Abstract
Background
The efficacy of colorectal endoscopic submucosal dissection (ESD) has been reported mainly from Japanese referral centers. However, ESD is technically difficult and associated with a higher risk of adverse events than endoscopic mucosal resection, especially for novices performing colorectal ESD with little experience in gastric ESD. The current study evaluated the results of colorectal ESD during the clinical learning curve by retrospectively examining the results of colorectal ESD performed by four endoscopists who had experience with fewer than five cases of gastric ESD.
Methods
The study retrospectively investigated the first 20 cases managed by each endoscopist, for a total of 80 cases. The main outcome measurements were procedural time, en bloc resection rate with tumor-free margins (R0 resection rate), and adverse events rate. From among clinicopathologic characteristics, factors that affected main outcome measurements were identified.
Results
Of the 80 cases (56 colonic and 24 rectal lesions; 44 granular laterally spreading tumors (LSTs) and 23 nongranular LSTs, 5 depressed, and 8 protruding), 54 cases (67.5 %) had resection using a standard tip-type knife, and 26 cases (32.5 %) had resection using a small scissors-type knife. The mean tumor diameter was 34.9 ± 14.1 mm, and the mean procedural time was 108.8 ± 53.4 min. The resection in 75 cases (93.8 %) was performed en bloc, and the R0 resection rate was 75 % (60/80). Perforation occurred in six cases (7.5 %) and postoperative hemorrhage in three cases (3.8 %). Multivariate analyses showed that colonic lesions and larger lesions (≥40 mm) were significantly associated with prolonged procedural time (≥90 min). Use of the scissors-type knife was significantly associated with a higher R0 resection rate. Perforation occurred only in colonic lesions.
Conclusions
For novices in colorectal ESD, beginning with rectal and smaller lesions may be advisable. Also, using scissors-type knives may increase the R0 resection rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The efficacy of endoscopic submucosal dissection (ESD) for en bloc resection of mucosal lesions of gastrointestinal neoplasia has been widely reported, especially for early gastric tumors. It enables resection of almost all mucosal and slightly submucosal invasive tumors regardless of their size and shape, even in the colon [1].
The efficacy of colorectal ESD performed by experienced endoscopists has been reported mainly from Japanese referral centers [2–8]. However, colorectal ESD is not established to date as a standard therapy because of its technical difficulty and high risk of adverse events, especially for novices performing colorectal ESD. Indeed, the rate of perforation during colorectal ESD is reported to be higher than for endoscopic mucosal resection (EMR), even in referral centers [9, 10]. Although most cases have been managed conservatively with endoscopic clipping closure and although the per lesion summary estimate of surgery after ESD-related adverse events is reported to be only 1 % (95 % confidence interval (CI) 0–1 %) [11], the higher risk of perforation than for EMR has prevented the widespread use of colorectal ESD.
The following three points represent the main difficulties with the performance of colorectal ESD that are not seen with gastric ESD:
-
(1)
Very thin walls present a high risk of perforation.
-
(2)
Enterobacterium-induced, serious peritonitis may develop in the event of perforation.
-
(3)
The lumen is narrow and angulated, causing poor operability by endoscopy and generating a higher level of difficulty [1].
Therefore, colorectal ESD is very difficult to perform, both for novices performing colorectal ESD in Japan who have little experience with gastric ESD and for skilled endoscopists in Western countries, where early gastric neoplasia is relatively rare [12]. Extensive experience with gastric ESD before the performance of colorectal ESD has been recommended [8, 13].
A questionnaire survey sent to 1,356 institutions in Japan showed that endoscopists performing colorectal ESD also had performed gastric ESD in 92.9 % of these institutions. Additionally, only endoscopists with skills above a certain level were permitted to perform colorectal ESD in 92.3 % of the same institutions [8]. These results reflect a general belief that colorectal ESD is more difficult to perform than gastric ESD.
To improve the efficacy and safety of colorectal ESD, the development of devices or the improvement of current devices may be required. Standard tip-type knives (Flex Knife or Dual Knife; Olympus Optical Co., Tokyo, Japan) may require that endoscopists who perform colorectal ESD have adequate experience to avoid perforation.
