Abstract
Background
When considering an asymptomatic inguinal hernia, surgeons must weigh the risks of watchful waiting against the risk of operative complications. Laparoscopy offers the benefit of reduced postoperative pain, which, for appropriate surgical candidates, may strengthen the case for repair. This study compares general and disease-specific quality of life following totally extraperitoneal (TEP) laparoscopic inguinal hernia repair (LIHR) of asymptomatic and symptomatic hernias.
Methods
We summarize prospective data from 387 patients who underwent TEP LIHR between 2009 and 2015 by four surgeons at a single institution. Asymptomatic individuals were identified by pain scores of zero at preoperative clinic visits. Validated quality of life (QOL) measurements were administered preoperatively and at 3 weeks, 6 months, and 1-year postop. Comparisons were made using Chi-square test, t test, or Mann–Whitney U test. Changes over time were assessed using longitudinal mixed effects models.
Results
A cohort of 79 asymptomatic cases were compared to 308 symptomatic individuals. The asymptomatic cohort had larger median hernia defects (2.5 vs 2 cm, p < 0.01), was older (mean 63.0 vs 58.9 years, p = 0.03), included fewer indirect hernias (57.7 vs 74.9%, p < 0.01), took pain medication for fewer days (mean 1.2 ± 1.5 vs 2.2 ± 3.0 days, p = 0.02), returned to baseline activities of daily living earlier (median 3 vs 5 days, p < 0.01), and reported decreased postoperative pain (p = 0.02). There was no significant difference in general QOL. There was one recurrence in the asymptomatic group and were two in the symptomatic cohort.
Conclusions
Asymptomatic individuals undergoing TEP LIHR reported less postoperative pain, returned to baseline activities, and discontinued pain medication sooner than symptomatic patients. These results are encouraging and may inform patient-centered discussions about asymptomatic hernia repair.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Symptoms in the presence of inguinal hernia vary widely from completely asymptomatic to disabling pain [1, 2]. Lifetime risk for developing an inguinal hernia is 27% for men and 3% for women, and inguinal hernia repair (IHR) is the most commonly performed operation in the United States, with an incidence of 28 per 100,000 individuals [3, 4]. IHR has a number of well-known early and late surgical complications. Early complications include urinary retention, hematoma, and surgical site infection. Among late complications are recurrence, chronic pain, numbness, and fertility problems for men [5]. Chronic pain is generally defined as pain persisting beyond 3 months, and up to one-third of individuals will report some degree of chronic discomfort after IHR when asked on anonymous surveys. This figure drops to 10% when asked in clinic, with 3% experiencing pain significant enough to interfere with daily life [6]. Fertility problems can arise from injury to the spermatic cord in males. Unilateral injury to the vas deferens occurs in up to 0.3% of adult repairs. Injury of the testicular artery occurs in up to 0.5% and can lead to testicular atrophy [7]. As with any surgery, IHR carries a risk of death. A Danish study on over 26,000 hernia repairs found mortality rate to be 0.02% for those under 60 years of age, and 0.48% for those over [8].
The advent of laparoscopy brought new surgical approaches to IHR, and rigorous analysis comparing laparoscopic techniques to open has determined that the laparoscopic approach offers less postoperative pain, faster return to daily activities, and overall fewer complications [9, 10]. The laparoscopic repair has also been associated with less chronic pain than open repair [11]. On the other hand, the laparoscopic approach is more expensive and requires longer operative time [9, 10]. Both approaches are considered acceptable, and The National Institute for Health and Clinical Excellence recommends that patients should be educated to the risks and benefits carried by both techniques prior to surgery [12].
