Abstract
Background
Inguinal hernia repair is the most common surgery in the world. Health-related quality of life (HRQOL) outcomes are arguably the most important elements of successful repair. This study is aimed to describe short- and long-term quality of life outcomes in patients undergoing laparoscopic inguinal hernia repair.
Methods
We prospectively followed patients who underwent totally extraperitoneal laparoscopic inguinal hernia repair (TEP) as part of an Institutional Review Board-approved study. HRQOL was measured preoperatively, or 3 weeks, 6 months, and 1 year postoperatively using Short Form 36 Health Survey Version 2 (SF-36v2) and Carolinas Comfort Scale. Postoperative HRQOL scores were compared to baseline using paired t tests.
Results
Between June 2009 and February 2014, 1,175 patients underwent TEP by four surgeons. Of those, 301 patients with 388 hernias were registered in the database and followed by a research coordinator. Mean age was 56.4 ± 15.2 years and 93 % were male. Mean body mass index was 26.1 ± 3.7 kg/m2. Seventy-eight percent presented with pain, the majority of which were described as mild. Hernias were unilateral right-sided in 43 %, left-sided in 28 %, and bilateral in 29 %. Eighty-five percent were primary hernias. Average operative time was 43.5 ± 17.9 min and there were no intraoperative complications. Urinary retention occurred in 6 %. Visual analog scale at discharge was 1.9 ± 1.7. Analgesics were used an average of 2.5 ± 3.4 days and return to activities of daily living and work occurred on postoperative 5.5 ± 4.4 and 5.6 ± 3.9 days. Recurrence occurred in 2.1 %. Significant improvements between baseline and 1 year were found in role limitations due to physical health (81.5 ± 25.6 vs. 91.8 ± 19.4, p = 0.02), social functioning (87.4 ± 21.3 vs. 92.9 ± 15.3, p = 0.02), and pain (78.2 ± 19.7 vs. 86.6 ± 15.9, p = 0.007).
Conclusions
TEP results in significant improvement in HRQOL including physical health, social functioning, and pain at 1 year. On average, patients are able to return to activities of daily living and work within a week.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Inguinal hernia is the most common operation performed in the world and surgical repair continues to be the definitive treatment [1]. In the United States alone, approximately 700,000 hernia repairs are performed annually [2]. Fortunately, this high-volume surgery is associated with a low morbidity and mortality and thus, quality and success of herniorrhaphy is increasingly being measured by patient-centered outcomes through quality of life measures in the short and long term.
The majority of studies assessing quality of life after open repair have shown improvement when compared to the patients’ reported preoperative state [3–8]. Instruments used to measure health-related quality of life vary, though SF-36® remains one of the most common. Most studies show improvement in physical and social function, as well as pain after open repair [7, 9–11].
The first reported laparoscopic repair of an inguinal hernia was in 1992 [12]. Since then, several studies have shown that laparoscopic repair, when performed by experienced surgeons, results in reduced postoperative pain and morbidity, an earlier recovery, and more rapid return to work when compared to open repair [13–17]. Some have gathered SF-36® responses from patients at various time points after laparoscopic repair but few have been able to compare long-term data to those of the preoperative period [10, 14, 18–21]. This study presents quality of life data measured through the SF-36® instrument, prior to and up to 1 year after laparoscopic total extraperitoneal repair (TEP) of groin hernias in an ambulatory population.
Materials and methods
Study protocol
Patients aged 18 and over who were examined by the four participating surgeons at NorthShore University HealthSystem were offered participation in the prospective hernia database through a consent form and explanation by the surgeon. The database is approved by the Institutional Review Board and data gathered by a research coordinator. Self-reported health-related quality of life (HRQOL) questionnaires were distributed to the patients either in person or by mail preoperatively, and postoperatively at 3 weeks, 6 months, 1 year, and 2 years. For the purpose of this study, only patients undergoing laparoscopic totally extraperitoneal repair of a primary or recurrent, unilateral or bilateral groin hernia (indirect, direct, or femoral) were analyzed. Patients who underwent simultaneous repair of an umbilical or ventral hernia were excluded.