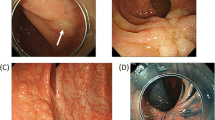
Honma et al. [14] developed a scissors-type grasping device consisting of stag beetle (SB) knives (Sumitomo Bakelite, Tokyo, Japan) that enable resection of tumors without endoscopic movement. These standard and short SB knives have been effective for ESD in the stomach, esophagus, and colon. These authors also developed the SB Knife Jr, specialized for colorectal ESD [15]. The SB Knife Jr has smaller blade tips than standard and short SB knives, and its blades are tapered to enable more accurate and safe ESD procedures. Oka et al. [16] also reported that the SB Knife Jr yielded better results than the Hook Knife in terms of complete en bloc resection and avoidance of perforation. This device may be especially useful for novices performing colorectal ESD.
The current study evaluated the results of colorectal ESD during the clinical learning curve by retrospectively examining the results of colorectal ESD performed by four endoscopists who had little experience with gastric ESD. The study also aimed to identify factors that affected the treatment outcomes.
Materials and methods
Indication criteria for colorectal ESD
The recommended indications for colorectal ESD are as follows:
-
(1)
Lesions difficult to remove en bloc with a snare EMR such as nongranular laterally spreading tumors (LSTs), particularly the pseudo-depressed type, lesions with a type VI pit pattern, and large lesions of the protruding type suspected to be carcinomas
-
(2)
Lesions with fibrosis due to biopsy or peristalsis
-
(3)
Sporadic localized lesions involving chronic inflammation such as ulcerative colitis
-
(4)
Local residual carcinoma after EMR [17].
Because indications 2, 3, and 4 often have a high degree of fibrosis, the ESD procedure for these lesions may possibly be accompanied by adverse events if performed by novices in colorectal ESD. We therefore excluded these lesions in this evaluation.
ESD procedure
Details of the colorectal ESD procedure have been described previously [1–7, 18]. Some of differences between our method and other reported methods are described in the following sections.
Preparation
Patients were instructed to restrict their intake of fiber-rich foods on the day before colorectal ESD and to drink 10 mL of 0.75 % sodium picosulfate solution (Laxoberon; Teijin Pharma Co, Ltd, Tokyo, Japan) after dinner. On the morning of the procedure, 2 L of an isotonic polyethylene glycol electrolyte solution (Niflec; Ajinomoto Pharma Co, Ltd, Tokyo, Japan) with 10 mL of dimeticon (Gascon; Kissei Pharmaceutical, Matsumoto, Japan) was used to achieve good bowel preparation.
Sedative agents
For the purpose of sedation, 15 mg of pentazocine and 2–3 mg of midazolam were administered intravenously before the ESD procedure.
Endoscopic system
Colorectal ESD was performed using single-channel, ultraslim endoscopes with a water jet system: PCF-Q260JI (outer diameter, 10.5 mm; Olympus Optical Co.) for lesions in the proximal colon (from the cecum to the descending colon) and GIF-Q260J (outer diameter 9.8 mm; Olympus Optical Co.) for lesions of the sigmoid colon or rectum. Disposable attachments for the tips of the endoscopes (Elastic touch F-030 or F-025; Top Co., Tokyo, Japan) also were used.
High-frequency generator
We used the ICC 200 high-frequency generator (ERBE, Tübingen, Germany). The settings were endocut mode (effect 2, 60 W) for mucosal incision, forced mode (40 W) for submucosal dissection, and soft-coagulation mode (50 W) for hemostasis. We also used the ESG-100 (Olympus Optical Co.) with the SB Knife Jr. The settings were endocut mode (pulse cut fast, 35 W) for mucosal incision and submucosal dissection and soft-coagulation mode (50 W) for hemostasis.
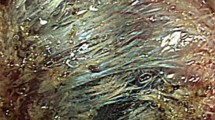
Local injection
A solution of sodium hyaluronate was required for successful performance of mucosal incision and submucosal dissection. We used a mixture comprising a solution of sodium hyaluronate (MucoUp; SEIKAGAKU Co., Tokyo, Japan) and a small volume of epinephrine and indigo carmine.
Knives for incision and dissection
The knives used for mucosal incision and submucosal dissection were standard tip-type knives (Dual Knife; Olympus Optical Co.) or scissors-type knives (SB Knife Jr; Sumitomo Bakelite Co., Tokyo, Japan). We began to use both the Dual Knife and the SB Knife Jr in almost the same phase of the study period.
