Abstract
Background
The current status of colorectal endoscopic submucosal dissection (ESD) performed by endoscopists without colorectal ESD experience is unknown. This study evaluated the quality of colorectal ESD performed by endoscopists without colorectal ESD experience.
Methods
We retrospectively examined the outcomes of 420 consecutive patients with 427 superficial colorectal tumors (male/female, 251/169; mean age, 69 years) who underwent ESD. The procedures were performed by 31 endoscopists without colorectal ESD experience using needle knife-type devices at 13 hospitals from October 2008 to June 2017. Cases were divided into the first and second phases according to the experience of the endoscopist: the first phase included the first 20 cases and the second phase included case 21 and beyond. We also identified factors associated with en bloc resection failure.
Results
Rates of colonic tumors, laterally spreading tumors of the non-granular type, poor scope operability, and severe submucosal fibrosis for the first phase were significantly lower than those for the second phase. The en bloc resection rates for the first and second phases were 93% and 96%, respectively. The factors associated with en bloc resection failure were poor scope operability (odds ratio [OR] 2.6; 95% confidence interval [CI] 1.0–6.5), severe submucosal fibrosis (OR 6.5; 95% CI 2.6–15.9), and the first 20 cases (OR 3.4; 95% CI 1.2–10.1).
Conclusion
Inexperienced endoscopists should initially perform colorectal ESD for tumors without severe submucosal fibrosis under good scope operability for at least 20 cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Endoscopic submucosal dissection (ESD) has been indicated for the treatment of large tumors or tumors with severe submucosal fibrosis because of its capability to achieve complete resection [1,2,3]. Currently, ESD is widely used for the treatment of not only gastric and esophageal tumors but also colorectal tumors. We have previously reported the usefulness and safety of colorectal ESD, even for tumors in difficult locations such as anorectal tumors with hemorrhoids near the dentate line [4] or cecal tumors extending into the appendiceal orifice [5]. Because the morbidity associated with colon carcinomas is increasing in Japan [6], the number of ESD procedures to treat colorectal tumors will also continue to increase. However, for inexperienced endoscopists, colorectal ESD has not yet been considered a common procedure because it is more difficult than gastric and esophageal ESD because it requires superior endoscopic skills. It also involves a higher risk of adverse events than endoscopic mucosal resection (EMR) [7, 8]. To ensure safety, it is important to establish the type of tumors for which endoscopists without colorectal ESD experience should initially perform ESD. However, the current status of colorectal ESD performed by inexperienced endoscopists has not been disclosed, the type of tumors that inexperienced endoscopists should initially perform ESD for, and how endoscopist skills can be improved have yet to be established. Therefore, the aim of this study was to conduct a retrospective multicenter survey to evaluate the quality of colorectal ESD performed by endoscopists without colorectal ESD experience.
Patients and methods
Patients
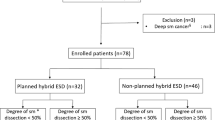
This study included 2879 consecutive patients who had 2979 superficial colorectal tumors that were resected using ESD at 13 hospitals (1 academic hospital and 12 affiliated hospitals [Hiroshima GI Endoscopy Research Group]) between October 2008 and June 2017. We excluded the procedures performed by experts or procedures during which the main operator was substituted by an expert for some reason and the expert completed the residual procedure. Furthermore, we also excluded the cases utilizing devices other than the needle knife-type because needle knife-type devices were commonly used for colorectal ESD and were completely different from other devices, such as scissor-type devices [9]. We retrospectively examined the outcomes of 420 patients with 427 superficial colorectal tumors (male/female, 251/169; mean age, 69 years) who underwent ESD performed by endoscopists without colorectal ESD experience using needle knife-type devices. We divided the cases sequentially into two phases based on the experience of the endoscopist: the first phase included cases 1–20 and the second phase included case 21 and beyond. Then, we compared their clinicopathological characteristics and outcomes of ESD. Figure 1 presents the flowchart of the patient enrollment process with the total number of tumors.
