technique were associated with the recurrence of a stricture. In multivariate analysis, three and more attempts at endoscopic dilation and a hand-sewn anastomosis were independent predictors of a recurrence after initial successful dilation of an anastomosis stenosis (Table 2).
The distribution of hand-sewn and stapled anastomosis was not balanced in regard to anastomosis height. Hence, 9 and 18 anastomosis ≤8 cm of the anal verge were hand-sewn and stapled, respectively (p = 0.04). Conversely, above 8 cm from the anal verge, 28 and 21 anastomoses were hand-sewn anastomosis and stapled, respectively. Thirty-eight percept (14/37) of the dilated hand-sewn anastomosis recurred, while two-thirds of these recurrences (9/14) occurred within 8 cm from the anal verge.
All patients who were diagnosed with an anastomotic stricture were queried using a questionnaire. The survey response rate amounted to 88 % (67/76) with a median follow-up of 11 years (IQR 7–14). Twenty patients (26 %) died during the follow-up. In all patients who died, the cause of death was not related to the endoscopic balloon dilation nor to complications of the anastomotic stenosis. Figure 3 summarizes the bowel habits reported before and after endoscopic balloon dilation as recorded by the questionnaire.
Discussion
This study demonstrates that endoscopic balloon dilation of benign anastomotic stenosis of the lower gastrointestinal tract is a safe and highly effective procedure with low morbidity and no mortality. Even recurrent anastomotic stenoses were effectively relieved by repeat balloon dilation in almost all patients.
Data from the literature about recurrence rates after endoscopic balloon dilation are scarce [11, 14, 15]. Recurrence rates after endoscopic balloon dilation have been reported between 6 % [15] and 20 % [11] with a follow-up of only 2 and 1 year, respectively. The largest cohort included 36 patients [11] treated with balloon dilation for a stenotic colorectal anastomosis. The present study analysed the outcome of 76 patients with a median follow-up of 17 years. The long-term success rate after balloon dilation was 75 %. Most recurrences occurred during the first 2 years after balloon dilation with a definitive stenosis-free probability of 75 % after 4 years.
The observed response rate of 88 % in this study compares favourably to the average response rate of 54 % reported for mailed surveys [16]. Up to 26 % of the included patients died during the 17-year follow-up. Although their general practitioner was contacted and a possible recurrence of the anastomotic stenosis investigated, a recurrence cannot be definitively excluded. On the other hand, all patients (n = 26, 31 %) who complained about irregular bowel movements underwent a colonoscopy. No stenosis recurrence or any anatomical reasons for the reported irregular bowel movements were found. The thorough follow-up performed in the present series may minimize any potential bias caused by the retrospective analysis.
A tight or high-grade anastomotic stenosis and the number of dilations required were predictive of a recurrence in univariate analysis. In multivariate analysis, the requirement for three and more endoscopic balloon dilations and a hand-sewn anastomosis was independent risk factor for a stenosis recurrence. The latter results suggest that stenotic hand-sewn anastomosis may not respond as well to endoscopic balloon dilation than stenosis which occurred following stapler anastomosis. This finding was particularly striking in low-lying hand-sewn anastomoses, since 64 % of recurrent stenosis following hand-sewn anastomoses occurred in anastomosis performed 8 cm or below from the anal verge. No association of the occurrence/recurrence of an anastomotic stenosis with a given surgeon could be shown [17]. Although no explanation for the increased stricture susceptibility of low-lying colorectal anastomosis can be given, this observation may affect the choice of the anastomotic technique and may be important for future investigations.
Several risk factors for the development of anastomotic strictures have been reported, e.g. occurrence of an anastomotic leakage, pelvic sepsis, use of a circular stapler, and the distance to the anal verge [18]. The incidence of anastomotic strictures after colorectal anastomosis ranges between 3 and 30 % [15]. In this series, every fifth stenosis was identified during routine endoscopic evaluation before stoma reversal. Therefore, asymptomatic stenosis may have been missed in the present analysis, because asymptomatic patients are usually not subjected to an endoscopic evaluation.
In conclusion, endoscopic balloon dilation for anastomotic stenosis after colorectal resection is highly successful with low morbidity and long-time patency. Recurrent strictures appeared more often after balloon dilation of hand-sewn anastomoses than after dilated stapled anastomoses. Yet, even the most recurrent stenoses could be successfully treated with balloon dilation.