Given the rare but significant operative risks, recommending IHR must be approached on a case-by-case basis. Surgery is generally recommended for individuals experiencing symptoms when impact on quality of life seems to outweigh the small rate of complications. However, the question becomes more complicated when considering asymptomatic hernias. In the era of open surgery, a ‘watchful waiting’ approach was considered appropriate management for asymptomatic hernias. Watchful waiting carries its own risks; incarcerated and strangulated hernias are surgical emergencies, with delay being potentially fatal. While the risk of incarceration is low, at just 0.55% over 4 years, emergent repair is associated with increased morbidity and mortality, and watchful waiting is associated with a 1.59 odds-ratio of having emergency hernia surgery [13, 14]. Additionally, up to 68% of individuals with asymptomatic hernias eventually develop symptoms and end up having surgery at an older age [15]. With advancing technology and decreasing complication rates, the watchful waiting approach has been called into question, and several studies have compared watchful waiting to elective repair. Individual studies have failed to show a significant difference in chronic pain, and both approaches have been deemed safe forms of management [16,17,18]. This study is a review of an institutional database aimed to examine outcomes and quality of life (QOL) after laparoscopic inguinal hernia repair (LIHR) using totally extraperitoneal (TEP) technique.
Methods
A prospectively collected database of all patients undergoing hernia repair between 2009 and 2015 was queried for those who underwent LIHR by TEP technique. Elective operations on primary, recurrent, unilateral, and bilateral inguinal hernias were included. Tacks were used for all cases of mesh fixation. General guidelines for fixation were direct hernias >2 cm and indirect hernias >6 cm, although some surgeons in the group use fixation more liberally. Hernia defect size was estimated intraoperatively using an open laparoscopic grasper as a reference. The asymptomatic cohort was populated with individuals who orally reported a pain score of zero to their surgeon at their preoperative clinic visit. Patients were asked to complete quality of life questionnaires preoperatively, and postoperatively at 3 weeks, 6 months and 1 year.
Health-related quality of life assessment tools
In total, three comprehensive quality of life instruments, encompassing both generic and surgery specific elements, were distributed to patients. The Short Form 36 Health Survey Version 2 (SF-36) commonly used to assess patients’ overall health status at any given time, consists of 36 total items divided amongst eight different categories. Responses are scored on a Likert scale [19]. Value of this scale in a surgical setting is limited, however, given the acute changes around the time of surgery are not reflected in this survey.
The Surgical Outcomes Measurement System (SOMS) is a relatively new comprehensive collection of measures specifically assessing patients in the postoperative state, regardless of the type of operation they had. Similar to SF-36, SOMS encompasses 34 items included within seven quality of life domains: pain on a visual analog scale (VAS), pain impact, pain quality, fatigue, physical functioning, body image, and satisfaction. Despite similarities to SF-36, SOMS is more specific to the surgical patient.
The Carolinas Comfort Scale (CCS), the most commonly used validated QOL instrument for hernia surgery, consists of 8 questions specific to pain, movement limitations, and the sensation of mesh experienced after hernia repair. Each question is scored on a 6-point Likert scale (0 = No symptoms, 2 = Mild and bothersome, and 5 = Disabling symptoms) where the best possible score is 0 [20].
Over the course of the study, the QOL instruments administered varied slightly as new measures were added. Since 2009, SF-36 has been distributed to all patients pre- and postoperatively. In 2011 and 2012, CCS and SOMS were respectively added to the study protocol. CCS has only been administered postoperatively due to the nature of questions pertaining to mesh sensation. The SOMS tool, in its entirety, was given preoperatively and a modified version—SOMS Short Form, limited to the domains of Body Image, Pain Impact, Pain Quality, and Satisfaction, given postoperatively since being acquired.
Statistical methods
Data are presented as frequency count with percentage for categorical variables and mean with standard deviation or median with interquartile range for continuous variables. Patient demographics, intra-operative characteristics, postoperative outcomes, and QOL assessments were compared between asymptomatic and symptomatic hernia patients. Categorical variables were compared using Chi-square test or Fisher’s exact test (for small cell size), and continuous variables were compared using t test or Mann–Whitney U test (nonparametric). Change in QOL assessments over time was assessed using mixed-effects linear regression models with an unstructured covariance structure controlling for random effects of intercept. An interaction term between group (symptomatic vs asymptomatic) and time was included to assess differential effects of QOL across time by group, with interactions considered significant at p < 0.05. Additional analyses adjusted for age. Statistical significance was established through at p < 0.05. All statistical analyses were performed using SAS 9.3 statistical software (SAS Inc. Cary, NC).
