Abstract
Background
Accurate tumor size measurement is critical for selecting proper candidates for endoscopic resection (ER) of early gastric cancer (EGC). However, size discrepancy between endoscopic size and pathologic size often occurs during ER for EGC.
Objective
The purposes of this study were to investigate the clinicopathological characteristics related to size discrepancy and the clinical implications of size discrepancies in terms of therapeutic outcomes.
Methods
Between April 2006 and June 2013, a total of 820 patients with 826 EGCs underwent ER. Enrolled lesions were categorized into the following three groups based on size discrepancy between endoscopic size and pathologic size: well-estimated (N = 308), underestimated (N = 215), or overestimated (N = 303) lesions. The well-estimated group was defined as lesions with a ratio of endoscopic size to pathologic size from 0.7 to 1.3.
Results
The overall median size discrepancy was 5.0 mm (interquartile range 2.0–9.0). Size, location, macroscopic type, primary tumor stage, and histology differed significantly between the three groups. Larger size [odds ratio (OR) 5.07, 95 % confidence interval (CI) 3.38–7.59, p < 0.001], flat/depressed type (OR 1.71, 95 % CI 1.15–2.55, p = 0.008), and undifferentiated histology (OR 2.24, 95 % CI 1.31–3.83, p = 0.003) were independent risk factors for endoscopic size underestimation in multivariate analysis. Smaller size (OR 10.95, 95 % CI 4.64–25.87, p < 0.001) was the only independent predictor for endoscopic overestimation of size. Significantly lower complete resection and curative resection rates were detected in the underestimated group compared with the well-estimated group, while the complete resection rate in the overestimated group tended to be higher than in the well-estimated group. There was no significant difference of curative resection rate between the overestimated and the well-estimated groups.
Conclusions
Larger size, flat/depressed type, and undifferentiated histology of EGC carry a significant risk for endoscopic underestimation of lesion size, which results in the lower rates of complete and curative resections for EGC. Further studies to reduce size discrepancy are warranted.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Early gastric cancer (EGC) is defined as gastric cancer that is confined to the mucosa or submucosa, irrespective of the presence of regional lymph node metastasis [1]. In eastern countries with a high prevalence of gastric cancer [2, 3], endoscopic resection (ER), including endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD), is a curative treatment option for some EGC cases [4, 5]. Recently, considerable data have also been reported from the western world as ER is gaining wide acceptance [6, 7]. The standard indications for ER of EGC include a size of 2 cm or smaller in diameter [8]. Furthermore, the expanded indications include a size of 3 cm or smaller if the lesion with differentiated histology shows ulcerative findings in mucosal cancer or SM1 depth of invasion without ulceration. In undifferentiated EGCs, the lesion must be a size of 2 cm or smaller and intramucosal, with no evidence of ulcer findings [8, 9]. Therefore, accurate tumor size measurement is critical for deciding proper candidates for ER of EGC.
Paradoxically, the size criteria for ER are mainly based on histopathologic findings of excised formalin-fixed specimens after surgery [9]. In contrast, endoscopists should estimate the lesion size based on endoscopic imaging. Thus, size discrepancy between endoscopic size and pathologic size often occurs during ER. Despite the importance of size measurement in ER for EGC, only a few studies so far have investigated the size discrepancy [10]. Therefore, the purposes of this study were to assess the clinicopathological characteristics related to size discrepancy in EGC and to evaluate the clinical implications of size discrepancies in terms of therapeutic outcomes.
Methods
Patients
This was a retrospective cohort study that analyzed the EGC database, which was maintained prospectively. Between April 2006 and June 2013 at a high-volume tertiary referral center, a total of 820 patients with 826 EGCs were enrolled in the present study. Enrolled patients underwent ER for EGC according to the standard and expanded indications [8]. Patients with lesions with piecemeal resection (N = 69), patients with lesions from remnant stomach (N = 2), and patients with Barrett-associated cancers (N = 2) were excluded.
Enrolled lesions were categorized into the following three groups based on size discrepancy between endoscopic size and pathologic size: well-estimated (N = 308), underestimated (N = 215), or overestimated (N = 303) lesions. The well-estimated group was defined as lesions with a ratio of endoscopic size to pathologic size from 0.7 to 1.3. The underestimated and overestimated groups were defined as lesions with ratios of endoscopic size to pathologic size less than 0.7 and more than 1.3, respectively.