Indications for ESD for superficial colorectal tumors were based on the criteria proposed by the Japan Gastroenterological Endoscopy Society (JGES) [10] and the Japanese Society of Gastroenterology [11]. ESD was indicated for tumors requiring endoscopic en bloc resection and for which en bloc resection using snare EMR would have been difficult [7], such as laterally spreading tumors of the non-granular type (LST-NG), particularly LST-NG pseudo-depressed type, tumors showing a type VI pit pattern, carcinomas with submucosal shallow invasions < 1000 μm, large depressed tumors, and large elevated tumors that were probably malignant, including large nodular lesions such as laterally spreading tumors of the granular type (LST-G). In addition, ESD was indicated for colorectal tumors with submucosal fibrosis (induced by biopsy or peristalsis of the lesion), sporadic localized tumors in chronic intestinal inflammatory conditions such as ulcerative colitis, and local residual or recurrent early-stage carcinomas after endoscopic resection. With regard to the indications, each hospital was allowed to decide which cases should undergo colorectal ESD performed by an endoscopist without colorectal ESD experience.
The study was conducted in accordance with the Declaration of Helsinki. All patients were informed of the risks and benefits of ESD, and each patient provided written informed consent for the use of patient data. The clinical trial number for this study is UMIN000016197 (Institutional Review Board registration date: January 14, 2015).
Operators
Colorectal ESD was performed by 31 endoscopists without colorectal ESD experience at 13 hospitals. All these endoscopists were board-certified fellows of the JGES, had performed more than 1000 colonoscopies, and had experience with more than 20 cases of gastric ESD. Furthermore, they had attended colorectal ESD procedures performed by experts and provided assistance for more than 10 cases prior to performing colorectal ESD.
ESD procedure
The ESD procedures were performed using needle knife-type devices, such as a dual knife (Olympus Medical Systems Corp., Tokyo, Japan) or a flush knife (Fujifilm Corporation, Tokyo, Japan). We excluded the cases utilizing devices other than the needle knife-type, such as SB knife Jr (Sumitomo Bakelite Co., Ltd., Tokyo, Japan) and ITknife nano (Olympus Medical Systems Corp.). After injecting a mixture of a solution of 10% glycerin solution and/or 0.4% sodium hyaluronate (Muco Up; Johnson & Johnson, New Brunswick, NJ, USA) and a small amount of indigo carmine (0.2 mL/20 mL sodium hyaluronate plus glycerin) into the submucosal layer, ESD was performed.
Outcomes of ESD
The following variables were investigated: clinicopathological characteristics of patients and tumors, procedure times, en bloc resection rate, histological complete resection rate, curative resection rate, and adverse events. Poor scope operability was defined as situations that involved paradoxical movement of the endoscope, poor control with adhesions, and lesion motion with heartbeat or breathing, as previously reported [12]. Endoscopically, the degree of submucosal fibrosis was classified as no fibrosis, mild fibrosis, or severe fibrosis, as reported previously [13]. Delayed bleeding was defined as a reduction in the hemoglobin level of 2 g/dL or more in comparison with the latest preoperative level or any sign of apparent bleeding or massive melena [14]. Histological complete resection was defined as resection of the tumor with a pathologically negative horizontal margin and a negative vertical margin. The definition of curative resection in this study was determined using the Japanese Society for Cancer of the Colon and Rectum guidelines criteria, which involved satisfying all four of the following characteristics: a well-differentiated or moderately differentiated papillary carcinoma, no vascular invasion, submucosal invasion depth < 1000 μm, and grade 1 budding [6].
Statistical analyses
JMP statistical software version 13.0 (SAS Institute Inc., Cary, NC, USA) was used for all statistical analyses. A receiver operating characteristic curve analysis was performed to determine the optimal cut-off values of the quantitative data, such as the number of cases that defined the learning phase. Student’s t test and the Mann–Whitney U test were used to compare the continuous variables, whereas Pearson’s Chi square test and Fisher’s exact probability test were used to compare the categorical variables. Among the clinical characteristics, factors influencing the main outcome were identified using a multiple logistic regression method. p < 0.05 was considered statistically significant.
Results
Operator characteristics
Table 1 presents the characteristics of the operators. In the present study, the mean ± standard deviation (SD) number of tumors resected by each operator was 14 ± 16 (range 1–65 cases). The mean ± SD duration between the first and final colorectal ESD performed by each operator during the study period was 30.6 ± 28.3 months (range 2–107 months). Experts took over the procedure for three cases; therefore, the self-completion rate by endoscopists without colorectal ESD experience was 99.3% (427/430).