Results
Of 638 TEP LIHR patients in the database from 2009 to 2015, 387 had the necessary data available after chart review. A cohort of 79 patients (20.4%) reported a pain score of 0 at their preop clinic visit and were compared to 308 symptomatic individuals. Demographic comparisons are shown in Table 1. The groups had a similar gender distribution and incidence of comorbidities. The asymptomatic cohort was older than the symptomatic cohort (63.0 vs 58.9 years, p = 0.03). Intraoperative findings (Table 2) revealed the asymptomatic cohort had larger median hernia defects (2.5 vs 2 cm, p < 0.01) and included fewer indirect hernias (57.7 vs 74.9%, p < 0.01). Operative time and hernia laterality were similar. Mesh fixation was used in about 55% of cases, and tacks were the consistently used method. Analysis of postoperative variables (Table 3) showed that the asymptomatic patients took pain medication for fewer days on average (1.2 ± 1.5 vs 2.2 ± 3.0 days, p = 0.02), and returned to baseline activities of daily living earlier (median 3 vs 5 days, p < 0.01). There was one recurrence in the asymptomatic group, and two in the symptomatic group. All three of the recurrences occurred in individuals with indirect hernias, and two of the three had mesh fixation with tacks at the time of surgery.
46.5% of individuals who reported zero pain in clinic reported pain on the VAS pain score included in the SOMS questionnaire preoperatively, with an average score of 1.30. The average clinic pain score of the symptomatic group was higher than the SOMS reported score (3.35 vs 2.74, p < 0.01). The asymptomatic group’s preop SOMS VAS score remained significantly different from the symptomatic group’s (1.30 vs 2.74, p < 0.01). Over time, SOMS VAS score remained significantly different at 3 weeks, but not at 6 months or 1 year (Table 4).
There were no significant differences in postoperative complications between the cohorts. Rates of seroma, hematoma, and surgical site infection are within range of rates reported in the literature. Rate of urinary retention has been reported from 1.3 to 5.8% in prior studies [21]. In this analysis, the asymptomatic and symptomatic cohorts respectively experienced urinary retention at a rate of 8.6 and 6.0%. The higher rate seen in the asymptomatic cohort may also be explained by the older age of this group.
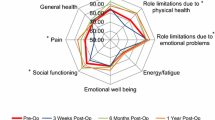
Longitudinal mixed-effects models indicated CCS Pain, Movement, and Total scores significantly improved over time. Asymptomatic patients had significantly more favorable CCS Pain scores compared to symptomatic patients [estimate (standard error): −1.84 (0.90), p = 0.04]; however, this significance was eliminated after adjusting for age [−1.37 (0.89), p = 0.13]. All SF-36 domains (physical functioning, role physical and emotional, energy and fatigue, well-being, social functioning, pain, and general health) were significantly improved over time, but there was no difference between asymptomatic and symptomatic patients. SOMS pain impact, pain quality, and fatigue were all significantly improved over time. Asymptomatic patients had significantly more favorable pain impact and pain quality scores compared to symptomatic patients, even after adjustment for age [estimate (se): −1.16 (0.49), p = 0.02; −1.03 (0.40), p = 0.01, respectively]. Table 5 presents results of mixed-effects models.
20% of patients who had TEP LIHR reported no pain at their preop clinic visit. Interestingly, nearly half of these reported some pain on the preop SOMS questionnaire, resulting in an average score of 1.3 on a 0–10 scale. The average pain score reported on SOMS by symptomatic individuals was significantly lower than the score reported in clinic. Figure 1 illustrates these discrepancies. Despite the preop SOMS pain scores being less divergent than the clinic scores, they remained significantly different over time until 6 months postoperatively (Fig. 2).
The asymptomatic cohort discontinued pain medication and returned to normal activities of daily living more quickly than preoperatively symptomatic individuals. This is consistent with significant difference between the cohorts as measured by SOMS pain impact and quality. The longitudinal trends for these SOMS domains are shown in Figs. 3 and 4. It is interesting that pain impact for the asymptomatic group increases from preop to 3 weeks postop, before decreasing to well below preop levels by 6 months. As noted above, a mixed-effect model of pain by CSS over time demonstrated significantly lower pain in the asymptomatic group until adjustment for age. The CCS questionnaire data were rearranged to reflect proportion of response by time type for Figs. 5 and 6. There were significantly more “No symptoms” responses in the asymptomatic group at each time point postoperatively, remaining consistent with postoperative outcomes and SOMS trends.