Demographic data for the enrolled patients and clinicopathologic characteristics and outcomes of the three groups were analyzed. Written informed consents explaining possible procedure-related risks, complications, and alternative surgical options were obtained from all patients before ER. This study was approved by the Institutional Review Board of Yonsei University College of Medicine, Korea.
Size measurement
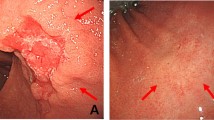
Size was measured prospectively by endoscopy and pathology. Endoscopic size was estimated in the longest diameter of lesion, by five gastroenterology attending physicians using standard upper gastrointestinal endoscopes (GIF Q260 and H260, Olympus, Japan) as follows. First was the visual estimation method, whereby the tip of the endoscope was withdrawn about 3–4 cm from the EGC and the largest diameter was visually estimated. Second was the open biopsy forceps method, whereby a biopsy forceps (FB-21K-1, Olympus, Japan), with a diameter of 6 mm when opened fully, was used. The forceps was withdrawn in the open position toward the endoscope tip as far as possible until both cups were fully visualized. The open forceps was then advanced until it was aligned against the largest diameter of the lesion, with the tip of the endoscope still placed at approximately 3–4 cm from the lesion [11]. Chromoendoscopy with indigo carmine (0.2 % solution) was routinely performed to define the horizontal extent of tumor infiltration. Magnifying endoscopy with narrow-band imaging (ME-NBI) was carried out in selected cases for delineation of ill-defined margins by chromoendoscopy [12, 13].
Pathologic size was based on the longest diameter of the lesion in the ER specimen. After resection, ER specimens were only minimally stretched to avoid overextension, pinned on a styrofoam board, and immediately immersed in formalin fixative for 4 h. Fixed specimens were sectioned serially at 2-mm intervals, and entirely embedded in paraffin. Size was measured using the map template, which was considered the reference standard.
Clinicopathologic characteristics
The size was based on pathologic size, with classification of no larger than 20 mm and larger than 20 mm. The location of lesions was divided into three sections by categorization of the longitudinal axis of the stomach (upper third containing the fundus, cardia, and upper body; mid-third containing the mid-body, lower body, and angle; and lower third containing the antrum and pylorus) and four sections by categorization of the cross-sectional circumference of the stomach (anterior wall, posterior wall, greater curvature, and lesser curvature). Macroscopic type was classified according to the macroscopic classification of EGC by the Japanese Gastric Cancer Association [14]. Additionally, the macroscopic types were grouped as elevated or flat/depressed types [10]. Submucosal invasion was evaluated by endoscopic ultrasound (EUS) in a select group of patients (476/820, 58.0 %) and was confirmed by histologic diagnosis. Histologic diagnoses and grade of differentiation were performed based on the World Health Organization classification of gastrointestinal tumors [15, 16]. The histologic diagnoses were classified into two categories based on the Japanese classification of gastric carcinoma, as either differentiated or undifferentiated histologic type [14].
Endoscopic resection
The ER methods included consisted of EMR (including the injection-and-cut technique, EMR with the cap technique, and EMR by a snare after circumferential precutting with a knife) and ESD. The details of ER were described previously [17].
Therapeutic outcomes
The therapeutic outcomes of ER were classified as complete resection and curative resection. Complete resection was defined as en bloc resection with no cancer cell exposure to any cut end [18]. Incomplete resection was defined as resection that did not meet the complete resection criteria. Different definitions of curative resection were applied for differentiated and undifferentiated histologic type cancers, respectively, because they have different profiles regarding the risk of metastasis [9]. Curative resection in differentiated EGC was defined as complete resection with no lymphovascular invasion and no submucosal invasion deeper than 500 μm from the muscularis mucosa [19]. Curative resection in undifferentiated EGC was defined as complete resection with intramucosal invasion, no lymphovascular invasion, no ulceration, and no larger than 2 cm in diameter [20]. Non-curative resections were defined as resections that did not meet the respective curative resection criteria.