Instruction of ESD
Each endoscopist in the current study had expertise in therapeutic endoscopy, with experience in managing more than 2,000 cases of total colonoscopy and more than 300 cases of EMR or endoscopic piecemeal mucosal resection (EPMR). Before performing colorectal ESD, each endoscopist had served as an assistant to senior endoscopists for more than 20 cases of colorectal ESD and had undergone training using animal models. They had acquired sufficient knowledge of the ESD procedure during the same period. They also had experienced fewer than five cases of gastric ESD when they began to perform colorectal ESD.
In the current study, for safe performance of colorectal ESD, most of the rectal lesions were resected in the first half of the case series of each endoscopist. In addition, all ESD procedures were supervised by a senior endoscopist with experience of more than 50 cases of colorectal ESD. The senior endoscopist assumed only verbal control of the ESD procedure. However, when a perforation occurred, the subsequent ESD procedure was performed by the senior endoscopist. As a result, the self-completion rate was the same as the rate without perforation.
Study subjects
Colorectal ESD was performed at the Tohoku University Hospital between July 2009 and April 2013 by four endoscopists. The first 20 consecutive cases managed by each endoscopist were evaluated retrospectively. All tumors were larger than 20 mm in diameter. Cases involving neuroendocrine tumors (NETs) or carcinoids were excluded because the histologic characteristics of NET are different from those of adenocarcinomas or adenomas. Written informed consent for the ESD procedure was obtained from all the participants under the protocol approved by the Tohoku University Hospital Committee for Clinical Investigation.
According to the Paris endoscopic classification [19], a macroscopic type of tumor was classified as protruding (0-I) or as nonprotruding and excavated (0-II). The type 0-II lesions were subdivided into slightly elevated (IIa) or depressed (IIc, IIa + IIc) lesions. The IIa lesions larger than 20 mm in diameter were called “LSTs,” and the LSTs were categorized as either the granular (LST-G) or nongranular (LST-NG) type [2–7].
The procedural time was defined as the total time from the onset of the mucosal incision to the end of the submucosal dissection. After the ESD procedure, if the tumor had been resected in a single piece, the resection was endoscopically judged to be an en bloc resection. The resected specimens were fixed in 10 % buffered formalin, paraffin-embedded, sliced at intervals of 2 mm, and microscopically reviewed in accordance with the Vienna classification [20]. Due to the high risk of lymph node metastasis, colectomy was recommended in cases with massive submucosal invasion of more than 1,000 μm, poorly differentiated adenocarcinoma, or vessel infiltration [19, 21].
The grade of resection was histopathologically evaluated as R0 (complete) resection in cases in which the tumor was resected en bloc and the lateral and basal margins were free of tumor cells [2]. In other cases, resection was defined as R1 (incomplete) or Rx (not evaluable) [2].
In this study, procedure-related mortality was defined as any death within 30 days after the ESD. Delayed postoperative hemorrhage was defined as clinical evidence of bleeding manifested by melena or hematochezia that required endoscopic hemostasis within 0 to 14 days after the procedure [5].
We examined the clinicopathologic characteristics of cases such as age, gender, location (rectum or colon), macroscopic type of tumor (LST-G, LST-NG, depressed, protruding), tumor size, and histologic type (adenocarcinomas or adenomas) as well as the knife type used (Dual Knife or SB Knife Jr). The main outcome measurements of this study were procedural time, en bloc resection rate with tumor-free margins (R0 resection rate), and adverse events rate. Among the clinicopathologic characteristics, factors that affected the main outcome measurements were identified using multivariate analyses.
Statistical analysis
Quantitative data are presented as mean ± standard deviation. Discrete variables are presented as median and range. All statistical analyses were performed using the JMP version 9 (SAS Institute Inc., Cary, NC, USA). Differences among groups were evaluated using the chi-square test or Fisher’s exact probability test, as appropriate. A multiple logistic regression method that included all possible variables was used. The level of statistical significance was set at a P value lower than 0.05.
Results
Clinicopathologic characteristics of the 80 patients
The 80 cases in this study included 54 men (67.5 %) and 26 women (32.5 %). The mean age of the entire group was 68.1 ± 9.9 years. The patients in 29 cases (36.3 %) had histories of prior abdominal surgery. Tumors were located at the rectum in 24 cases (30 %) and at the colon in 56 cases (70 %). In terms of macroscopic type, 44 cases (55 %) were identified as LST-G, 23 cases (28.8 %) as LST-NG, 5 cases (6.2 %) as depressed and 8 cases (10 %) as protruding (Table 1).