Clinicopathological characteristics of the cases in each phase
Table 2 summarizes the clinicopathological characteristics of the patients and tumors resected using ESD in each phase. During the first phase (1–20 cases), 295 patients and 300 tumors were included; during the second phase (21 cases or more), 125 patients and 127 tumors were included. The mean ± SD tumor size during the first phase was 29 ± 14 mm, and that during the second phase was 30 ± 13 mm; there was no significant difference. The proportion of rectal tumors during the first phase (43%) was significantly higher than that during the second phase (31%) (p < 0.01). The proportion of LST-NG during the first phase (31%) was significantly lower than that during the second phase (41%) (p < 0.05). The rate of poor scope operability during the first phase (17%) was significantly lower than that during the second phase (28%) (p < 0.05). The rate of severe submucosal fibrosis during the first phase (13%) was significantly lower than that during the second phase (24%) (p < 0.01). There were no significant differences between the two phases in terms of the sex ratio, mean age of patients, ratios of the use of anticoagulants and/or antiplatelet therapy, ratios of local recurrence or discontinued endoscopic resection, and histology.
Outcomes of colorectal ESD during each phase
Table 3 shows the outcomes of colorectal ESD for each phase. The mean ± SD procedure times were 97 ± 67 min for the first phase and 109 ± 76 min for the second phase, with no significant difference. The en bloc resection rates were 93% (278/300) for the first phase and 96% (122/127) for the second phase, with no significant difference. There were no significant differences between the two phases in terms of histological complete resection rates and curative resection rates. Delayed bleeding occurred in three patients (1%) during the first phase and in three patients (2%) during the second phase. Intraoperative perforations occurred in eight patients (3%) during the first phase and in one patient (1%) during the second phase. None of the patients required surgery. There were no significant differences between the two phases in terms of adverse events.
Figure 2 shows the learning curves of the en bloc resection rate and the perforation rate. We sequentially divided the cases into groups of 10 according to each operator’s range of experience. The en bloc resection rates were 93% (203/218), 91% (75/82), 91% (41/45), 97% (29/30), 100% (22/22), and 100% (20/20) for cases 1–10, 11–20, 21–30, 31–40, 41–50, and 51–60, respectively. The perforation rates were 1% (3/218), 6% (5/82), 2% (1/45), 0% (0/30), 0% (0/22), and 0% (0/20) for cases 1–10, 11–20, 21–30, 31–40, 41–50, and 51–60, respectively.
Factors associated with en bloc resection failure
A multivariate analysis revealed that the factors associated with en bloc resection failure were poor scope operability (odds ratio [OR] 2.6; 95% confidence interval [CI] 1.0–6.5), severe submucosal fibrosis (OR 6.5; 95% CI 2.6–15.9), and the first 20 cases (OR 3.4; 95% CI 1.2–10.1). Other factors such as the use of anticoagulants and/or antiplatelet therapy, tumor size, tumor location, and growth type showed no significant correlation with en bloc resection failure (Table 4).
Discussion
Although colorectal ESD had been performed by a limited number of experts in high-volume centers, many hospitals including low-volume centers have recently introduced them. We previously performed a retrospective multicenter survey that included non-specialized hospitals covering the entire Hiroshima area to investigate the current status of colorectal ESD at a regional level [15]. In this study, it was determined that the safety of colorectal ESD at the regional level can be maintained by allocating cases in accordance with the skill level of each hospital. Additionally, it may be important to allocate the cases according to the difficulty of the procedure and the skill level of each endoscopist to achieve safe colorectal ESD.
There have been some reports of the learning curve of colorectal ESD [16,17,18,19,20,21,22,23]. It was reported that 30–100 colorectal ESD procedures are required for endoscopists to achieve proficiency [16,17,18,19,20]. Hotta et al. [16] reported that approximately 80 procedures should be performed to acquire the skills necessary to remove large colorectal tumors successfully and that approximately 40 procedures are sufficient for acquiring the skills necessary to prevent perforations while performing colorectal ESD. Jeon et al. [17] reported that approximately 50 procedures are required for an endoscopist experienced in gastric ESD to achieve a sufficient skill level necessary for performing colorectal ESD for LST, and that colorectal ESD for LST-NG seems to be associated with a higher level of technical difficulty compared to LST-G. However, all of these studies were single-center analyses; depending on each hospital, the characteristics of the cases, the skill level of the endoscopists, and the guidance system may have differed. A learning curve analysis including several endoscopists from different hospitals is required before colorectal ESD can be considered a standard procedure in the near future. Therefore, we conducted a retrospective multicenter survey with a focus on the learning curve to investigate the quality of colorectal ESD performed by inexperienced endoscopists.
