Abstract
Background
Single-incision laparoscopic cholecystectomy (SILC) is a newer approach that may be a safe alternative to traditional laparoscopic cholecystectomy (TLC) based on retrospective and small prospective studies. As the demand for single-incision surgery may be driven by patient perceptions of benefits, we designed a prospective randomized study using patient-reported outcomes as our end points.
Methods
Patients deemed candidates for either SILC or TLC were offered enrollment in the study. After induction of anesthesia, patients were randomized to SILC or TLC. Preoperative characteristics and operative data were recorded, including length of stay (LOS). Pain scores in recovery and for 48 h and satisfaction with wound appearance at 2 and 4 weeks were reported by patients. We used the gastrointestinal quality of life index (GIQLI) survey preoperatively and at 2 and 4 weeks postoperatively to assess recovery. Procedural and total hospital costs per case were abstracted from hospital billing systems.
Results
Mean age of the study group was 44.1 years (±14.8), 87 % were Caucasian, and 77 % were female, with no difference between groups. Operative times were longer for SILC (median = 57 vs. 47 min, p = 0.008), but mean LOS was similar (6.8 ± 4.2 h SILC vs. 6.2 ± 4.8 h TLC, p = 0.59). Operating room cost and encounter cost were similar. GIQLI scores were not significantly different preoperatively or at 2 or 4 weeks postoperatively. Patients reported higher satisfaction with wound appearance at 2 weeks with SILC. There were no differences in pain scores in recovery or in the first 48 h, although SILC patients required significantly more narcotic in recovery (19 mg morphine equivalent vs. 11.5, p = 0.03).
Conclusions
SILC is a longer operation but can be done at the same cost as TLC. Recovery and pain scores are not significantly different. There may be an improvement in patient satisfaction with wound appearance. Both procedures are valid approaches to cholecystectomy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Single-incision laparoscopic surgery was initially described in 1992 [1], with the first report of single-incision laparoscopic cholecystectomy (SILC) published in 1997 [2]. Numerous case series, case–control studies, and several prospective trials have demonstrated the feasibility and safety of SILC [3–6]. However, the overall safety and low complication rate for traditional laparoscopic cholecystectomy (TLC) requires a large sample size to detect a difference between the two approaches when considering end points such as complication rate or blood loss.
Given that it would be difficult to show a significant improvement in the safety outcomes of TLC with SILC, the benefits of the single-incision approach may lie in other domains, such as reduced pain, less narcotic use, shorter hospital stay, faster return to preoperative functional status, and improved cosmesis. It is not clear whether patients perceive these potential advantages as important in their decision-making, and there is currently very little data with which surgeons can inform their patients about what benefits may be expected when choosing single-incision over the traditional laparoscopic approach.
There may be an increase in procedure-related costs with SILC when specialized angled instruments or disposable access devices are required to complete the procedure, or if the single-incision approach results in longer operative times. However, not all surgeons use specialized equipment or access devices, and there is at least one report that SILC can be performed at a cost equivalent to that of TLC [7].
The purpose of the current study is to perform a prospective, randomized, single-blinded trial to study relevant patient-centered and more traditional procedural outcomes of single-incision versus TLC.
Methods
Study site and subject selection
This study was conducted at Saint Luke’s Hospital of Kansas City and was approved by the Institutional Review Board of Saint Luke’s Hospital. Subjects were identified from outpatient clinic schedules by a chief complaint relating to gallbladder disease. Patients were evaluated by one of the three participating surgeons, and if the patient met inclusion criteria, he or she was offered enrollment in the study. Inclusion criteria were (1) age >18, (2) clinical condition requiring elective cholecystectomy, (3) fluency in written and spoken English, and (4) competency to give his/her own informed consent. Patients were excluded if additional procedures were planned or performed with the cholecystectomy, or if the operating surgeon determined the patient was not appropriate for randomization at the outpatient consultation or in the course of preoperative workup. Patients not appropriate for randomization had a high body mass index (BMI), prior upper abdominal incisions, acute gallbladder inflammation, or were unwilling to undergo randomization. Once a patient gave informed consent to participate in the study, baseline demographic information was collected by interview and chart review, and patients completed a gastrointestinal quality of life index (GIQLI) survey.