In all cases, good bowel preparation was achieved early in the afternoon before the colorectal ESD. The mean tumor diameter in the entire group was 34.9 ± 14.1 mm. Of the 80 cases, 24 (30 %) had a tumor diameter of 40 mm or larger and 56 (70 %) had a tumor diameter smaller than 40 mm. Histopathology showed that 39 patients (48.8 %) had adenocarcinomas and 41 patients (51.2 %) had adenomas (Table 1). Five patients had submucosal invasion. Three of these five patients had lymphatic invasion, venous invasion, or massive submucosal invasion greater than 1,000 μm and underwent colectomy.
The Dual Knife was used in 54 cases (67.5 %) and the SB Knife Jr in 26 cases (32.5 %). Of the 54 cases in which the Dual Knife was used, 12 (22.2 %) required another knife or snare. On the other hand, of the 26 cases in which the SB Knife Jr was used, only 2 cases (7.7 %) required another knife or snare (P = 0.089, Fisher’s exact test).
Main outcome measurements of colorectal ESD
The mean procedural time for the 80 cases was 108.8 ± 53.4 min. For 47 (58.8 %) of these 80 cases, the procedural time was 90 min or longer. The en bloc resection (endoscopic) rate was 93.8 % (75/80), and the R0 resection (histologic) rate was 75 % (60/80).
Perforations occurred during six ESD procedures (7.5 %), which were managed by conservative medical treatment with bowel rest and intravenous antibiotics after the endoscopic closure. Delayed postoperative hemorrhage occurred in three cases (3.8 %) and was treated by endoscopic hemostasis. Therefore, the rate of all ESD-induced adverse events was 11.3 % (9/80). No deaths occurred within 30 days after the ESD.
When the 80 cases were divided into the 40 cases in the first half of the study and the 40 cases in the second half, the en bloc resection rate was 87.5 % (35/40) for the first half and 100 % (40/40) for the second half of the study. Similarly, the R0 resection rate increased from 60 % (24/40) in the first half to 90 % (36/40) in the second half of the study. Perforation occurred only in the first half of the study. No case of perforation occurred in the second half of the study.
Factors that affected the prolonged procedural duration (≥90 min)
Among the clinicopathologic characteristics including the location, macroscopic type, tumor size, histologic type, and knife type, the colonic lesions required longer procedural durations than rectal lesions, but the difference was not significant. Significantly more cases with larger lesions (≥40 mm) required prolonged procedural durations than cases with smaller lesions. The procedural duration did not differ significantly in terms of macroscopic type, histologic type, or knife type (Table 2). The procedural duration also was correlated positively with the tumor diameter (r = 0.566; P < 0.0001).
Multivariate analyses showed that colonic lesions and larger lesions (≥40 mm) were independent predictors of prolonged procedural duration (≥90 min), with respective adjusted odds ratios (ORs) of 3.61 (95 % CI 1.05–14.71) and 14.74 (3.58–89.36). No other factors were associated with prolonged procedural duration (Table 2).
Factors that affected the R0 resection rate
Among the clinicopathologic characteristics examined, the R0 resection rate in the SB Knife Jr group was higher than in the Dual Knife group, but the difference was not significant. The other factors examined did not differ (Table 3). Multivariate analyses showed that use of the SB Knife Jr was significantly associated with the R0 resection rate, with an adjusted OR of 3.91 (95 % CI 1.10–18.81). No other factors had a significant influence on the rate of R0 resection (Table 3).
Factors that affected the adverse events rate
All six cases with perforation had colonic lesions. The rate of perforation in the SB Knife Jr group was lower than in the Dual Knife group, but the difference was not significant (Table 4). All three patients who experienced delayed postoperative hemorrhage had larger lesions (≥40 mm) (Table 4). Because the number of cases with perforation or delayed postoperative hemorrhage was very small, multivariate analyses could not be performed.
Discussion
The efficacy of colorectal ESD performed by experienced endoscopists has been reported mainly from Japanese referral centers [2–8]. On the other hand, there have been few reports on colorectal ESD from Western countries [22, 23].