We previously reported that poor scope operability and submucosal deep invasion were significant independent predictors of incomplete resections, and that poor scope operability and severe submucosal fibrosis were independent predictors of perforation during colorectal ESD [12]. Imai et al. [24] reported that among less-experienced endoscopists (experience with < 40 cases of colorectal ESD in their series), colonic tumors were independent predictors of en bloc resection. Furthermore, Takeuchi et al. [25] reported that inadequate lifting after the submucosal injection during colorectal ESD, which frequently occurs with LST-NG and protruding tumors, was the risk factor that was most frequently associated with technical difficulties and adverse events. They also mentioned that less-experienced endoscopists (colonoscopy experience < 11 years in their series) should initially perform colorectal ESD for LST-G. In the present study, we allowed each hospital to decide which case should undergo colorectal ESD performed by an endoscopist without colorectal ESD experience. The rates of colonic tumors, LST-NG, poor scope operability, and severe submucosal fibrosis for the first phase were significantly lower than those for the second phase. Because inexperienced endoscopists at each hospital started performing colorectal ESD for tumors with relatively simple conditions, the treatment outcomes of the present study, even for the first phase, were not inferior to those of previous reports [16,17,18,19,20,21,22,23]. However, the treatment outcomes of procedures performed during the second phase were also satisfactory despite dealing with more difficult cases than those encountered during the first phase. There was no difference in procedure times of the first phase and second phase. This may have been related to the fact that there were more difficult cases during the second phase than during the first phase.
A multivariate analysis revealed that the significant factors associated with en bloc resection failure were severe submucosal fibrosis, poor scope operability, and the first 20 cases. Therefore, inexperienced endoscopists should initially perform colorectal ESD for tumors without severe submucosal fibrosis under good scope operability for at least 20 cases. We examined all tumors before ESD and evaluated the scope operability at that time. Furthermore, according to previous reports, large tumor size, LST-NG, fold conversion, and biopsy before ESD were associated with submucosal fibrosis [26,27,28,29]. These characteristics are important for allocating cases according to the skill level of each endoscopist. In fact, an expert took over the procedure for three cases because of poor scope operability.
It has been recommended that endoscopists should acquire experience with 20–50 gastric ESD procedures before performing colorectal ESD [16, 21, 22]. In Japan, it is common for endoscopists without colorectal ESD experience to initially perform ESD for gastric tumors. In the present study, all operators had experience with more than 20 cases of gastric ESD. However, in Western countries, early gastric carcinoma is less common than it is in Japan [30]. Consequently, Western endoscopists have limited opportunities to perform gastric ESD, which is presumed to be easier and safer than colorectal ESD. There have been some reports of the safety of colorectal ESD performed by endoscopists without gastric ESD experience [18, 19, 23]. Yang et al. [18] reported that ESD was attempted for 250 colorectal tumors by an endoscopist without prior gastric ESD experience, and that significant improvements were observed in the success rates and the perforation rates as the surgeons gained further experience. Shiga et al. [19] analyzed the outcomes of 180 consecutive colorectal ESD procedures performed by three endoscopists who had either no experience or experience with fewer than five cases of gastric ESD; they reported that en bloc rates, complete resection rates, and perforation rates improved from 88.3%, 75.0%, and 10.0% during the early phase to 98.3%, 88.3%, and 3.3% during the late phase, respectively. Furthermore, there have been some reports of the feasibility of training involving an animal model or self-learning software for non-experts so that they can improve their skills performing colorectal ESD [23, 31, 32]. These results suggested that gastric ESD experience may not be absolutely required before performing colorectal ESD.