Statistical analysis
The χ 2 test or Fisher’s exact test was used to test categorical data. The Student’s t test or Wilcoxon signed rank test or one-way analysis of variance was used for noncategorical data. Multinomial logistic regression analysis was performed to assess the relationship of clinicopathological characteristics and size discrepancy towards underestimation and overestimation from well-estimation, respectively. Characteristics with a univariate significance of p < 0.05 were candidates for multivariate analysis. p < 0.05 was considered statistically significant. Statistical analysis was performed using the SAS program (version 9.2, SAS Institute, Cary, NC, USA).
Results
Size discrepancy and baseline characteristics of patients
A total of 820 patients with 826 EGCs (598 men and 222 women; mean age 65.3 ± 10.6 years) underwent ER. Specifically, ten EMRs and 816 ESDs were performed. The overall median sizes of lesions were 12.0 mm [interquartile range (IQR) 10.0–15.0] and 12.0 mm (IQR 7.0–20.0) by endoscopy and pathology, respectively. This was not significantly different (p = 0.369). The overall median absolute size discrepancy between endoscopic size and pathologic size was 5.0 mm (IQR 2.0–9.0), and the overall median ratio of endoscopic size to pathologic size was 1.0 (IQR 1.0–2.0). The median ratios of endoscopic size to pathologic size in the well-estimated, underestimated, and overestimated groups were 1.0 (IQR 0.8–1.1), 0.50 (IQR 0.4–0.6), and 1.9 (IQR 1.5–2.7), respectively. The median absolute size discrepancies as well as median ratios of endoscopic size to pathologic size among five endoscopists were not statistically different. The overall intraclass correlation coefficient (ICC) between endoscopic size and pathologic size was 0.61 [95 % confidence interval (CI) 0.54–0.67]. The ICCs between endoscopic size and pathologic size among involved endoscopists were not significantly different.
The baseline characteristics of enrolled patients are shown in Table 1. No significant differences in baseline characteristics, including age, sex, alcohol, smoking, comorbidities, use of antiplatelets, use of anticoagulation, and Helicobacter pylori infection were detected between patients with endoscopically well-estimated, underestimated, and overestimated lesions.
Clinicopathological characteristics related to size discrepancy
The comparison of clinicopathological characteristics between the three groups is listed in Table 2. Size (p < 0.001), location (p = 0.001), macroscopic type (p = 0.020), primary tumor (pT) stage (p = 0.001), and histology (p = 0.006) were significantly different between the three groups. T stage on EUS tended to differ between the groups (p = 0.207). In particular, larger size (p < 0.001), flat/depressed type (p = 0.016), and undifferentiated histology (p = 0.002) were significant characteristics of the underestimated group compared with the well-estimated group. The underestimated group tended to exhibit mid-third location (p = 0.082), submucosal invasion on EUS (p = 0.124), and submucosal invasion determined by histopathology (p = 0.139) compared with the well-estimated group. In addition, smaller size (p < 0.001) and intramucosal invasion determined by histopathology (p = 0.024) were significant features of the overestimated group compared with the well-estimated group. The overestimated group tended to locate in the lower-third of the stomach (p = 0.076).
In multivariate analysis, larger size [odds ratio (OR) 5.07, 95 % CI 3.38–7.59, p < 0.001], flat/depressed macroscopic type (OR 1.71, 95 % CI 1.15–2.55, p = 0.008), and undifferentiated histology (OR 2.24, 95 % CI 1.31–3.83, p = 0.003) were independent risk factors for endoscopic size underestimation. Submucosal invasion determined by histopathology showed a tendency toward being associated with endoscopic underestimation of size (OR 1.35, 95 % CI 0.86–2.14, p = 0.194). In contrast, smaller size (OR 10.95, 95 % CI 4.64–25.87, p < 0.001) was the only significant predictive factor for endoscopic size overestimation. Location in the lower third of the stomach (OR 1.90, 95 % CI 0.94–3.82, p = 0.073) and intramucosal invasion determined by histopathology (OR 1.52, 95 % CI 0.97–2.38, p = 0.070) revealed a tendency toward being related to endoscopic overestimation of lesion size (Table 3).