TEP technique
Four surgeons performed TEP and enrolled patients in the study. All four had experience of at least 100 TEP repairs prior to enrolling patients. Antibiotics (most often a first-generation cephalosporin) were administered prior to incision in all cases. General endotracheal anesthetic was utilized for all cases and a urinary catheter was placed in some patients prior to incision. There was slight variation among the surgeons in terms of technique, however, all used two 5-mm and one 12-mm ports. The extraperitoneal space was entered in the infraumbilical region lateral to the midline on the ipsilateral side of the hernia. Only the anterior rectus sheath was incised, and the port was placed posterior to the rectus muscle. If a bilateral repair was performed, no additional ports were placed. A dissecting balloon was used in some cases but not all based on surgeon preference. Insufflation with carbon dioxide was limited to 12 mmHg. After creation of the extraperitoneal working space, the hernia sac was reduced. Two mesh types were used in this patient cohort and both were used similarly to cover the entire myopectineal orifice from the symphysis pubis to the anterior superior iliac spine laterally. The majority of mesh was 15 × 10 cm and flat without an opening or slit for the spermatic cord. On occasions when the hernia size was large (generally >4 cm diameter), a 16 × 12 cm mesh with a flap or slit for the spermatic cord was used. Tacks (absorbable or permanent) were used in some but not all cases based on surgeon preference. When used, tacks were placed laterally above the iliopubic tract, medially on Cooper’s ligament, and anterior to the rectus muscle. The anterior rectus sheath was closed with an absorbable suture at the completion of the case.
Postoperative data collection
HRQOL questionnaires were distributed to the patients either in person or by mail preoperatively, and postoperatively at 3 weeks, 6 months, 1 year, and 2 years. All patients were asked to return to clinic 3 weeks after the procedure. A research coordinator assessed postoperative complications through review of the patients’ electronic medical record. A recurrence was noted if found on subsequent physical exam or imaging. Patients were also asked about recurrence through the mailed questionnaires and the data were cross-referenced with their medical record. Any inconsistency was further verified by research nurse and project coordinator.
Health-Related Quality of Life Outcome Measures
Short Form 36 Health Survey Version 2 (SF-36v2) ® consists of 36 items that are used to calculate eight subscales: physical functioning, role physical, bodily pain, general health perception, vitality, social functioning, role emotional, and mental health. The subscales are transformed into values ranging from 0 (poor health) to 100 (best health). The SF-36v2® has been suggested as a core HRQOL outcome instrument and has been applied frequently in hernia patients [7, 9–11, 14, 18–21].
Carolinas Comfort Scale (CCS)
This metric was purchased and given to patients at all of the postoperative time points. The instrument was developed to evaluate and track the quality of life outcome particularly for patients undergoing hernia surgery [22]. The CCS scale has been statistically validated against other well-studied and validated assessment tools and is considered a valid QOL assessment in hernia patients.
Other data including preoperative, intraoperative, and postoperative characteristics were also collected through the patients’ electronic medical record
Statistical analysis
Patient demographics, preoperative, intraoperative, and postoperative characteristics were summarized as frequency counts with percentages for categorical variables and means with standard deviations for continuous variables. HRQOL SF-36v2 and CCS scores were calculated at each time point and were compared between baselines and at 3 weeks, 6 months, and 1 year postoperatively using paired t tests. Multiplicity was adjusted using Bonferroni correction method. Data were analyzed using SAS 9.3 software (SAS Inc., Cary, NC) and a p value of <0.05 was considered significant.
Results
Patient preoperative characteristics
Between June 2009 and February 2014, 1,175 adult patients underwent TEP by one of the four participating surgeons. Of those, 301 patients with 388 groin hernias were consented and agreed to participate in our prospective database. All of the patients participating in this study underwent elective repair and a surgical resident participated in the majority of cases. Patient demographics and preoperative characteristics are shown in Table 1. Mean age was 56.4 ± 15.2 years and 93 % were male. Mean body mass index was 26.1 ± 3.7 kg/m2. Seventy-eight percent presented with pain at baseline, the majority of which were described as mild. Hernias were unilateral right-sided in 43 %, left-sided in 28 %, and bilateral in 29 %. Among them, eighty-five percent were primary hernias (Table 1).
Intraoperative period
A dissecting balloon was used 31 % of the time. The average operative time was 43.5 ± 17.9 min. A tacker was used 66 % of the time, 80 % of which were absorbable tacks. An average of 5.2 ± 3.3 tacks were used for unilateral cases (10.2 ± 3.3 for bilateral) during which tacks were used. Macroporous polyester mesh (Parietex™ anatomical) was used in 65 % of the cases. Macroporous polypropylene mesh (Physiomesh®) was used 31 % of the time. Mesh size was 15 × 10 cm 97 % of the time. The other 3 % of the time, a 16 × 12 cm polyester mesh with a slit through which the spermatic cord traversed, was utilized. There were no intraoperative surgical or anesthetic (i.e., cardiopulmonary) complications. There were no conversions to open.