The main strength of the present study is that it was a multicenter study that investigated the outcomes of procedures performed by a large number of endoscopists without colorectal ESD experience. Furthermore, we identified the type of tumors for which inexperienced endoscopists should initially perform colorectal ESD to prevent en bloc resection failure. However, this study also had some limitations. First, this analysis had a retrospective design. Consequently, we could not evaluate the procedure details, such as the presence and degree of assistance offered by expert supervisors. The presence of expert supervisors might have influenced the treatment outcomes [23]. Second, this analysis included only cases using needle knife-type devices to avoid bias caused by differences in devices. Finally, there were considerable variations in the number of procedures performed by each operator. We could not determine whether all endoscopists without colorectal ESD experience would be able to improve the procedure outcomes in the same manner because some of them performed colorectal ESD for only a few cases during the study period. A prospective multicenter study should be performed in the future to address these issues.
In conclusion, endoscopists without colorectal ESD experience can perform colorectal ESD effectively and safely through proper case selection. Inexperienced endoscopists should initially perform colorectal ESD for tumors without severe submucosal fibrosis under good scope operability for at least 20 cases.
References
Cao Y, Liao C, Tan A, Gao Y, Mo Z, Gao F (2009) Meta-analysis of endoscopic submucosal dissection versus endoscopic mucosal resection for tumors of the gastrointestinal tract. Endoscopy 41:751–757
Terasaki M, Tanaka S, Oka S, Nakadoi K, Takata S, Kanao H, Yoshidas S, Chayama K (2012) Clinical outcomes of endoscopic submucosal dissection and endoscopic mucosal resection for laterally spreading tumors larger than 20 mm. J Gastroenterol Hepatol 27:734–740
Oka S, Tanaka S, Saito Y, Iishi H, Kudo SE, Ikematsu H, Igarashi M, Saitoh Y, Inoue Y, Kobayashi K, Hisabe T, Tsuruta O, Sano Y, Yamano H, Shimizu S, Yahagi N, Watanabe T, Nakamura H, Fujii T, Ishikawa H, Sugihara K (2015) Local recurrence after endoscopic resection for large colorectal neoplasia: a multicenter prospective study in Japan. Am J Gastroenterol 110:697–707
Tamaru Y, Oka S, Tanaka S, Hiraga Y, Kunihiro M, Nagata S, Furudoi A, Ninomiya Y, Asayama N, Shigita K, Nishiyama S, Hayashi N, Chayama K (2016) Endoscopic submucosal dissection for anorectal tumor with hemorrhoids close to the dentate line: a multicenter study of Hiroshima GI Endoscopy Study Group. Surg Endosc 30:4425–4431
Boda K, Oka S, Tanaka S, Tanaka H, Matsumoto K, Yamashita K, Sumimoto K, Hirano D, Tamaru Y, Ninomiya Y, Hayashi N, Chayama K (2018) Short-term outcomes of endoscopic submucosal dissection for superficial cecal tumors: a comparison between extension and nonextension into the appendiceal orifice. Ther Adv Gastroenterol 11:1756284818772794
Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, Hamaguchi T, Hyodo I, Igarashi M, Ishida H, Ishihara S, Ishiguro M, Kanemitsu Y, Kokudo N, Muro K, Ochiai A, Oguchi M, Ohkura Y, Saito Y, Sakai Y, Ueno H, Yoshino T, Boku N, Fujimori T, Koinuma N, Morita T, Nishimura G, Sakata Y, Takahashi K, Tsuruta O, Yamaguchi T, Yoshida M, Yamaguchi N, Kotake K, Sugihara K (2015) Japanese Society for Cancer of the Colon and Rectum (JSCCR) Guidelines 2014 for treatment of colorectal cancer. Int J Clin Oncol 20:207–239