Because of the technical difficulty and the high risk of adverse events, colorectal ESD has not been established to date as a standard therapeutic method. For novices performing colorectal ESD, experience with gastric ESD has been recommended before colorectal ESD is attempted [8, 13]. A panel of experts gathered in Europe similarly stated that ESD should be performed in a step-up approach, starting with lesions presenting in the rectum or the distal stomach, moving on to those in the colon and proximal stomach, and finally to lesions in the esophagus [24].
However, it is difficult for endoscopists in Western countries to perform sufficient gastric ESD procedures to gain such experience because fewer early gastric neoplasias occur in Western countries than in Japan [12]. Therefore, the current data on colorectal ESD during the clinical learning curve may be of great use. In addition, the endoscopists in the current study had experience with fewer than five cases of gastric ESD when they began to perform colorectal ESD. This is a unique point of this study, and the settings of this study were almost the same as those in Western countries.
Needless to say, the experiences of the four endoscopists in the current study were few. Many experts have recommended that novices should experience 20–50 supervised (gastric) ESD cases before starting to perform colorectal ESD [8, 13, 25, 26]. However, because of the very thin wall of the colorectum, colorectal ESD generally requires more delicate control than procedures for the gastric wall. Therefore, it may be better for endoscopists with expertise in colonoscopy or colorectal EMR/EPMR to start colorectal ESD before becoming too familiar with gastric ESD.
On the other hand, similar reports have described novices performing colorectal ESD in Western countries [27, 28]. However, most cases involved rectal lesions, and two endoscopists had a certain amount of experience with gastric and esophageal lesions [27]. In a study reported by Iacopini et al. [28], ESD procedures were performed by only one endoscopist.
For the 80 cases examined in this study, the R0 resection rate was 75 % (60/80), and no ESD-induced fatalities occurred. The lateral margin was judged to be positive when the tumor existed in the first or end slice, even if the lateral and basal margins were free of tumor cells in all slices. Therefore, the R0 resection rate may be lower than in previous studies [2–8]. However, the en bloc resection rate (93.8 %, 75/80) was not low, even compared with previous reports involving expert endoscopists [2–8].
If endoscopists set up slightly larger lateral margins, the R0 resection rate will be satisfactory (close to the en bloc resection rate of 93.8 %). Additionally, in the metaanalysis of ESD versus transanal endoscopic microsurgery (TEM), TEM was reported to achieve a higher R0 resection rate [29]. However, other studies have reported that both ESD and TEM are effective and safe [30, 31].
Clinicians should select ESD or TEM as appropriate, taking their respective advantages into consideration. Although ESD enables minimal invasiveness and avoidance of anesthesia, it has the possibility of additional surgery in cases of massive submucosal invasion.
With regard to adverse events, perforation during the ESD procedure occurred in six cases and delayed postoperative hemorrhage in three cases. All were treated by endoscopic closure and hemostasis. These results indicate that colorectal ESD is feasible and safe during the clinical learning curve.
In terms of factors related to prolonged procedural durations (≥90 min), multivariate analyses showed that colonic lesions and larger lesions (≥40 mm) were significantly associated with prolonged procedural durations. Colonic lesions generally have poor operability by endoscopy and were expected to require higher levels of endoscopic skill and longer procedural durations than rectal lesions. Indeed, Niimi et al. [26] have recommended a training system for colorectal ESD from the rectum to the colon. It stands to reason that larger lesions would be associated with longer procedural durations. In fact, the procedural durations were positively correlated with the tumor diameter. It was reported that lesions measuring 40 mm or larger should have been resected by experienced endoscopists due to prolonged procedural durations [32].
As for factors that affected the R0 resection rate, that of the colon was slightly higher than that of the rectum in the current study. This point was in conflict with those of previous reports. As mentioned in the “Materials and methods” section, most of the rectal lesions were resected in the first half of the case series of each endoscopist. Because of the low endoscopic skill and small margins, the R0 resection rate of the rectum might decrease. If rectal and colonic lesions were resected equally, the location might have a significant influence on the R0 resection rate in multivariate analyses.