Discussion
In this review of 387 TEP LIHRs, patients in the asymptomatic cohort were older than their symptomatic counterparts. This may be explained by asymptomatic individuals being diagnosed later or taking longer to seek surgical consultation. Intraoperatively, this cohort also was found to have larger hernia defects and a lower proportion of indirect hernias. This may indicate that smaller hernia defects and indirect hernias are more likely to cause symptoms. A review of literature was unable to identify other studies describing a difference in preop symptoms between direct and indirect or small and large hernia defects. Inguinal defects in the setting of athletic pubalgia or ‘sportsman’s hernia’ are documented, although findings vary, with some citing equal distribution of direct and indirect hernias, while others predominantly describing small, bilateral indirect defects [22, 23].
A clear limitation of this study resulting from its retrospective nature was that 251 of the 638 TEP LIHRs in the database were missing necessary parameters. The majority of these exclusions were due lack of orally reported pain score on a 0–10 scale from preoperative clinic. There was a consideration to run the analysis using the preoperative SOMS VAS score, which would have included more patients. However, since this measure is not routinely used clinically, an analysis from the perspective of oral patient reporting in clinic was felt to be more clinically relevant, especially given the significant difference found between oral pain score and the SOMS VAS preoperatively.
Groin pain in the presence of an inguinal hernia can be a challenging entity. Causality is often unclear and strong correlations between surgical findings and symptoms have not been established. However, it has been demonstrated that pain preoperatively is predictive of pain postoperatively [24, 25]. Likewise, this analysis suggests that lack of pain preoperatively predicts less pain postoperatively. Outcomes for asymptomatic patients were equivalent to symptomatic patients, and it may be concluded that elective, totally extraperitoneal laparoscopic repair is safe for asymptomatic, appropriate surgical candidates.
References
Fitzgibbons RJ Jr, Forse RA (2015) Clinical practice. Groin hernias in adults. N Engl J Med. doi:10.1056/NEJMcp1404068
Malangoni MA, Gagliardi RJ (1004) Hernias. In: Townsend CM, Beauchamp RD, Evers BM, Mattox K (eds) Sabiston textbook of surgery, 17th edn. Saunders, New York, pp 1199–1218
Berger D (2016) Evidence-based hernia treatment. Dtsch Arztebl Int. doi:10.3238/arztebl.2016.0150
Devlin HB (1995) Trends in hernia surgery in the land of Astley Cooper. In: Soper NJ (ed) Problems in general surgery, vol 12. Lippincott-Raven, Philadelphia, pp 85–92
Cunningham J, Temple WJ, Mitchell P, Nixon JA, Preshaw RM, Hagen NA (1996) Cooperative hernia study: pain in the postrepair patient. Ann Surg 224(5):598
Berndsen FH, Petersson U, Arvidsson D, Leijonmarck CE, Rudberg C, Smedberg S, Montgomery A (2007) Discomfort five years after laparoscopic and Shouldice inguinal hernia repair: a randomised trial with 867 patients. A report from the SMIL study group. Hernia. doi:10.1007/s10029-007-0214-7
Fitzgibbons RJ (2005) Can we be sure polypropylene mesh causes infertility? Ann Surg. doi:10.1097/01.sla.0000157210.80440.b7
Bay-Nielsen M, Kehlet H, Strand L, Malmstrøm J, Andersen FH, Wara P, Juul P, Callesen T, Danish Hernia Database Collaboration (2001) Quality assessment of 26,304 herniorrhaphies in Denmark: a prospective nationwide study. Lancet. doi:10.1016/S0140-6736(01)06251-1
EU Hernia Trialists Collaboration (2000) Laparoscopic compared with open methods of groin hernia repair: systematic review of randomised controlled trials. Br J Surg. doi:10.1046/j.1365-2168.2000.01540.x