Characteristics of the endoscopic procedure, including procedure time during ER and complications of ER, were assessed. The overall median ER time was 44.0 min (IQR 30.0–65.0). The overall complication rates for bleeding and perforation were 4.5 % (37/826) and 2.9 % (24/826), respectively. There were no significant differences between the three groups in terms of the ER procedure time and bleeding and perforation rates.
Therapeutic outcomes according to size discrepancy
The therapeutic outcomes of three groups are summarized in Table 4. The overall complete resection and curative resection rates were 90.3 % (746/826) and 80.8 % (667/826), respectively. Complete resection and curative resection were not statistically different among five endoscopists involved. Complete resection (p < 0.001) and curative resection (p < 0.001) were significantly different among the three groups. Significantly lower rates of complete resection (p = 0.003) and curative resection (p < 0.001) were detected in the underestimated group compared with the well-estimated group, whereas the complete resection rate in the overestimated group tended to be higher than in the well-estimated group (p = 0.078). There was no significant difference of curative resection rate between the overestimated and the well-estimated groups.
Positive cancer invasion at the lateral cut end (p < 0.001) and lymphovascular invasion (p = 0.037) were also statistically different among the three groups. The groups tended to have the different rate of positive cancer invasion at the vertical cut end (p = 0.083). The underestimated group showed the significantly higher rate of positive cancer invasion at the lateral cut end (p < 0.001) and tended to exhibit the higher rate of lymphovascular invasion (p = 0.080) compared with the well-estimated group. There was no statistical difference of positive cancer invasion at the vertical cut end between the underestimated and the well-estimated groups. The overestimated group revealed the significantly lower rate of positive cancer invasion at the vertical cut end (p = 0.042). There were no statistical differences of positive cancer invasion at the lateral cut end and lymphovascular invasion between the overestimated and the well-estimated groups.
Discussion
This study focused on clinicopathological characteristics and therapeutic outcomes of size discrepancy between endoscopic size and pathologic size in EGCs treated by ER.
Size discrepancy between endoscopic estimation and pathologic measurement is inevitable during ER for EGC since endoscopists can only estimate approximate tumor size on the basis of endoscopic imaging. Along these lines, only a few retrospective studies have so far been performed on size discrepancy in EGC, and these had controversial results [10, 21, 22]. A previous study showed that the mean size discrepancy in EGCs, comprising 396 differentiated and 60 undifferentiated lesions, was 7.3 ± 9.1 mm [22]. Moreover, the mean size discrepancies in other studies were 18.4 ± 22.0 mm in extremely well-differentiated adenocarcinomas and 5.8 ± 7.5 mm in EGCs consisting of 834 differentiated and 21 undifferentiated lesions, respectively [21]. These findings were comparable to the mean size discrepancy in our study revealing 6.8 ± 9.5 mm. In contrast, an earlier study showed that the mean size discrepancy of lesions with 438 differentiated and 70 undifferentiated histologic types was 1.7 mm (95 % CI 1.4–2.0) and an absolute difference less than 4 mm was found for 80 % of enrolled cases [10]. However, the retrospective approach using the endoscopic visual estimation method on still images performed by only trained endoscopists is a critical limitation to application of the results in a practical setting. In the current study, an absolute difference of less than 4 mm was found for 47.1 % (389/826) of enrolled lesions. Moreover, the strength of overall ICC between endoscopic size and pathologic size was moderate. Although the heterogeneity in composition of endoscopists as well as in endoscopic estimation methods may affect our results [11, 23], the limited success of endoscopic size estimation warranted further well-designed, multicenter, prospective studies to reduce the size discrepancy. In clinical grounds, to improve the size estimation before ER, other endoscopic methods including EUS and ME-NBI should be taken into account. EUS has the potential to provide a more objective lesion size measurement. The marginal demarcations of tumors could be better recognized in ME-NBI [12, 13, 24]. Although the estimated size via radial scanning echoendoscopes may not represent the maximal diameter of the entire lesion, particularly with the longest size in the longitudinal axis, we recommend the combined evaluation of the lesion size to compensate for the limited accuracy of endoscopic estimation. With regards to a standard method in measuring lesion sizes, there is no consensus for the standard method to determine the size of EGC before ER. Therefore, we should investigate the most precise method to estimate lesion sizes before ER and standardize the method accompanied by the development of a more appropriate technique in handling the ER specimen to avoid inconsistency in pathologic measurements. Additionally, the clinicopathologic features predictive of endoscopic size underestimation should be investigated as a potentially important factor of incomplete ER of EGC.