Oka S, Tanaka S, Kanao H, Ishikawa H, Watanabe T, Igarashi M, Saito Y, Ikematsu H, Kobayashi K, Inoue Y, Yahagi N, Tsuda S, Simizu S, Iishi H, Yamano H, Kudo SE, Tsuruta O, Tamura S, Saito Y, Cho E, Fujii T, Sano Y, Nakamura H, Sugihara K, Muto T (2010) Current status in the occurrence of postoperative bleeding, perforation and residual/local recurrence during colonoscopic treatment in Japan. Dig Endosc 22:376–380
Niikura R, Yasunaga H, Yamada A, Matsui H, Fushimi K, Hirata Y, Koike K (2016) Factors predicting adverse events associated with therapeutic colonoscopy for colorectal neoplasia: a retrospective nationwide study in Japan. Gastrointest Endosc 84:971.e6–982.e6
Kuwai T, Yamaguchi T, Imagawa H, Sumida Y, Takasago T, Miyasako Y, Nishimura T, Iio S, Yamaguchi A, Kouno H, Kohno H, Ishaq S (2017) Endoscopic submucosal dissection of early colorectal neoplasms with a monopolar scissor-type knife: short- to long-term outcomes. Endoscopy 49:913–918
Tanaka S, Kashida H, Saito Y, Yahagi N, Yamano H, Saito S, Hisabe T, Yao T, Watanabe M, Yoshida M, Kudo SE, Tsuruta O, Sugihara K, Watanabe T, Saitoh Y, Igarashi M, Toyonaga T, Ajioka Y, Ichinose M, Matsui T, Sugita A, Sugano K, Fujimoto K, Tajiri H (2015) JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc 27:417–434
Tanaka S, Saitoh Y, Matsuda T, Igarashi M, Matsumoto T, Iwao Y, Suzuki Y, Nishida H, Watanabe T, Sugai T, Sugihara K, Tsuruta O, Hirata I, Hiwatashi N, Saito H, Watanabe M, Sugano K, Shimosegawa T (2015) Evidence-based clinical practice guidelines for management of colorectal polyps. J Gastroenterol 50:252–260
Hayashi N, Tanaka S, Nishiyama S, Terasaki M, Nakadoi K, Oka S, Yoshihara M, Chayama K (2014) Predictors of incomplete resection and perforation associated with endoscopic submucosal dissection for colorectal tumors. Gastrointest Endosc 79:427–435
Matsumoto A, Tanaka S, Oba S, Kanao H, Oka S, Yoshihara M, Chayama K (2010) Outcome of endoscopic submucosal dissection for colorectal tumors accompanied by fibrosis. Scand J Gastroenterol 45:1329–1337
Tajiri H, Kitano S (2004) Complications associated with endoscopic mucosal resection: definition of bleeding that can be viewed as accidental. Dig Endosc 16:S134–S136
Boda K, Oka S, Tanaka S, Nagata S, Kunihiro M, Kuwai T, Hiraga Y, Furudoi A, Terasaki M, Nakadoi K, Higashiyama M, Okanobu H, Akagi M, Chayama K (2018) Clinical outcome of endoscopic submucosal dissection for colorectal tumors: a large multicenter retrospective study from the Hiroshima GI Endoscopy Research Group. Gastrointest Endosc 87:714–722
Hotta K, Oyama T, Shinohara T, Miyata Y, Takahashi A, Kitamura Y, Tomori A (2010) Learning curve for endoscopic submucosal dissection of large colorectal tumors. Dig Endosc 22:302–306
Jeon HH, Lee HS, Youn YH, Park JJ, Park H (2016) Learning curve analysis of colorectal endoscopic submucosal dissection (ESD) for laterally spreading tumors by endoscopists experienced in gastric ESD. Surg Endosc 30:2422–2430
Yang DH, Jeong GH, Song Y, Park SH, Park SK, Kim JW, Jung KW, Kim KJ, Ye BD, Myung SJ, Yang SK, Kim JH, Park YS, Byeon JS (2015) The feasibility of performing colorectal endoscopic submucosal dissection without previous experience in performing gastric endoscopic submucosal dissection. Dig Dis Sci 60:3431–3441
Shiga H, Ohba R, Matsuhashi T, Jin M, Kuroha M, Endo K, Moroi R, Kayaba S, Iijima K (2017) Feasibility of colorectal endoscopic submucosal dissection (ESD) carried out by endoscopists with no or little experience in gastric ESD. Dig Endosc 29:58–65
Sakamoto T, Saito Y, Nakamura F, Abe S, Takamaru H, Sekiguchi M, Yamada M, Nakajima T, Matsuda T, Yamagishi H, Kato H (2018) Short-term outcomes following endoscopic submucosal dissection of large protruding colorectal neoplasms. Endoscopy 50:606–612
Niimi K, Fujishiro M, Goto O, Kodashima S, Koike K (2012) Safety and efficacy of colorectal endoscopic submucosal dissection by the trainee endoscopists. Dig Endosc 24:154–158