Postoperative period
The average length of stay (including time prior to the operation) was 10.8 ± 22.8 h. Nineteen (6.3 %) patients returned to the Emergency Department within 24 h of the procedure. There were 22 (7 %) admissions and seven (2.3 %) readmissions (Table 2). There were no mortalities. Early complications occurred in 23 % and are included in Table 2. There was only one severe complication (scrotal abscess requiring reoperation and drainage). There were no mesh-related complications.
Narcotic pain medications were stopped on postoperative day 2.5 ± 3.4 on average. Of those that returned home on the day of surgery, 27.4 % of patients did not require narcotic pain medications after discharge from the hospital.
Patients were asked on which postoperative day they were able to return to activities of daily living (ADL) including cleaning, cooking, bathing, and shopping. The mean return to ADL was 5.5 ± 4.4 days and return to work 5.6 ± 3.9 days.
There were a total of 133 phone calls by 35.9 % of the patients in the period between discharge from the hospital and the patient’s first postoperative clinic visit. The reasons for calling are shown in Table 3. The majority of the calls were due to questions regarding care of the wounds as well as pain followed by urinary and bowel issues.
Recurrences occurred in 2.1 % (8/388) of hernias repaired. The average number of days from surgery to recurrence was 432.4 ± 264.2 days. A higher recurrence rate was noted after the switch from polyester to polypropylene mesh (1.0 vs. 5.3 %) resulting in the surgeons converting back to the use of the polyester mesh at the midpoint of the data collection period. Of the eight recurrences, five were primary hernias and three were recurrent. All eight recurrences were in males. The number of recurrences was split evenly between the first and second half of the study (four in each).
Health-related quality of life
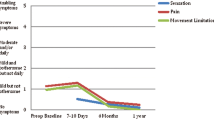
Of the 301, 43.8 % of the patients completed preoperative SF-36v2® forms. Postoperatively, 56 % of the 301 patients completed the same SF-36® forms at 3 weeks, 20 % at 6 months, 40 % at 1 year, and 8 % at 2 years. The 6 months, 1 year, and 2 years forms were mailed to the patients. Due to the relatively low percentage of patients reaching 2 years, the 2-year data were excluded. Figure 1 depicts the SF-36 data compiled.
Physical functioning
The average preoperative score was 84.0 ± 22.4 and there was no significant change at 3 weeks postoperatively (85.1 ± 21.1, p = 0.80). 6 months postoperatively, the score was nearly significantly improved from baseline to 92.8 ± 14.7 (p = 0.05), and this remained relatively unchanged at 1 year postoperatively (88.0 ± 23.3, p = 0.49).
Role limitations due to physical health
The average preoperative score was 81.5 ± 25.6 and this score decreased slightly, though not significantly, at 3 weeks postoperatively to 72.9 ± 28.6. This subscale significantly improved from baseline at 6 months and 1 year (92.0 ± 19.7, p = 0.049 and 91.8 ± 19.4, p = 0.02 respectively).
Role limitations due to emotional problems
The average preoperative score was 90.4 ± 17.2 which remained unchanged at 3 weeks and 6 months after surgery (91.7 ± 15.4 and 90.4 ± 18.5). At 1 year, there was a statistically significant improvement in this subscale to 94.1 ± 11.8, p = 0.03.
Energy and fatigue
The average preoperative score was 70.3 ± 18.6 which decreased to 66.3 ± 20.5, though not significantly (p = 0.11). There were no significant improvements in this subscale at any point: 6 months 69.6 ± 18.6, p = 0.14 and 1 year 71.9 ± 19.3, p = 0.93.
Emotional well-being
The mean preoperative score was 79.5 ± 14.5 which remained similar at 3 weeks (79.2 ± 13.6, p = 0.77), 6 months (80.9 ± 12.8, p = 0.81), and 1 year (84.1 ± 11.1, p = 0.12).
Social functioning
This subscale was significantly improved from baseline (87.4 ± 21.3) at 1 year (92.9 ± 15.3, p = 0.02), but not significantly different at 3 weeks (82.6 ± 22.4, p = 0.29) or 6 months (95.0 ± 10.1, p = 0.142).