As mentioned at the beginning of this report, the SB Knife Jr may be useful for novices with expertise in performing colorectal ESD. The usefulness of another scissors-type knife also has been reported [33]. Although the current study showed no significant difference in the procedural time between the Dual Knife group and the SB Knife Jr group, use of the SB Knife Jr was associated with an increased rate of R0 resection. Because the burning effect of the SB Knife Jr during the incision is moderately strong, we might have set up larger margins, which might have led to the higher R0 resection rate.
Although the problem of the burning effect exists, it is important for novices to perform colorectal ESD safely from all aspects. Indeed, although 22.2 % of the Dual Knife group required another knife or snare because of technical difficulties, only 7.7 % of the SB Knife Jr group required another knife or snare.
Our study had some limitations. First, our study could not exclude selection bias in terms of the knife type and location. The knife for colorectal ESD was not selected randomly, so we might have preferred the SB Knife Jr for lesions presenting perpendicularly to the scope. To evaluate the usefulness of the SB Knife Jr, a prospective cohort study should be performed. As for the location, if rectal and colonic lesions are resected equally, we might be able to exclude selection bias.
Second, because a senior endoscopist observed colorectal ESD performed by novices, the results of colorectal ESD might have been influenced by the skill of the senior endoscopist. Because the endoscopists in the current study had little experience with ESD, supervision by senior endoscopists was necessary to reduce the risk of adverse events.
Third, we are not able to exclude the effect of fibrosis, which might have affected the main outcome measurements. However, the number of lesions with moderate to severe fibrosis was small because we excluded lesions with fibrosis due to biopsy or peristalsis, sporadic localized lesions in chronic inflammation, and local residual carcinoma after EMR.
The ESD procedure is technically challenging for novices. However, the efficacy and the safety of colorectal ESD were demonstrated in the current study. It may be better for novices performing colorectal ESD to begin with rectal and smaller lesions in order to reduce adverse events. In addition, use of the SB Knife Jr may increase the R0 resection rate. We hope the current study will be useful for novices in colorectal ESD. In the future, a prospective study should be undertaken to determine the efficacy and safety of colorectal ESD.
References
Yahagi N, Fujishiro M, Omata M (2004) Endoscopic submucosal dissection of colorectal lesion. Dig Endosc 16:S178–S181
Fujishiro M, Yahagi N, Kakushima N, Kodashima S, Muraki Y, Ono S, Yamamichi N, Tateishi A, Oka M, Ogura K, Kawabe T, Ichinose M, Omata M (2007) Outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasm’s in 200 consecutive cases. Clin Gastroenterol Hepatol 5:678–683
Tamegai Y, Saito Y, Masaki N, Hinohara C, Oshima T, Kogure E, Liu Y, Uemura N, Saito K (2007) Endoscopic submucosal dissection: a safe technique for colorectal tumors. Endoscopy 39:418–422
Tanaka S, Oka S, Kaneko I, Hirata M, Mouri R, Kanao H, Yoshida S, Chayama K (2007) Endoscopic submucosal dissection for colorectal neoplasia: possibility of standardization. Gastrointest Endosc 66:100–107
Saito Y, Uraoka T, Matsuda T, Emura F, Ikehara H, Mashimo Y, Kikuchi T, Fu KI, Sano Y, Saito D (2007) Endoscopic treatment of large superficial colorectal tumors: a case series of 200 endoscopic submucosal dissection (with video). Gastrointest Endosc 66:966–973
Isomoto H, Nishiyama H, Yamaguchi N, Fukuda E, Ishii H, Ikeda K, Ohnita K, Nakao K, Kohno S, Shikuwa S (2009) Clinicopathological factors associated with clinical outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms. Endoscopy 41:679–683