Sakamoto T, Saito Y, Fukunaga S, Nakajima T, Matsudas T (2011) Learning curve associated with colorectal endoscopic submucosal dissection for endoscopists experienced in gastric endoscopic submucosal dissection. Dis Colon Rectum 54:1307–1312
Ohata K, Nonaka K, Misumi Y, Tsunashima H, Takita M, Minato Y, Tashima T, Sakai E, Muramoto T, Matsuyama Y, Hiejima Y, Matsuhashi N (2016) Usefulness of training using animal models for colorectal endoscopic submucosal dissection: is experience performing gastric ESD really needed? Endosc Int Open 4:E333–E339
Imai K, Hotta K, Yamaguchi Y, Kakushima N, Tanaka M, Takizawa K, Kawata N, Matsubayashi H, Shimoda T, Mori K, Ono H (2016) Preoperative indicators of failure of en bloc resection or perforation in colorectal endoscopic submucosal dissection: implications for lesion stratification by technical difficulties during stepwise training. Gastrointest Endosc 83:954–962
Takeuchi Y, Iishi H, Tanaka S, Saito Y, Ikematsu H, Kudo SE, Sano Y, Hisabe T, Yahagi N, Saitoh Y, Igarashi M, Kobayashi K, Yamano H, Shimizu S, Tsuruta O, Inoue Y, Watanabe T, Nakamura H, Fujii T, Uedo N, Shimokawa T, Ishikawa H, Sugihara K (2014) Factors associated with technical difficulties and adverse events of colorectal endoscopic submucosal dissection: retrospective exploratory factor analysis of a multicenter prospective cohort. Int J Colorectal Dis 29:1275–1284
Lee SP, Kim JH, Sung IK, Lee SY, Park HS, Shim CS, Han HS (2015) Effect of submucosal fibrosis on endoscopic submucosal dissection of colorectal tumors: pathologic review of 173 cases. J Gastroenterol Hepatol 30:872–878
Sakamoto H, Hayashi Y, Miura Y, Shinozaki S, Takahashi H, Fukuda H, Okada M, Ino Y, Takezawa T, Sunada K, Lefor AK, Yamamoto H (2017) Pocket-creation method facilitates endoscopic submucosal dissection of colorectal laterally spreading tumors, non-granular type. Endosc Int Open 5:E123–E129
Fu K, Sano Y, Kato S, Fujii T, Iwasaki J, Sugito M, Ono M, Saito N, Yoshida S, Fujimori T (2005) Hazards of endoscopic biopsy for flat adenoma before endoscopic mucosal resection. Dig Dis Sci 50:1324–1327
Fukunaga S, Nagami Y, Shiba M, Sakai T, Maruyama H, Ominami M, Otani K, Hosomi S, Tanaka F, Taira K, Tanigawa T, Yamagami H, Watanabe T, Fujiwara Y (2019) Impact of preoperative biopsy sampling on severe submucosal fibrosis on endoscopic submucosal dissection for colorectal laterally spreading tumors: a propensity score analysis. Gastrointest Endosc 89:470–478
Fock KM (2014) Review article: the epidemiology and prevention of gastric cancer. Aliment Pharmacol Ther 40:250–260
Iacopini F, Bella A, Costamagna G, Gotoda T, Saito Y, Elisei W, Grossi C, Rigato P, Scozzarro A (2012) Stepwise training in rectal and colonic endoscopic submucosal dissection with differentiated learning curves. Gastrointest Endosc 76:1188–1196
Pioche M, Rivory J, Nishizawa T, Uraoka T, Touzet S, O’Brien M, Saurin JC, Ponchon T, Denis A, Yahagi N (2016) Randomized comparative evaluation of endoscopic submucosal dissection self-learning software in France and Japan. Endoscopy 48:1076–1083
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Kazuki Boda, Shiro Oka, Shinji Tanaka, Shinji Nagata, Masaki Kunihiro, Toshio Kuwai, Yuko Hiraga, Akira Furudoi, Koichi Nakadoi, Hideharu Okanobu, Tomohiro Miwata, Shiro Okamoto, and Kazuaki Chayama have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Boda, K., Oka, S., Tanaka, S. et al. Real-world learning curve analysis of colorectal endoscopic submucosal dissection: a large multicenter study. Surg Endosc 34, 3344–3351 (2020). https://doi.org/10.1007/s00464-019-07104-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07104-2