Pain
Pain significantly worsened from baseline (78.2 ± 19.7) at 3 weeks (67.4 ± 23.3, p = 0.005), but improved at 6 months (82.9 ± 16.1, p = 0.14), and was significantly less at 1 year postoperatively (86.6 ± 15.9, p = 0.007).
General health
This subscale was not significantly different from baseline (77.6 ± 18.6) at any time point: 3 weeks (79.7 ± 17.2, p = 0.74), 6 months (81.0 ± 16.4, p = 0.18), and 1 year (78.2 ± 23.4, p = 0.26).
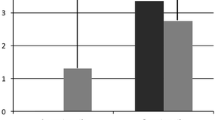
CCS
Scores are presented in Table 4. There was notable improvement over time in all subscales. Figure 2 presents those patients with various levels of symptoms at 1 year after repair. Less than two percent had moderate or worse pain and no one reported disabling symptoms.
In order to see whether lighter weight mesh resulted in improved quality of life scores, CCS was used to compare various factors. Physiomesh® scored significantly better than Parietex™ in terms of total score at 1 year (0.34 vs. 3.85, p = 0.003). Mesh size, age, gender, and the presence of pain preoperatively did not result in any significant difference at any postoperative point.
Patients whose surgery utilized a balloon were compared to those that did not have a balloon and there was no difference in quality of life outcomes both in CCS and SF-36® subscales. Similar comparisons were performed analyzing fixation type and again no differences were found.
Discussion
This study demonstrated significant improvements in several quality of life parameters after TEP repair of various types of groin hernias in an ambulatory population. Several studies have previously reported SF-36® data in patients after laparoscopic groin hernia repair but are limited in their retrospective nature and sometimes lack of baseline data along with long-term (1 year or greater) responses [10, 14, 18–21]. Some have suggested that only prospective studies are useful in assessing quality of life parameters as patients tend to over or underestimate symptoms when asked retrospectively which led to the formation of this study [3].
In addition, the more serious complications and high recurrence rates in studies published previously may have reflected the early learning curve as they were not evident in this series [23]. The majority of complications in this series were due to urinary retention and seroma/hematoma formation. Similar rates of seroma formation have been found in previous studies and may be a difficult complication to avoid [24]. In terms of urinary retention, there is a disparity in the literature in range of 1–22 % [25–27]. It is possible that recall bias may play a role and electronic medical records may improve the accuracy in future gathering of this particular data.
The recurrence rate in this cohort is lower than those previously published and in line with more recent reports. Admittedly, this study is limited in terms of accurate recurrence rates given that others have shown that recurrences are often missed when self-reported and not formally examined by a specialist [15, 28]. Interestingly, a switch from polyester (Parietex™ anatomical) to a slightly lighter weight mesh (Physiomesh®) was done with hopes to decrease long-term postoperative pain. Carolina Comfort Scores™ at 1 year confirmed this to be the case, however, at the expense of a significantly higher recurrence rate. We hypothesize that given our tendency to avoid tacking and the probable longer tissue in-growth duration with a Monocryl-laminated mesh, migration played a role in the significant increase in recurrences (1.0–5.3 %). Participating surgeons in this study have since converted back to polyester mesh.
Chronic pain continues to be of concern after hernia repair. Complaints of persistent pain after open repair range from 0 to 60 % but do appear to be lower after laparoscopic approaches [15, 28–31]. The patient cohort was too small to accurately perform an analysis of predictors, however others have shown that young age and recurrent hernia predict chronic pain [32]. In this prospective cohort, the pain subscale of the SF-36® was significantly improved at 1 year as compared to baseline. Still, however, 13 % of patients reported a worse pain score at 1 year when compared to baseline. When the more specific CCS instrument was used however, extremely few (<2 %) reported any bothersome pain at 1 year as illustrated in Fig. 2. We believe this illustrates the weakness of using an instrument, such as SF-36®, in a surgical population.
Unfortunately, one of the weaknesses of SF-36® may be its lack of specificity in regards to specific surgical diseases and postoperative states. Though specific quality of life instruments have been developed for hernia repair, such as the Carolina Comfort Scale™, there is still a need for instruments that can be benchmarked against other diseases and treatments. Unfortunately, SF-36® was not developed with the surgical patient in mind. Ideally, an instrument that is able to assess a surgical patient’s overall health in addition to a specific life instrument could be used.