The GIQLI is a gastrointestinal-specific health-related quality of life (HRQoL) instrument developed and extensively validated in three phases, including a cohort of 194 patients who underwent laparoscopic cholecystectomy [8]. In particular, the GIQLI score improves after cholecystectomy, compared with preoperative scores [9], in both laparoscopic and open cholecystectomy [10].
Surgery
Patients were randomized after induction of anesthesia. Single-incision or TLC was performed using a standardized technique, which was used by all three surgeons. Study patients had only chief residents or minimally invasive surgery fellows scrubbed with attending faculty. Briefly, for TLC, initial peritoneal access was achieved at the umbilicus with either the open Hasson technique or with a Veress needle followed by placement of an 11-mm optical trocar under direct vision. A 5-mm, 30° laparoscope was inserted. Under direct vision, three additional 5-mm trocars were inserted in the epigastrium, right subcostal at the anterior axillary line, and right subcostal at the midclavicular line. The fundus was elevated cephalad and the cystic duct and artery were dissected free, ligated with a 5-mm clip applier, and divided with endo-shears. The gallbladder was dissected off of the liver bed with cautery and placed into an endocatch bag, which was retrieved through the umbilical incision. The umbilical incision was closed with a figure-of-8 0-Vicryl suture. The lateral 5-mm trocar incisions were not closed at the fascial level.
For the single-incision approach, a single skin incision was made at the umbilicus, and initial peritoneal access was achieved with Veress needle insufflation followed by insertion of a 5-mm optical port. Two additional fascial incisions were made slightly cephalad and lateral to the initial port site. A bariatric 5-mm port (5 × 150 mm, Applied Medical, Rancho Santa Margarita, CA) was used in the central incision for a 5-mm, 30° bariatric scope. Two additional low-profile 5-mm ports (5 × 100 mm, Covidien, Mansfield, MA) were used for instruments. When needed, the gallbladder was sutured to the anterior abdominal wall via a 3-0 silk suture passed trans-abdominally on a straight needle. Otherwise, the infundibulum was grasped and elevated cephalad and lateral. All graspers used in the SILS cases were standard laparoscopic graspers; there were no single-incision specialty articulating graspers used. The remainder of the operation was conducted as in the TLC. At the completion of the SILS case, the initial 5-mm fascial incision was dilated to 10–12 mm to allow for specimen retrieval. The dilated incision was closed with a 0-Vicryl figure-of-8 suture. The lateral 5-mm trocar incisions, which were within the rectus fascia, were closed using a single interrupted 0-Vicryl suture. All patients received 0.5 % bupivacaine intradermal and subcutaneously prior to skin incision and prior to skin closure for a total of 30 ml.
Steri-strips and bandages were placed on all patients at the umbilicus, epigastrium, and right upper quadrant at the usual trocar sites of traditional four-port laparoscopic cholecystectomy. Patients were instructed to remove their bandages after 48 h, at which point they were unblinded to which procedure they had. Surgical data collected included length of operation, conversion from SILC to TLC, estimated blood loss, and amount of narcotic (fentanyl) given intraoperatively.
Outcome data
Patient-reported pain scores were recorded during their stay in the post-anesthesia care unit (PACU), as was the amount of narcotic given, converted to morphine equivalents. Length of stay in PACU and total hospital length of stay were recorded. Patients were given a log to record the amount of pain medication (hydrocodone 5 mg/acetaminophen 500 mg) required in the first 48 h, as well as their pain scores. Patients reported when they returned to work or otherwise resumed normal activities. Patients completed GIQLI surveys at 2 weeks and 30 days.
Cost data
The hospital costs for the cholecystectomy procedure and for the encounter, including the procedure, were abstracted from hospital billing data. Direct costs include supplies, instruments, medications, and salaries and are calculated based on a modified ratio of costs to charges methodology. Indirect or overhead costs are allocated using a process similar to a Medicare Step-Down.