Saito Y, Uraoka T, Yamaguchi Y, Hotta K, Sakamoto N, Ikematsu H, Fukuzawa M, Kobayashi N, Nasu J, Michida T, Yoshida S, Ikehara H, Otake Y, Nakajima T, Matsuda T, Saito D (2010) A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest Endosc 72:1217–1225
Tanaka S, Tamegai Y, Tsuda S, Saito Y, Yahagi N, Yamano HO (2010) Multicenter questionnaire survey on the current situation of colorectal endoscopic submucosal dissection in Japan. Dig Endosc 22:S2–S8
Taku K, Sano Y, Fu KI, Saito Y, Matsuda T, Uraoka T, Yoshino T, Yamaguchi Y, Fujita M, Hattori S, Ishikawa T, Saito D, Fujii T, Kaneko E, Yoshida S (2007) Iatrogenic perforation associated with therapeutic colonoscopy: a multicenter study in Japan. J. Gastroenterol Hepatol 22:1409–1414
Oka S, Tanaka S, Kanao H, Ishikawa H, Watanabe T, Igarashi M, Saito Y, Ikematsu H, Kobayashi K, Inoue Y, Yahagi N, Tsuda S, Simizu S, Iishi H, Yamano H, Kudo SE, Tsuruta O, Tamura S, Saito Y, Cho E, Fujii T, Sano Y, Nakamura H, Sugihara K, Muto T (2010) Current status in the occurrence of postoperative bleeding, perforation, and residual/local recurrence during colonoscopic treatment in Japan. Dig Endosc 22:376–380
Repici A, Hassan C, De Paula Pessoa D, Pagano N, Arezzo A, Zullo A, Lorenzetti R, Marmo R (2012) Efficacy and safety of endoscopic submucosal dissection for colorectal neoplasia: a systematic review. Endoscopy 44:137–147
Suzuki H, Gotoda T, Sasako M, Saito D (2006) Detection of early gastric cancer: misunderstanding the role of mass screening. Gastric Cancer 9:315–319
Hotta K, Oyama T, Shinohara T, Miyata Y, Takahashi A, Kitamura Y, Tomori A (2010) Learning curve for endoscopic submucosal dissection of large colorectal tumors. Dig Endosc 22:302–306
Honma K, Kobayashi M, Watanabe H, Suga T, Tominaga K, Yamagata M, Hiraishi H (2010) Endoscopic submucosal dissection for colorectal neoplasia. Dig Endosc 22:307–311
Homma K, Otaki Y, Sugawara M, Kobayashi M (2012) Efficacy of novel SB Knife Jr examined in a multicenter study on colorectal endoscopic submucosal dissection. Dig Endosc 24:S117–S120
Oka S, Tanaka S, Takata S, Kanao H, Chayama K (2012) Usefulness and safety of SB Knife Jr in endoscopic submucosal dissection for colorectal tumors. Dig Endosc 24:S90–S95
Tanaka S, Oka S, Chayama K (2008) Colorectal endoscopic submucosal dissection: present status and future perspective, including its differentiation from endoscopic mucosal resection. J Gastroenterol 43:641–651
Yamamoto H, Kawata H, Sunada K, Sasaki A, Nakazawa K, Miyata T, Sekine Y, Yano T, Satoh K, Ido K, Sugano K (2003) Successful en bloc resection of large superficial tumors in the stomach and colon using sodium hyaluronate and small-caliber-tip transparent hood. Endoscopy 35:690–694
Participants in the Paris workshop (2003) The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc 58:S3–S43
Schlemper RJ, Riddell RH, Kato Y, Borchard F, Cooper HS, Dawsey SM, Dixon MF, Fenoglio-Preiser CM, Fléjou JF, Geboes K, Hattori T, Hirota T, Itabashi M, Iwafuchi M, Iwashita A, Kim YI, Kirchner T, Klimpfinger M, Koike M, Lauwers GY, Lewin KJ, Oberhuber G, Offner F, Price AB, Rubio CA, Shimizu M, Shimoda T, Sipponen P, Solcia E, Stolte M, Watanabe H, Yamabe H (2000) The Vienna classification of gastrointestinal epithelial neoplasia. Gut 47:251–255
Kitajima K, Fujimori T, Fujii S, Takeda J, Ohkura Y, Kawamata H, Kumamoto T, Ishiguro S, Kato Y, Shimoda T, Iwashita A, Ajioka Y, Watanabe H, Watanabe T, Muto T, Nagasako K (2004) Correlations between lymph node metastasis and depth of submucosal invasion in submucosal invasive colorectal carcinoma: a Japanese collaborative study. J Gastroenterol 39:534–543