Memon MA, Cooper NJ, Memon B, Memon MI, Abrams KR (2003) Meta-analysis of randomised clinical trials comparing open and laparoscopic inguinal hernia repair. Br J Surg. doi:10.1002/bjs.4301
Grant AM, Scott NW, O’Dwyer PJ (2004) Pain and numbness after laparoscopic and open repair of a groin hernia: five year follow-up of a randomized trial. Br J Surg. doi:10.1002/bjs.4799
Jenkins J, O’Dwyer P (2008) Inguinal Hernias. BMJ. doi:10.1136/bmj.39450.428275.AD
Primatesta P, Goldacre MJ (1996) Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortality. Int J Epidemiol 25(4):835–839
Hwang MJ, Bhangu A, Webster CE, Bowley DM, Gannon MX, Karandikar SS (2014) Unintended consequences of policy change to watchful waiting for asymptomatic inguinal hernias. Ann R Coll Surg Engl. doi:10.1308/003588414X13946184902000
Fitzgibbons RJ Jr, Ramanan B, Arya S, Turner SA, Li X, Gibbs JO, Reda DJ (2013) Long-term results of a randomized controlled trial of a nonoperative strategy (watchful waiting) for men with minimally symptomatic inguinal hernias. Ann Surg. doi:10.1097/SLA.0b013e3182a19725
Mizrahi H, Parker MC (2012) Management of asymptomatic inguinal hernia: a systematic review of the evidence. Arch Surg. doi:10.1001/archsurg.2011.914
Fitzgibbons RJ, Giobbie-Hurder A, Gibbs JO, Dunlop DD, Reda DJ, McCarthy M Jr, Neumayer LA, Barkun JS, Hoehn JL, Murphy JT, Sarosi GA Jr, Syme WC, Thompson JS, Wang J, Jonasson O (2006) Watchful waiting vs repair of inguinal hernia in minimally symptomatic men: a randomised clinical trial. JAMA. doi:10.1001/jama.295.3.285
O’Dwyer PJ, Norrie J, Alani A, Walker A, Duffy F, Horgan P (2006) Observation or operation for patients with an asymptomatic inguinal hernia. Ann Surg. doi:10.1097/01.sla.0000217637.69699.ef
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30(6):473–483
Heniford BT, Walters AL, Lincourt AE, Novitsky YW, Hope WW, Kercher KW (2008) Comparison of generic versus specific quality-of-life scales for mesh hernia repairs. J Am Coll Surg. doi:10.1016/j.jamcollsurg.2007.11.025
Wikiel KJ, Eid GM (2015) Groin defects seen at extra-peritoneal laparoscopic dissection during surgical treatment of athletic pubalgia. Surg Endosc. doi:10.1007/s00464-014-3866-2
Kopelman D, Kaplan U, Hatoum OA, Abaya N, Karni D, Berber A, Sharon P, Peskin B (2016) The management of sportsman’s groin hernia in professional and amateur soccer players: a revised concept. Hernia. doi:10.1007/s10029-014-1322-9
Chowbey PK, Pithawala M, Khullar R, Sharma A, Soni V, Baijal M (2006) Complications in groin hernia surgery and the way out. J Minim Access Surg 2(3):174
Patel LY, Lapin B, Gitelis ME, Brown C, Linn JG, Haggerty S, Denham W, Butt Z, Barrera E, Joehl R, Carbray J, Hall T, Ujiki MB (2016) Long-term patterns and predictors of pain following laparoscopic inguinal hernia repair: a patient-centered analysis. Surg Endosc. doi:10.1007/s00464-016-5207-0
Pierides GA, Paajanen HE, Vironen JH (2016) Factors predicting chronic pain after open mesh based inguinal hernia repair: a prospective cohort study. Int J Surg. doi:10.1016/j.ijsu.2016.03.061
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Ujiki reports personal fees from GORE and Medtronic, outside the submitted work. Dr. Linn reports personal fees and Industry sponsored research support from Medtronic, outside the submitted work. Dr. Haggerty reports personal fees from GORE and Medtronic, outside the submitted work. Drs. Hedberg, Butt, Linn, Denham, Lapin, Mr. Hall, Gitelis, and Ms. Carbray have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Hedberg, H.M., Hall, T., Gitelis, M. et al. Quality of life after laparoscopic totally extraperitoneal repair of an asymptomatic inguinal hernia. Surg Endosc 32, 813–819 (2018). https://doi.org/10.1007/s00464-017-5748-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5748-x