Abstract
Purpose
The aim of this study was to pathologically investigate the developmental pattern of undifferentiated mucosal gastric cancer and to determine safe surgical margins for curative resection by endoscopic resection.
Results
Intramucosal cancer spread, or the width of the proliferative zone, was pathologically investigated in 47 cases of undifferentiated mucosal gastric cancer of size 20 mm or smaller without ulceration (scars). The 47 cases comprised 40 IIc and 7 IIb cases. The IIc cases consisted of 5 (12.5%) of intermediate-layer type (cancer localized at the intermediate layer of the mucosa), 31 (77.5%) of superficial type, and 4 of whole-layer type (10%). The IIb cases consisted of six of intermediate-layer type (85.7%) and one of superficial type (14.3%). The width of the proliferative zone in the 40 IIc cases ranged from 0 to 2,390 μm (average 605.5 μm). There was no significant correlation between width of proliferative zone and background mucosa. With regard to lesion size, average width was 243.6 μm in cases with longest diameter ≤5 mm, while it was significantly larger (617.1 μm) in cases with diameter >5 mm.
Conclusions
In endoscopic treatment of undifferentiated mucosal gastric cancer of size 20 mm or smaller without ulceration (scars), the lateral safety margin should be 3 mm or more.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Indications for endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) of early gastric cancer were proposed in guidelines by the Japanese Gastric Cancer Association [1], and treatment has been given according to these guidelines as a defined standard nationwide in Japan. Expansion of the indications for EMR/ESD to submucosal (SM) cancer and undifferentiated cancer under certain circumstances has been discussed. In consideration of the absence of lymphatic metastasis, indications for endoscopic treatment have been expanded to SM cancer with invasion depth ≤500 μm and undifferentiated mucosal cancer of longest diameter ≤20 mm without ulceration, because such cancers have been postulated to have no metastasis.
However, since undifferentiated cancer spreads laterally along the proliferative zone in a developmental pattern, macroscopic diagnosis of cancer expansion is not always consistent with pathological diagnosis, and the presence of skip lesions has also been demonstrated [2–5], which remains a problem in judging curative resection.
Aims
The aim of this study is to pathologically investigate the developmental pattern of undifferentiated mucosal gastric cancer and to determine safe surgical margins for curative resection by endoscopic resection (EMR/ESD).
Subjects and Methods
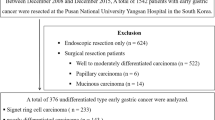
The samples comprised 18 gastric cancers resected surgically with sufficient lymphadenectomy between April 2001 and March 2006 and 29 gastric cancers resected by EMR/ESD between October 2000 and May 2006 at the Japanese Foundation for Cancer Institute Hospital, Tokyo, Japan. All of them were solitary undifferentiated mucosal cancer 20 mm or smaller in size without ulcer scars. Of the patients, 21 were male and 26 were female. Macroscopic type was diagnosed according to the Japanese Classification of Gastric Carcinoma. Cancers identifiable only by color changes were diagnosed as IIb, while those with a distinct depression macroscopically were diagnosed as IIc (Fig. 1).
The surgical margins were cancer-free in all cases, and no lymphatic or vascular invasion was recognized. Growth of mucosal cancer was observed in hematoxylin and eosin (HE)- and periodic acid Schiff (PAS)-stained specimens, and the absence of ulcer scars was confirmed. The surgically resected tissue was sliced at 5 mm width and the EMR/ESD tissue was sliced at 2 mm width in all cases for mapping of cancer development. Legion size was measured with a scale on the mapping image and subjected to analysis.
The patterns of cancer intramucosal spread were categorized as in Fig. 2 according to the classification by Yao et al. [6, 7]. In particular, cancer was not exposed at the mucosal surface of the resected specimens in 40 IIc cases, and the width of spread in the intermediate layer of the mucosa or along the proliferative zone was measured with a microscale (Fig. 3). When cancer spread bidirectionally along the proliferative zone from the depression, the maximum diameter was adopted for analysis. The width of the proliferative zone was compared with the background gastric mucosa and size of the lesion.