Limitations of this study include the fact that the patients of four different surgeons were included and the procedure was not standardized among them. Another limitation is that 301 of 1,175 patients enrolled in our database over the time period. This was due, in part, to an imbalance in our volume and number of coordinators in our research office for a period of a few months in the mid-portion of our data collection period during which recruitment and consent for patients, as well as mailings of follow-up quality of life surveys, were limited to one coordinator who could not meet the demands. After the midpoint, two additional coordinators were added and follow-up and recruitment improved. This did result in inconsistent survey responses, however, we feel the 301 patients are a representative sample of the eligible patient population.
In conclusion, laparoscopic total extraperitoneal repair of groin hernias results in a low recurrence and morbidity rate, and significant improvement in HRQOL including physical health, social functioning, and pain at 1 year. Less than 2 % of patients report bothersome symptoms in the groin at 1 year.
References
Bay-Nielsen M, Kehlet H, Strand L, Malmstrom J, Andersen F, Wara P, Juul P, Callesen T (2001) Quality assessment of 26,304 herniorrhaphies in Denmark: a prospective nationwide study. Lancet 358:1124–1128
Rutkow I (1998) Epidemiologic, economic, and sociologic aspects of hernia surgery in the United States in the 1990s. Surg Clin N Am 78:941–951
Palmqvist E, Larsson K, Anell A, Hialmarsson C (2013) Prospective study of pain, quality of life, and the economic impact of open inguinal hernia repair. Br J Surg 100:1483–1488
Magnusson J, Videhult P, Gustafsson U, Nygren J, Thorell A (2014) Relationship between preoperative symptoms and improvement of quality of life in patients undergoing elective inguinal herniorrhaphy. Surgery 155:106–113
Bitzer E, Lorenz C, Nickel S, Dorning H, Trojan A (2008) Patient-reported outcomes in hernia repair. Hernia 12:407–414
Mathur S, Bartlett A, Gilkison W, Krishna G (2006) Quality of life assessment in patients with inguinal hernia. ANZ J Surg 76:491–493
Zieren J, Kupper F, Paul M, Neuss H, Muller J (2003) Inguinal hernia: obligatory indication for elective surgery? A prospective assessment of quality of life before and after plug and patch inguinal hernia repair. Langenbecks Arch Surg 387:417–420
Lawrence K, Jenkinson C, McWhinnie D, Coulter A (1997) Quality of life in patients undergoing inguinal hernia repair. Ann R Coll Surg Engl 79:40–45
Post S, Weiss B, Willer M, Neufang T, Lorenz D (2004) Randomized clinical trial of lightweight composite mesh for Lichtenstein inguinal hernia repair. Br J Surg 91:44–48
Wellwood J, Sculpher M, Stoker D, Nicholls G, Geddes C, Whitehead A, Singh R, Spiegelhalter D (1998) Randomised controlled trial of laparoscopic versus open mesh repair for inguinal hernia: outcome and cost. BMJ 317:103–110
Barrat C, Seriser F, Arnoud R, Trouette P, Champault G (2004) Inguinal hernia repair with beta glucan-coated mesh: prospective multicenter study (115 cases)—preliminary results. Hernia 8:33–38
Arregui M, Davis C, Yucel O, Nagan R (1992) Laparoscopic mesh repair of inguinal hernia using a preperitoneal approach: a preliminary report. Surg Laparosc Endosc 2:53–58
Singh A, Bansal V, Misra M, Kumar S, Rajeshwari S, Kumar A, Sagar R, Kumar A (2011) Testicular functions, chronic groin pain, and quality of life after laparoscopic and open mesh repair of inguinal hernia: a prospective randomized controlled trial. Surg Endosc 26:1304–1317
Abbas A, Abd Ellatif M, Noaman N, Negm A, El-Morsy G, Amin M, Moatamed A (2012) Patient-perspective quality of life after laparoscopic and open hernia repair: a controlled randomized trial. Surg Endosc 26:2465–2470
Eker H, Langeveld H, Klitsie P, Van’t Riet M, Stassen L, Weidema W, Steyerberg E, Lange J, Bonjer H, Jeekel J (2012) Randomized clinical trial of total extraperitoneal inguinal hernioplasty vs Lichtenstein repair: a long-term follow-up study. Arch Surg 147:256–260