Statistical analysis
The primary end point of the study was the difference in the GIQLI score at 4 weeks compared to preoperative, between the SILC and TLC groups. Secondary end points included the difference in the GIQLI score at 2 weeks compared to preoperative, hospital length of stay after surgery in hours, procedural cost, and total encounter cost. GIQLI scores were compared between randomized groups using repeated-measures models, including terms for treatment group, time, treatment-by-time interaction, and an unstructured covariance matrix. The primary comparison of GIQLI outcomes was at the 4-week time point. Cost and length of stay were compared between treatment groups using generalized linear models.
The primary analyses were intent-to-treat and compared patients between the treatment groups to which they were randomized. A secondary analysis was performed comparing the baseline characteristics of those patients who were unenrolled before randomization to those patients with complete follow-up data, and comparing patients with and to those without complete follow-up data. To check the balance between the two arms of the randomization, patient baseline characteristics were compared between the SILC and TLC groups using t-tests for continuous variables and χ2 tests for categorical variables. To check for any selection bias, similar analyses were also run to compare the characteristics between the enrolled and unenrolled patients.
The primary and secondary end points were compared using t tests. To gain more statistic power, a repeated-measures model was used to compare follow-up GIQLI scores at 2 and 4 weeks, adjusting for preoperative GIQLI scores and treatment-by-time interaction. All analyses were conducted using SAS software, release 9.3 (SAS institute, Cary, NC) Two-sided p values <0.05 denote statistical significance. Analyses were performed by the Biostatistical Core at Saint Luke’s Hospital’s Mid-America Heart Institute.
Results
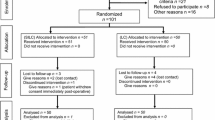
Between March 2010 and January 2012, a total of 103 patients were offered enrollment in the study, based on surgeon assessment of eligibility at the initial office consultation. Of these patients, 19 did not undergo randomization because of patient withdrawal of consent (4), the patient not undergoing cholecystectomy (9), and surgeon determining that the patient was not eligible (6). Eighty-four patients were randomized, and 5 of them were subsequently excluded because additional procedures were performed at the time of cholecystectomy (intraoperative cholangiography in 4 patients, urgent D&C in 1 patient). Thus, 79 patients were included in this analysis, 40 SILC and 39 TLC. Complete cost data are available for 38 SILC and 38 TLC patients, complete 2-week follow-up data are available for 35 SILC and 35 TLC patients, and complete 4-week follow-up data are available for 32 SILC and 27 TLC patients (Fig. 1).
Unenrolled patients were compared with those who remained enrolled to determine if there were imbalances in patient characteristics that might introduce additional bias to the results. We found unenrolled patients were more likely Hispanic or African-American and were less likely to have been evaluated by surgeon C. Patients with incomplete follow-up were likewise compared to patients with complete follow-up and were found to be younger, funded by Medicaid, and Hispanic, and had fewer comorbidities (data not shown).
Baseline characteristics of study patients are summarized in Table 1. There were no significant differences in age, gender, race, insurance provider, prior abdominal surgery, indication for cholecystectomy, BMI, smoking status, or number of comorbidities between the SILC and TLC cohorts. The preoperative GIQLI scores were not different between the groups.
Operative outcomes are summarized in Table 2. There were no conversions to an open procedure and no significant complications (e.g., bile leak, bile duct injury, retained common bile duct stone, need for additional procedures, mortality). One SILC patient required the placement of an additional 5-mm port. Operating room time, from incision to dressing placement, was statistically significantly longer for SILC than for TLC (median = 57 min, range = 22–140 min SILC vs. 47 min, range = 24–85 min TLC). Estimated blood loss and intraoperative narcotic use were similar in the two groups. Recovery room narcotic requirements were higher in SILC patients (median = 19.0 morphine mg equivalents vs. 11.5 morphine mg equivalents), with similar pain scores on a 1–10 scale at PACU discharge (median = 4 for SILC vs. 3.4 for TLC). PACU and total hospital lengths of stay were equivalent. Likewise, average pain scores over the first 48 h as well as the amount of narcotic used during that time were similar between SILC and TLC groups.