Results
-
(1)
The longer diameter ranged from 2 to 20 mm with an average of 10.85 mm. In terms of macroscopic appearance of the lesion, there were seven IIb cases, of which six were of intermediate-layer type (85.7%) and one was of superficial type (14.3%). There was no whole-layer type case. On the other hand, there were 40 IIc cases that consisted of 5 of intermediate-layer type (12.5%), 31 of superficial type (77.5%), and 4 of whole-layer type (10.0%; Table 1).
Table 1 Size and macroscopic appearance of undifferentiated early gastric cancer -
(2)
In the 40 IIc cases, the width of intramucosal cancer spread was examined. The width of the proliferative zone ranged from 0 to 2,390 μm with an average of 605.5 μm. The width was between 0 and 1,000 μm in 28 cases (70%), between 1,001 and 2,000 μm in 11 cases (27.5%), and between 2,001 and 3,000 μm in 1 case (2.5%; Table 2).
Table 2 Width of proliferative zone (0-IIc type) -
(3)
The width of the proliferative zone was compared with the background gastric mucosa in IIc cases. Cancer was located at the fundic region in 26 cases, for which the average width of the proliferative zone was 572.3 μm. Seven cases were localized at the pyloric gland area, for which the average width of the proliferative zone was 817.1 μm. Four cases were localized at the intermediate zone, for which the average width of the proliferative zone was 632 μm. Three cases were located at the mucosa with marked atrophy and/or intestinal metaplasia, for which the average width of the proliferative zone was 363.7 μm (Table 3). There was no significant difference in width of the proliferative zone among different locations, but it tended to be longer in the pyloric gland area and intermediate zone.
Table 3 Characteristics of background mucosa and average width of proliferative zone (0-IIc type) -
(4)
The minimal cancer size was defined as <5 mm. So, the width of the proliferative zone was compared at size more or less than 5 mm. There were ten cases with lesion size 5 mm or smaller, for which the average width of the proliferative zone was 276 μm. There were 31 cases with lesion size larger than 5 mm, for which the average width of the proliferative zone was 775 μm, which was significantly longer than that of the smaller cancers. The width of the proliferative zone tended to be greater in larger cancers (Table 4).
Table 4 Width of the proliferative zone (compared at size) -
(5)
Case: A 71-year-old male. A depressed lesion at the greater curvature of the lower gastric body was found by screening endoscopy. Biopsy revealed group V. ESD was carried out on February 10, 2006. The cancer was resected in one piece, and the lesion size was 8 mm (Fig. 4). Pathology was: sig, depth m, ly0, v0, l-ce(-), v-ce(-). Pathology revealed that the background mucosa consisted of fundic glands, and the cancer exhibited whole-layer type. The width of the proliferative zone was 1,900 μm (Fig. 5).
Discussion
Guidelines for treatment of gastric cancer were proposed by the Japanese Gastric Cancer Association to standardize treatment of gastric cancer according to definite criteria nationwide [1]. In the second edition, guidelines for piecemeal resection were documented, and expanded indications have been suggested based on size and in cases of SM and undifferentiated mucosal cancer. However, when the expanded indications are evaluated in cases of SM and undifferentiated cancer, it is apparent that indications, methods, and criteria on the surgical margin for curative resection have not been clearly defined.
Multicenter trials showed that the risk of lymphatic metastasis in undifferentiated mucosal gastric cancers 20 mm or smaller without ulceration was markedly low [1, 8, 9]. It has been reported earlier that the size of undifferentiated gastric cancer suitable for EMR was 5 mm or smaller [10], or 10 mm or smaller [11]. However, since such cancers develop laterally along the proliferative zone, it has been said that it is difficult to determine the cancer margin, and that endoscopic treatment is unlikely to be indicated due to the presence of skip lesions [2–5].
For these reasons, there is no distinct description in the guidelines regarding the distance from the cancer margin for cut-end negative and curative resection. In this study, we examined the developmental patterns of undifferentiated cancer and elucidated a method to determine safe surgical margins for curative resection by EMR/ESD.