Grant A, Scott N, O’Dwyer P (2004) Five-year follow-up of a randomized trial to assess pain and numbness after laparoscopic or open repair of groin hernia. Br J Surg 91:1570–1574
Memon M, Cooper N, Memon B, Memon M, Abrams K (2003) Meta-analysis of randomized clinical trials comparing open and laparoscopic inguinal hernia repair. Br J Surg 90:1479–1492
Myers E, Browne K, Kavanagh D, Hurley M (2010) Laparoscopic (TEP) versus Lichtenstein inguinal hernia repair: a comparison of quality-of-life outcomes. World J Surg 34:3059–3064
Dhankhar D, Sharma N, Mishra T, Kaur N, Singh S, Gupta S (2014) Totally extraperitoneal repair under general anesthesia versus Lichtenstein repair under local anesthesia for unilateral inguinal hernia: a prospective randomized controlled trial. Surg Endosc 28:996–1002
Kallianpur A, Parshad R, Dehran M, Hazrah P (2007) Ambulatory total extraperitoneal inguinal hernia repair: feasibility and impact on quality of life. JSLS 11:229–234
Pokorny H, Klingler A, Scheyer M, Fugger R, Bischof G (2006) Postoperative pain and quality of life after laparoscopic and open inguinal hernia repair: results of a prospective randomized trial. Hernia 10:331–337
Heniford B, Walters A, Lincourt A, Novitsky Y, Hope W, Kercher K (2008) Comparison of generic versus specific quality-of-life scales for mesh hernia repairs. JACS 206:638–644
Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R Jr, Dunlop D, Gibbs J, Reda D, Henderson W (2004) Open mesh versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 350:1819–1827
Hawn M, Itani K, Giobbie-Hurder A, McCarthy M Jr, Jonasson O, Neumayer L (2006) Patient-reported outcomes after inguinal herniorrhaphy. Surgery 140:198–205
Wauschkuhn C, Schwarz J, Boekeler U, Bittner R (2010) Laparoscopic inguinal hernia repair: gold standard in bilateral repair? Results of more than 2800 patients in comparison to the literature. Surg Endosc 24:3026–3030
Winslow E, Quasebarth M, Brunt L (2004) Perioperative outcomes and complications of open vs laparoscopic extraperitoneal inguinal hernia repair in a mature surgical practice. Surg Endosc 18:221–227
Koch C, Grinberg G, Farley D (2006) Incidence and risk factors for urinary retention after endoscopic hernia repair. Am J Surg 191:381–385
Staerkle R, Buchli C, Villiger P (2009) Patient satisfaction, hernia recurrence rate, and chronic pain 10 years after endoscopic total extraperitoneal inguinal hernia repair. Surg Laparosc Endosc Percutan Tech 19:405–409
Inaba T, Okinaga K, Fukushima R, Ikeda Y, Yamazaki E, Koide T, Horikawa M, Inoue T, Ogawa E (2012) Chronic pain and discomfort after inguinal hernia repair. Surg Today 42:825–829
Alfieeri S, Amid P, Campanelli G, Izard G, Kehlet H, Wijsmuller A, Di Miceli D, Doglietto G (2011) International guidelines for prevention and management of post-operative chronic pain following inguinal hernia surgery. Hernia 15:239–249
Reinpold W, Nehls J, Eggert A (2011) Nerve management and chronic pain after open inguinal hernia repair: a prospective two phase study. Ann Surg 254:163–168
Ali S, Zendejas B, Yadav S, Hernandez-Irizarry R, Lohse C, Farley D (2013) Predictors of chronic groin discomfort after laparoscopic totally extraperitoneal inguinal hernia repair. JACS 217:72–78
Acknowledgments
The authors would like to acknowledge the Grainger Foundation for generous financial support that made this project possible.
Disclosures
Michael B. Ujiki, Matthew E. Gitelis, Joann Carbray, Brittany Lapin, John Linn, Steven Haggerty, Chi Wang, Ryota Tanaka, Ermilo Barrera, Zeeshan Butt and Woody Denham have no any relevant conflicts of interest with respect to the authorship and or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ujiki, M.B., Gitelis, M.E., Carbray, J. et al. Patient-centered outcomes following laparoscopic inguinal hernia repair. Surg Endosc 29, 2512–2519 (2015). https://doi.org/10.1007/s00464-014-4011-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-4011-y