GIQLI scores preoperatively and at 2 and 4 weeks postoperatively are depicted in Fig. 2. Patients’ scores in each group improved at the 2- and 4-week time points compared to the preoperative level, but there was no difference in absolute values or in the difference from preoperative to postoperative values between SILC and TLC cohorts. Patients’ responses to the question “How satisfied are you with the appearance of your incision?” are represented in Figs. 3 and 4. At 2 weeks, the SILC patients had a significantly higher level of satisfaction with the appearance of their incisions, but this significance disappeared at the 4-week time point.
Figure 5 summarizes the mean procedural and total encounter costs for the SILC and TLC cohorts. Procedure costs were $945.80 ± $234.50 for SILC and $954.10 ± $206.50 for TLC (p = 0.87). Encounter costs were $3228.20 ± $915.70 for SILC and $3198.50 ± $716.40 for TLC (p = 0.88).
Discussion
Laparoscopic cholecystectomy has been the gold standard for treatment of benign gallbladder disease since the NIH consensus conference and subsequent published statement in 1992 [11]. While initial reports described higher rates of common bile duct injury with laparoscopic cholecystectomy compared with open procedures [12], subsequent work demonstrated that traditional four-port laparoscopic cholecystectomy is a safe operation [13].
The single-incision approach to laparoscopic cholecystectomy is an innovation that strives to make the procedure even less invasive. Over the past 3 years, there has been an increasing number of case series [14], case–control series [4, 5], and now randomized prospective trials [6, 15, 16] to study the procedural outcomes of SILC. While feasibility and safety outcomes comparable to those of TLC have been shown, there is a paucity of level I evidence to use when discussing specific advantages or disadvantages of a single-incision approach that may be important to a particular patient.
The touted advantages of SILC include better cosmesis because of fewer scars, and less pain, which may result in less narcotic use and faster return to normal activity; thus, we designed a prospective study to evaluate these patient-centered outcomes. Our population consisted of purely elective, outpatient surgeries due to our observation that acute inflammation is more often associated with prolonged operative times and a need to convert from SILC with additional ports [17].
We found no difference in pain scores between the groups at discharge from PACU, although our SILC population received a significantly higher amount of narcotic in PACU despite identical amounts of intraoperative narcotic. This is in direct contradistinction to a randomized trial from Greece that showed significantly lower pain scores at all postoperative time points [15]. That study used multiple adjuncts to reduce pain, including intraperitoneal infusion of local anesthetic, suggesting that these interventions may improve pain levels for patients undergoing laparoscopic cholecystectomy by any approach. Additionally, the investigators asked patients to rate shoulder tip pain and abdominal pain separately, whereas our study recorded an overall pain score. It is difficult to understand how the single-incision approach would impact shoulder pain, as was shown in the Greek study, perhaps indicating that the lack of blinding influenced patients’ perception of pain.
Our cohorts recorded similar pain levels and narcotic use over the first 48 h, during which time they were theoretically blinded to which surgery they had by uniform dressings. Bencsath et al. [18] surveyed patients who had undergone laparoscopic cholecystectomy within 1–3 years and found that 66 % of patients who recalled one incision being the most painful identified it as the umbilical incision. Patients were asked if they wished, in retrospect, that they could have eliminated an incision. Most patients wished to eliminate the umbilical incision; the majority of patients who would choose to eliminate the epigastric incision had had a 10–12-mm port in that location. Together, these observations suggest that approaches limiting or eliminating the umbilical incision may actually have more impact on postoperative pain.