Hurlstone DP, Atkinson R, Sanders DS, Thomson M, Cross SS, Brown S (2007) Achieving R0 resection in the colorectum using endoscopic submucosal dissection. Br J Surg 94:1536–1542
Probst A, Golger D, Arnholdt H, Messmann H (2009) Endoscopic submucosal dissection of early cancers, flat adenomas, and submucosal tumors in the gastrointestinal tract. Clin Gastroenterol Hepatol 7:149–155
Deprez PH, Bergman JJ, Meisner S, Ponchon T, Repici A, Dinis-Ribeiro M, Haringsma J (2010) Current practice with endoscopic submucosal dissection in Europe: position statement from a panel of experts. Endoscopy 42:853–858
Sakamoto T, Saito Y, Fukunaga S, Nakajima T, Matsuda T (2011) Learning curve associated with colorectal endoscopic submucosal dissection for endoscopists experienced in gastric endoscopic submucosal dissection. Dis Colon Rectum 54:1307–1312
Niimi K, Fujishiro M, Goto O, Kodashima S, Koike K (2012) Safety and efficacy of colorectal endoscopic submucosal dissection by the trainee endoscopists. Dig Endosc 24:154–158
Probst A, Golger D, Anthuber M, Markl B, Messmann H (2012) Endoscopic submucosal dissection in large sessile lesions of the rectosigmoid: learning curve in a European center. Endoscopy 44:660–667
Iacopini F, Bella A, Costamagna G, Gotoda T, Saito Y, Elisei W, Grossi C, Rigato P, Scozzarro A (2012) Stepwise training in rectal and colonic endoscopic submucosal dissection with differentiated learning curves. Gastrointest Endosc 76:1188–1196
Arezzo A, Passera R, Saito Y, Sakamoto T, Kobayashi N, Sakamoto N, Yoshida N, Naito Y, Fujishiro M, Niimi K, Ohya T, Ohata K, Okamura S, Iizuka S, Takeuchi Y, Uedo N, Fusaroli P, Bonino MA, Verra M, Morino M (2013) Systematic review and meta-analysis of endoscopic submucosal dissection versus transanal endoscopic microsurgery for large noninvasive rectal lesions. Surg Endosc. doi:10.1007/s00464-013-3238-3
Park SU, Min YW, Shin JU, Choi JH, Kim YH, Kim JJ, Cho YB, Kim HC, Yun SH, Lee WY, Chun HK, Chang DK (2012) Endoscopic submucosal dissection or transanal endoscopic microsurgery for nonpolypoid rectal high-grade dysplasia and submucosa-invading rectal cancer. Endoscopy 44:1031–1036
Kawaguti FS, Nahas CS, Marques CF, da Costa Martins B, Retes FA, Medeiros RS, Hayashi T, Wada Y, de Lima MS, Uemura RS, Nahas SC, Kudo SE, Maluf-Filho F (2013) Endoscopic submucosal dissection versus transanal endoscopic microsurgery for the treatment of early rectal cancer. Surg Endosc. doi:10.1007/s00464-013-3302-z
Nakajima T, Saito Y, Tanaka S, Iishi H, Kudo SE, Ikematsu H, Igarashi M, Saitoh Y, Inoue Y, Kobayashi K, Hisasbe T, Matsuda T, Ishikawa H, Sugihara KI (2013) Current status of endoscopic resection strategy for large, early colorectal neoplasia in Japan. Surg Endosc 27:3262–3270
Akahoshi K, Okamoto R, Akahane H, Motomura Y, Kubokawa M, Osoegawa T, Nakama N, Chaen T, Oya M, Nakamura K (2010) Endoscopic submucosal dissection of early colorectal tumors using a grasping-type scissors forceps: a preliminary clinical study. Endoscopy 42:419–422
Acknowledgments
We thank Dr. Rintaro Moroi and Dr. Hitoshi Nagasawa for data collection. We also thank Dr. Shoichi Kayaba and Dr. Manabu Shiraki for providing helpful advice concerning colorectal ESD.
Disclosures
Hisashi Shiga, Katsuya Endo, Masatake Kuroha, Yoichi Kakuta, Seiichi Takahashi, Yoshitaka Kinouchi, and Tooru Shimosegawa have no conflicts of interest or financial ties to disclose.
Funding
This study was not supported by grants from governmental agencies, private sources, or manufacturers of drugs or equipment.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shiga, H., Endo, K., Kuroha, M. et al. Endoscopic submucosal dissection for colorectal neoplasia during the clinical learning curve. Surg Endosc 28, 2120–2128 (2014). https://doi.org/10.1007/s00464-014-3443-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3443-8