In this study, larger size, flat/depressed type, and undifferentiated histology were independent risk factors for endoscopic size underestimation. Smaller size was the sole independent predictor for endoscopic overestimation of size. These findings were consistent with earlier studies showing that size discrepancy was proportional to tumor size and increased for undifferentiated histology [10, 22]. Nonetheless, size discrepancies towards underestimation versus overestimation were not differentiated in these studies. Furthermore, other earlier studies revealed that larger size, submucosal invasion, mid-third location, and an ill-defined margin of tumor infiltration were features of undifferentiated EGC [12, 22, 25–28]. Thus, the association of larger size with endoscopically underestimated tumor may be due to characteristics arising from the higher undifferentiated histology in the underestimated group. In addition, an ill-defined tumor margin and an intramucosal lateral spreading pattern of undifferentiated EGCs may contribute to size underestimation of EGC [12, 27].
To date, the clinical implications of size discrepancy with reference to therapeutic outcomes have not been evaluated. The underestimated group showed therapeutic outcomes of 82.3 % for complete resection and 67.9 % for curative resection, which are comparable to the reported therapeutic outcomes of ER for undifferentiated EGC of 55.0–90.7 % for complete resection rate and 31.1–82.5 % for curative resection rate [17, 20, 22, 25, 29–31], and much lower than the outcomes of ER for differentiated EGC of 88.9–93.4 % for complete resection rate and 91.3–94.7 % for curative resection rate [19, 32–36]. In addition, the outcomes of the underestimated group were significantly lower than those of the well-estimated lesions. We attributed this finding to the higher lateral margin positivity due to size underestimation as well as the tendency of more frequent lymphovascular invasion accompanied by larger tumor size in the underestimated group [37]. Moreover, increased histologic diversity with higher proportions of undifferentiated types in the underestimated group can result in trend towards deeper invasion [38, 39]. In contrast, there was no definite benefit to curative resection resulting from endoscopic overestimation of size in our study, though the overestimated group tended to have improved outcomes in complete resection compared with the well-estimated group. Therefore, we should avoid underestimating lesion size, as it leads to dissimilar therapeutic outcomes, and should instead pay attention to the possibility of underestimation if the lesion shows larger size, flat/depressed type, and undifferentiated histology. In contrast to deeper invasion, lymphovascular invasion, or undifferentiated histology, the precise demarcation of tumor margin relatively depends on endoscopists. Nonetheless, endoscopists often encounter some lesions revealing an ill-defined margin on chromoendoscopy as well as conventional white light endoscopy. In these cases, ME-NBI can be useful to define the ill-defined horizontal extent of tumor infiltration [12, 13, 24]. Circumferential biopsies of the lesion may be another supportive method to exclude the equivocal lateral tumor extension. Moreover, the real-time in vivo histologic evaluation using confocal laser endomicroscopy might be helpful to demarcate the tumor margin [40].
Our study had some limitations. First, this was a retrospective study in a single center. As this is the first study investigating the clinical implications of size discrepancy between endoscopic size and pathologic size in ER for EGC, the earlier data for cut-off value of well-estimated lesions versus underestimated or overestimated lesions are lacking. Although a recent study on the size variation of colon polyps between endoscopic estimate and pathologic measurement considered a variation of more than 33 % to be significant, the relatively arbitrary definitions of the three groups are a possible limitation. Additionally, endoscopic size estimation supported by ME-NBI was not differentiated. Because EGC demarcations could be better recognized in ME-NBI [12, 13, 24], the heterogeneity in endoscopic visualization is also a limitation. Lastly, EUS was evaluated in selected patients only. Thus, selection bias may have affected the study results.
Despite these limitations, the present study has some merits. This is the first comparative study composed of EGCs with well-estimated, underestimated, and overestimated endoscopic sizes. Moreover, this study suggests several clinicopathologic characteristics predictive of endoscopic size underestimation resulting in lower complete and curative resection rates of ER.