References
Kissin MW, Cox AG, Wilkins RA, Kark AE (1985) The fate of the EEA stapled anastomosis: a clinico-radiological study of 38 patients. Ann R Coll Surg Engl 67:20–22
Schlegel RD, Dehni N, Parc R, Caplin S, Tiret E (2001) Results of reoperations in colorectal anastomotic strictures. Dis Colon Rectum 44:1464–1468
Max E, Sweeney WB, Bailey HR, Oommen SC, Butts DR, Smith KW, Zamora LF, Skakun GB (1991) Results of 1000 single-layer continuous polypropylene intestinal anastomoses. Am J Surg 162:461–467
Hiranyakas A, Da Silva G, Denoya P, Shawki S, Wexner SD (2013) Colorectal anastomotic stricture: is it associated with inadequate colonic mobilization? Techn Coloproctol 17:371–375
Neutzling CB, Lustosa SA, Proenca IM, da Silva EM, Matos D (2012) Stapled versus handsewn methods for colorectal anastomosis surgery. Cochrane Database Syst Rev 2:CD003144
Orsay CP, Bass EM, Firfer B, Ramakrishnan V, Abcarian H (1995) Blood flow in colon anastomotic stricture formation. Dis Colon Rectum 38:202–206
Pahlman L, Glimelius B, Frykholm G (1989) Ischaemic strictures in patients treated with a low anterior resection and perioperative radiotherapy for rectal carcinoma. Br J Surg 76:605–606
Senagore A, Milsom JW, Walshaw RK, Dunstan R, Mazier WP, Chaudry IH (1990) Intramural pH: a quantitative measurement for predicting colorectal anastomotic healing. Dis Colon Rectum 33:175–179
Delaunay-Tardy K, Barthelemy C, Dumas O, Balique JG, Audigier JC (2003) Endoscopic therapy of benign colonic post-operative strictures: report on 27 cases. Gastroenterol Clin et Biol 27:610–613
Pietropaolo V, Masoni L, Ferrara M, Montori A (1990) Endoscopic dilation of colonic postoperative strictures. Surg Endosc 4:26–30
Truong S, Willis S, Schumpelick V (1997) Endoscopic therapy of benign anastomotic strictures of the colorectum by electroincision and balloon dilatation. Endoscopy 29:845–849
Genser L, Manceau G, Karoui M, Breton S, Brevart C, Rousseau G, Vaillant JC, Hannoun L (2013) Postoperative and long-term outcomes after redo surgery for failed colorectal or coloanal anastomosis: retrospective analysis of 50 patients and review of the literature. Dis Colon Rectum 56:747–755
Lefevre JH, Bretagnol F, Maggiori L, Ferron M, Alves A, Panis Y (2011) Redo surgery for failed colorectal or coloanal anastomosis: a valuable surgical challenge. Surgery 149:65–71
Belvedere B, Frattaroli S, Carbone A, Viceconte G (2012) Anastomotic strictures in colorectal surgery: treatment with endoscopic balloon dilation. Il G di Chir 33:243–245
Fregonese D, Di Falco G, Di Toma F (1990) Balloon dilatation of anastomotic intestinal stenoses: long-term results. Endoscopy 22:249–253
Asch DA, Jedrziewski MK, Christakis NA (1997) Response rates to mail surveys published in medical journals. J Clin Epidemiol 50:1129–1136
Tuson JR, Everett WG (1990) A retrospective study of colostomies, leaks and strictures after colorectal anastomosis. Int J Colorectal Dis 5:44–48
Pucciarelli S, Toppan P, Pilati PL, Piccoli A, Chemello F, Lise M (1994) Efficacy of dilatations for anastomotic colorectal stenoses: prognostic factors. Int J Colorectal Dis 9:149–152
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Magdalena Biraima, Michel Adamina, Res Jost, Stefan Breitenstein, and Christopher Soll have no conflict of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Biraima, M., Adamina, M., Jost, R. et al. Long-term results of endoscopic balloon dilation for treatment of colorectal anastomotic stenosis. Surg Endosc 30, 4432–4437 (2016). https://doi.org/10.1007/s00464-016-4762-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-4762-8