Among 47 cases, 7 IIb and 40 IIc cases were diagnosed macroscopically. Most IIb lesions were categorized as intermediate-layer type, while most IIc cases were of superficial or whole-layer type. Undifferentiated gastric cancer arises from the intermediate layer of the mucosa (the proliferative zone) and develops without exposure to the surface of the mucosa. During development, the center of the cancer becomes exposed to the surface, and then the cancer thickens and occupies the whole layer. This process was reported by Yao et al. [6, 7], who showed that the developmental pattern progressed from the “intermediate-layer type or deep-layer type” to the “superficial type” to the “whole-layer type.” The results of this study showed a similar tendency. It was presumed that undifferentiated cancer formed a depression during development and exhibited the morphology of IIb or IIc.
The width of the proliferative zone ranged from 0 to 2,390 μm (605.5 μm on average) in IIc 20 mm or smaller. The maximum width of cancer development from the distinct depression was 2,390 μm along the proliferative zone, so when a lesion of 20 mm or smaller was the target, a distance of 3 mm from the endoscopically diagnosed margin would be sufficient to contain the lesion.
It was more difficult to macroscopically diagnose the expansion of cancer in cases with a greater width of proliferative zone. When compared with background mucosa, the average width of the proliferative zone tended to be greater in the pyloric gland and middle body areas, but there was no significant difference. In terms of lesion size, the width of the proliferative zone tended to be greater in cancers with larger diameter.
Conclusions
Pathological examinations of 47 undifferentiated mucosal gastric cancer 20 mm or smaller in diameter without ulceration (scars) revealed that 3 mm or more from the depression was the macroscopically safe margin for endoscopic treatment of undifferentiated gastric cancer within the scope of the expanded treatment guidelines.
References
Japanese Gastric Cancer Association, ed. Guidelines for Gastric Cancer Treatment (for doctors). 2nd ed. Tokyo: Kanahara Syuppan; 2004. (in Japanese).
Hamada T, Yoshimine T, Kubota H, et al. Endoscopic resection of early gastric cancer: criteria for evaluating treatment outcomes and problems in relation with prognosis. Stomach Intest. 1991;26:255–265. (in Japanese).
Misumi A, Kimoto S, Harada K, et al. Mucosal resection for gastric cancer. Surgery. 1992;54:1304–1314. (in Japanese).
Ninomiya Y, Yanagisawa A, Kato Y, et al. Unresectable intramucosal spread of diffuse-type mucosal carcinoma of less than 20 mm in size. Endoscopy. 2000;32:604–608. doi:10.1055/s-2000-16506.
Nishigami T, Kojima T, Hori K, et al. Pathological diagnosis of expansion of mucosal gastric cancer. Stomach Intest. 2001;36(10):1257–1264. (in Japanese).
Yao T, Fujiwara T, Watanabe H, et al. Endoscopic diagnosis of expansion of gastric cancer. Stomach Intest. 1972;7:725–738. (in Japanese).
Yao T, Mizoguchi M, Okada M, et al. Endoscopic findings of early gastric cancer and comparison in resected specimens. Stomach Intest. 1988;23:55–66. (in Japanese).
Gotoda T, Yanagisawa A, Sasako M, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3:219–225. doi:10.1007/PL00011720.
Muto M, Hamamoto Y, Ono H, et al. EMR of early gastric cancer. Possibilities of expansion of indications for EMR of undifferentiated mucosal gastric cancer. Rinsho Syoukaki Naika. 2001;16:1651–1656. (in Japanese).
Hamada T, Kondo K, Itagaki Y, et al. Outcomes of endoscopic resection of minute undifferentiated gastric cancer. Indications based on cancer size. Stomach Intest. 1995;30:1279–1287. (in Japanese).
Nakano K, Yanagisawa A, Utsude K, et al. Limitations of indications for endoscopic mucosal resection (EMR) of undifferentiated gastric cancer. Pathological view. Stomach Intest. 1995;30:1289–1293. (in Japanese).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sawada, S., Fujisaki, J., Yamamoto, N. et al. Expansion of Indications for Endoscopic Treatment of Undifferentiated Mucosal Gastric Cancer: Analysis of Intramucosal Spread in Resected Specimens. Dig Dis Sci 55, 1376–1380 (2010). https://doi.org/10.1007/s10620-009-0883-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-009-0883-4