In conclusion, larger size, flat/depressed type, and undifferentiated histology of EGC carry a high risk for endoscopic underestimation of size, whereas a smaller size carries a significant risk for endoscopic overestimation of size. EGC with endoscopically underestimated size alters complete and curative resection rates, while there is no definite benefit to curative resection resulting from the endoscopic overestimation of size. Other supportive imaging modalities including EUS and ME-NBI should be considered to improve size measurement. Further multicenter, prospective studies should be conducted for the standardization of size estimation methods before ER in addition to reducing size discrepancies.
Abbreviations
- EGC:
-
Early gastric cancer
- ER:
-
Endoscopic resection
- EMR:
-
Endoscopic mucosal resection
- ESD:
-
Endoscopic submucosal dissection
- ME-NBI:
-
Magnifying endoscopy with narrow-band imaging
- EUS:
-
Endoscopic ultrasound
- IQR:
-
Interquartile range
References
Murakami T (1971) Pathomorphological diagnosis. Definition and gross classification of early gastric cancer. Gann Monogr Cancer Res 11:53–55
Ahn YO, Park BJ, Yoo KY, Kim NK, Heo DS, Lee JK, Ahn HS, Kang DH, Kim H, Lee MS et al (1991) Incidence estimation of stomach cancer among Koreans. J Korean Med Sci 6(1):7–14
Nakamura K, Ueyama T, Yao T, Xuan ZX, Ambe K, Adachi Y, Yakeishi Y, Matsukuma A, Enjoji M (1992) Pathology and prognosis of gastric carcinoma. Findings in 10,000 patients who underwent primary gastrectomy. Cancer 70(5):1030–1037
Tada M, Murakami A, Karita M, Yanai H, Okita K (1993) Endoscopic resection of early gastric cancer. Endoscopy 25(7):445–450
Gotoda T, Kondo H, Ono H, Saito Y, Yamaguchi H, Saito D, Yokota T (1999) A new endoscopic mucosal resection procedure using an insulation-tipped electrosurgical knife for rectal flat lesions: report of two cases. Gastrointest Endosc 50(4):560–563
Probst A, Pommer B, Golger D, Anthuber M, Arnholdt H, Messmann H (2010) Endoscopic submucosal dissection in gastric neoplasia: experience from a European center. Endoscopy 42(12):1037–1044
Farhat S, Chaussade S, Ponchon T, Coumaros D, Charachon A, Barrioz T, Koch S, Houcke P, Cellier C, Heresbach D, Lepilliez V, Napoleon B, Bauret P, Coron E, Le Rhun M, Bichard P, Vaillant E, Calazel A, Bensoussan E, Bellon S, Mangialavori L, Robin F, Prat F (2011) Endoscopic submucosal dissection in a European setting. A multi-institutional report of a technique in development. Endoscopy 43(8):664–670
Japanese Gastric Cancer Association (2011) Japanese gastric cancer treatment guidelines 2010 (version 3). Gastric Cancer 14(2):113–123
Gotoda T, Yanagisawa A, Sasako M, Ono H, Nakanishi Y, Shimoda T, Kato Y (2000) Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer 3(4):219–225
Choi J, Kim SG, Im JP, Kim JS, Jung HC (2013) Endoscopic estimation of tumor size in early gastric cancer. Dig Dis Sci 58(8):2329–2336
Gopalswamy N, Shenoy VN, Choudhry U, Markert RJ, Peace N, Bhutani MS, Barde CJ (1997) Is in vivo measurement of size of polyps during colonoscopy accurate? Gastrointest Endosc 46(6):497–502
Nagahama T, Yao K, Maki S, Yasaka M, Takaki Y, Matsui T, Tanabe H, Iwashita A, Ota A (2011) Usefulness of magnifying endoscopy with narrow-band imaging for determining the horizontal extent of early gastric cancer when there is an unclear margin by chromoendoscopy (with video). Gastrointest Endosc 74(6):1259–1267