We sought to measure the impact of SILC on patients’ recovery by recording the number of days from surgery to return to normal activities and by administering a GI-specific quality-of-life instrument before surgery and at 2 and 4 weeks postoperatively. The GIQLI was validated in a cohort of 194 patients who underwent laparoscopic cholecystectomy [8]; it showed responsiveness and internal consistency and outperformed generic quality-of-life instruments such as the SF-36 when applied to patients with gastrointestinal conditions [10]. We found an increase in GIQLI scores between preoperative and 2-week postoperative time points and between the 2 and 4-week postoperative time points, in an order of magnitude consistent with other studies of similar time points [8]. Those observations correlate with a mean number of 8 days between surgery and returning to work or other normal activities, in both cohorts. The fact that we did not detect a difference in GIQLI scores at 2 or 4 weeks between the SILC and TLC cohorts may mean that there is not a detectable difference in recovery with the single-incision approach, that the difference occurs prior to the 2-week time period, or that our sample size was too small to detect such a difference. We favor the former explanation.
We found no difference in length of stay between our groups, which is a different result compared with a case–control series performed at our institution [17]. This is likely the effect of recent efforts to implement fast-track pathways for laparoscopic cholecystectomy of any approach, which occurred during the period of our former study. For elective cholecystectomy under these conditions, postoperative length of stay may be driven more by symptoms of nausea or other reactions to anesthesia than by direct surgical issues.
Patient-reported level of satisfaction with the cosmetic outcome was statistically significantly higher at the 2-week time point in the SILC group, with a loss of significance at the 4-week time point driven by a greater number of patients in the TLC group reporting being “completely satisfied” with their wound appearance. Studies assessing patient satisfaction with the appearance of their cholecystectomy incision at later time points have found a high level of satisfaction, indicating that “improved cosmesis” may be a solution to a problem that does not necessarily exist [18, 19]. Bencsath’s survey of post-cholecystectomy patients found that 46 % recalled fewer incisions than they actually had at the time of surgery. Thus, while patients may fear poor cosmesis from a four-port approach preoperatively, the data suggest that most patients are satisfied with their incision appearance after the fact, even as early as 4 weeks postoperatively.
Finally, our cost data are comparable for the procedure and the encounter. Our single-incision approach during this study did not involve the routine use of specialized access devices, which would likely be the primary driving factor behind increased healthcare costs. There are a variety of ports available that are designed for single-incision surgery. Most of these are disposable and the cost of using them can exceed several hundred dollars. These ports also require an unnecessarily large fascial incision, which is likely to influence pain levels. The statistically but perhaps not clinically significant increase in operating room time did not translate into increased cost. This may not hold true when attempting SILC in patients with acute cholecystitis or other inflammatory conditions. Love et al. [7] also found equivalent costs in the single-incision approach compared to TLC, with increased costs associated with conversion to an open procedure.
One unintended consequence of SILC in a teaching practice is the impact on training. When designing our study, we noted that junior residents participating in SILC procedures tended to function as an assistant rather than surgeon, although this varied with an individual resident’s skills and experience. We limited trainee participation to chief residents and fellows to control for the impact of the resident’s learning curve on operation time. Laparoscopic cholecystectomy is frequently one of the first laparoscopic procedures that a junior resident will learn, and if that experience is limited or delayed due to the increased technical demands of the single-incision approach, then residents may experience a delay in acquiring laparoscopic operative skills in this and other procedures.
Recently, a robot-assisted laparoscopic cholecystectomy platform has been introduced for the daVinci system. There is no evidence to support any advantage to this extremely expensive approach to gallbladder disease; the only application a robot-assisted laparoscopic cholecystectomy has in practice is for a surgical team to gain experience using the robot in preparation for more complex procedures.
In summary, we found no difference in patient-centered outcomes in patients undergoing SILC compared to TLC, with the exception of increased satisfaction with wound appearance at 2 weeks. Our SILC cases took an average of 10 min longer, without an increase in procedural or total encounter costs. These findings must be interpreted in the context of our study population, which was limited to elective, outpatient cholecystectomy, resulting in a relatively socioeconomically privileged patient sample. In the absence of an appropriately powered study to provide level I evidence, it is reasonable to conclude from our study and others that the single-incision approach is a safe and valid approach to laparoscopic cholecystectomy, in properly trained surgeons’ hands and in an appropriately selected patient. However, the safety of SILC is still under scrutiny, and our study was not designed or powered to detect a difference in complications. It is likely that demand for this operation will be driven by patients’ perceptions of benefit, despite the strength of the supporting data. It then becomes the surgeon’s responsibility to provide a safe operation without an undue increase in healthcare cost, and those seem reasonable goals in light of the accumulating data on SILC.