Kadowaki S, Tanaka K, Toyoda H, Kosaka R, Imoto I, Hamada Y, Katsurahara M, Inoue H, Aoki M, Noda T, Yamada T, Takei Y, Katayama N (2009) Ease of early gastric cancer demarcation recognition: a comparison of four magnifying endoscopy methods. J Gastroenterol Hepatol 24(10):1625–1630
Japanese Gastric Cancer Association (2011) Japanese classification of gastric carcinoma, 3rd English edn. Gastric Cancer 14(2):101–112
Hamilton SR, Aaltonen LA (2000) Pathology and genetics of tumours of the digestive system. In: World Health Organization classification of tumours. International Agency for Research on Cancer, Lyon
Kim WH, Park CK, Kim YB (2005) A standardized pathology report for gastric cancer. Korean J Pathol 39:106–113
Kim JH, Lee YC, Kim H, Song KH, Lee SK, Cheon JH, Kim H, Hyung WJ, Noh SH, Kim CB, Chung JB (2009) Endoscopic resection for undifferentiated early gastric cancer. Gastrointest Endosc 69(4):e1–e9
Park YM, Cho E, Kang HY, Kim JM (2011) The effectiveness and safety of endoscopic submucosal dissection compared with endoscopic mucosal resection for early gastric cancer: a systematic review and metaanalysis. Surg Endosc 25(8):2666–2677
Isomoto H, Shikuwa S, Yamaguchi N, Fukuda E, Ikeda K, Nishiyama H, Ohnita K, Mizuta Y, Shiozawa J, Kohno S (2009) Endoscopic submucosal dissection for early gastric cancer: a large-scale feasibility study. Gut 58(3):331–336
Kim YY, Jeon SW, Kim J, Park JC, Cho KB, Park KS, Kim E, Chung YJ, Kwon JG, Jung JT, Kim EY, Kim KO, Jang B, Lee SH, Yang CH (2013) Endoscopic submucosal dissection for early gastric cancer with undifferentiated histology: could we extend the criteria beyond? Surg Endosc 27(12):4656–4662
Kang KJ, Kim KM, Kim JJ, Rhee PL, Lee JH, Min BH, Rhee JC, Kushima R, Lauwers GY (2012) Gastric extremely well-differentiated intestinal-type adenocarcinoma: a challenging lesion to achieve complete endoscopic resection. Endoscopy 44(10):949–952
Kang HY, Kim SG, Kim JS, Jung HC, Song IS (2010) Clinical outcomes of endoscopic submucosal dissection for undifferentiated early gastric cancer. Surg Endosc 24(3):509–516
Eichenseer PJ, Dhanekula R, Jakate S, Mobarhan S, Melson JE (2013) Endoscopic mis-sizing of polyps changes colorectal cancer surveillance recommendations. Dis Colon Rectum 56(3):315–321
Kiyotoki S, Nishikawa J, Satake M, Fukagawa Y, Shirai Y, Hamabe K, Saito M, Okamoto T, Sakaida I (2010) Usefulness of magnifying endoscopy with narrow-band imaging for determining gastric tumor margin. J Gastroenterol Hepatol 25(10):1636–1641
Yamamoto Y, Fujisaki J, Hirasawa T, Ishiyama A, Yoshimoto K, Ueki N, Chino A, Tsuchida T, Hoshino E, Hiki N, Fukunaga T, Sano T, Yamaguchi T, Takahashi H, Miyata S, Yamamoto N, Kato Y, Igarashi M (2010) Therapeutic outcomes of endoscopic submucosal dissection of undifferentiated-type intramucosal gastric cancer without ulceration and preoperatively diagnosed as 20 millimetres or less in diameter. Dig Endosc 22(2):112–118
Huh CW, da Jung H, Kim JH, Lee YC, Kim H, Kim H, Yoon SO, Youn YH, Park H, Lee SI, Choi SH, Cheong JH, Noh SH (2013) Signet ring cell mixed histology may show more aggressive behavior than other histologies in early gastric cancer. J Surg Oncol 107(2):124–129
Sawada S, Fujisaki J, Yamamoto N, Kato Y, Ishiyama A, Ueki N, Hirasawa T, Yamamoto Y, Tsuchida T, Tatewaki M, Hoshino E, Igarashi M, Takahashi H, Fujita R (2010) Expansion of indications for endoscopic treatment of undifferentiated mucosal gastric cancer: analysis of intramucosal spread in resected specimens. Dig Dis Sci 55(5):1376–1380
Zambelli A (2010) Can virtual chromoendoscopy measure up to histology in early gastric cancer? Dig Liver Dis 42(10):677–678
Abe S, Oda I, Suzuki H, Nonaka S, Yoshinaga S, Odagaki T, Taniguchi H, Kushima R, Saito Y (2013) Short- and long-term outcomes of endoscopic submucosal dissection for undifferentiated early gastric cancer. Endoscopy 45(9):703–707
Park J, Choi KD, Kim MY, Lee JH, Song HJ, Lee GH, Jung HY, Kim JH (2012) Is endoscopic resection an acceptable treatment for undifferentiated EGC? Hepatogastroenterology 59(114):607–611
Okada K, Fujisaki J, Yoshida T, Ishikawa H, Suganuma T, Kasuga A, Omae M, Kubota M, Ishiyama A, Hirasawa T, Chino A, Inamori M, Yamamoto Y, Yamamoto N, Tsuchida T, Tamegai Y, Nakajima A, Hoshino E, Igarashi M (2012) Long-term outcomes of endoscopic submucosal dissection for undifferentiated-type early gastric cancer. Endoscopy 44(2):122–127
Goto O, Fujishiro M, Kodashima S, Ono S, Omata M (2009) Outcomes of endoscopic submucosal dissection for early gastric cancer with special reference to validation for curability criteria. Endoscopy 41(2):118–122
Lee H, Yun WK, Min BH, Lee JH, Rhee PL, Kim KM, Rhee JC, Kim JJ (2011) A feasibility study on the expanded indication for endoscopic submucosal dissection of early gastric cancer. Surg Endosc 25(6):1985–1993
Ahn JY, Jung HY, Choi KD, Choi JY, Kim MY, Lee JH, Choi KS, Kim do H, Song HJ, Lee GH, Kim JH, Park YS (2011) Endoscopic and oncologic outcomes after endoscopic resection for early gastric cancer: 1370 cases of absolute and extended indications. Gastrointest Endosc 74(3):485-493
Yamaguchi N, Isomoto H, Fukuda E, Ikeda K, Nishiyama H, Akiyama M, Ozawa E, Ohnita K, Hayashi T, Nakao K, Kohno S, Shikuwa S (2009) Clinical outcomes of endoscopic submucosal dissection for early gastric cancer by indication criteria. Digestion 80(3):173–181
Min BH, Lee JH, Kim JJ, Shim SG, Chang DK, Kim YH, Rhee PL, Kim KM, Park CK, Rhee JC (2009) Clinical outcomes of endoscopic submucosal dissection (ESD) for treating early gastric cancer: comparison with endoscopic mucosal resection after circumferential precutting (EMR-P). Dig Liver Dis 41(3):201–209
Sako A, Kitayama J, Ishikawa M, Yamashita H, Nagawa H (2006) Impact of immunohistochemically identified lymphatic invasion on nodal metastasis in early gastric cancer. Gastric Cancer 9(4):295–302
Luinetti O, Fiocca R, Villani L, Alberizzi P, Ranzani GN, Solcia E (1998) Genetic pattern, histological structure, and cellular phenotype in early and advanced gastric cancers: evidence for structure-related genetic subsets and for loss of glandular structure during progression of some tumors. Hum Pathol 29(7):702–709
Zheng HC, Li XH, Hara T, Masuda S, Yang XH, Guan YF, Takano Y (2008) Mixed-type gastric carcinomas exhibit more aggressive features and indicate the histogenesis of carcinomas. Virchows Arch 452(5):525–534
Bok GH, Jeon SR, Cho JY, Cho JH, Lee WC, Jin SY, Choi IH, Kim HG, Lee TH, Park EJ (2013) The accuracy of probe-based confocal endomicroscopy versus conventional endoscopic biopsies for the diagnosis of superficial gastric neoplasia (with videos). Gastrointest Endosc 77(6):899–908
Conflicts of interest
There are no financial or other conflicts of interest to disclose.
Disclosure
The authors declare there are no financial relationships relevant to this publication.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shim, C.N., Song, M.K., Kang, D.R. et al. Size discrepancy between endoscopic size and pathologic size is not negligible in endoscopic resection for early gastric cancer. Surg Endosc 28, 2199–2207 (2014). https://doi.org/10.1007/s00464-014-3453-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3453-6