References
Pelosi MA, Pelosi MA 3rd (1992) Laparoscopic appendectomy using a single umbilical puncture (minilaparoscopy). J Reprod Med 37:588–594
Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I (1997) One-wound laparoscopic cholecystectomy. Br J Surg 84:695
Rivas H, Varela E, Scott D (2010) Single-incision laparoscopic cholecystectomy: initial evaluation of a large series of patients. Surg Endosc 24:1403–1412
Chang SK, Tay CW, Bicol RA, Lee YY, Madhavan K (2011) A case-control study of single-incision versus standard laparoscopic cholecystectomy. World J Surg 35:289–293
Gangl O, Hofer W, Tomaselli F, Sautner T, Fugger R (2011) Single incision laparoscopic cholecystectomy (SILC) versus laparoscopic cholecystectomy (LC)—a matched pair analysis. Langenbecks Arch Surg 396:819–824
Phillips MS, Marks JM, Roberts K, Tacchino R, Onders R, Denoto G, Rivas H, Islam A, Soper N, Gecelter G, Rubach E, Paraskeva P, Shah S (2012) Intermediate results of a prospective randomized controlled trial of traditional four-port laparoscopic cholecystectomy versus single-incision laparoscopic cholecystectomy. Surg Endosc 26(5):1296–1303
Love KM, Durham CA, Meara MP, Mays AC, Bower CE (2011) Single-incision laparoscopic cholecystectomy: a cost comparison. Surg Endosc 25:1553–1558
Eypasch E, Williams JI, Wood-Dauphinee S, Ure BM, Schmulling C, Neugebauer E, Troidl H (1995) Gastrointestinal quality of life index: development, validation and application of a new instrument. Br J Surg 82:216–222
Lien HH, Huang CC, Wang PC, Huang CS, Chen YH, Lin TL, Tsai MC (2010) Changes in quality-of-life following laparoscopic cholecystectomy in adult patients with cholelithiasis. J Gastrointest Surg 14:126–130
Shi HY, Lee HH, Chiu CC, Chiu HC, Uen YH, Lee KT (2008) Responsiveness and minimal clinically important differences after cholecystectomy: GIQLI versus SF-36. J Gastrointest Surg 12:1275–1282
United States National Institutes of Health (1992) Gallstones and laparoscopic cholecystectomy. NIH Consens Statement 10:1–28
Moore MJ, Bennett CL (1995) The learning curve for laparoscopic cholecystectomy. The Southern surgeons club. Am J Surg 170:55–59
Flum DR, Koepsell T, Heagerty P, Sinanan M, Dellinger EP (2001) Common bile duct injury during laparoscopic cholecystectomy and the use of intraoperative cholangiography: adverse outcome or preventable error? Arch Surg 136:1287–1292
Elsey JK, Feliciano DV (2010) Initial experience with single-incision laparoscopic cholecystectomy. J Am Coll Surg 210:620–624, 624–626
Tsimoyiannis EC, Tsimogiannis KE, Pappas-Gogos G, Farantos C, Benetatos N, Mavridou P, Manataki A (2010) Different pain scores in single transumbilical incision laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc 24:1842–1848
Marks J, Tacchino R, Roberts K, Onders R, Denoto G, Paraskeva P, Rivas H, Soper N, Rosemurgy A, Shah S (2011) Prospective randomized controlled trial of traditional laparoscopic cholecystectomy versus single-incision laparoscopic cholecystectomy: report of preliminary data. Am J Surg 201:369–372 discussion 372–363
Joseph S, Moore BT, Sorensen GB, Earley JW, Tang F, Jones P, Brown KM (2011) Single-incision laparoscopic cholecystectomy: a comparison with the gold standard. Surg Endosc 25:3008–3015
Bencsath KP, Falk G, Morris-Stiff G, Kroh M, Walsh RM, Chalikonda S (2012) Single-incision laparoscopic cholecystectomy: do patients care? J Gastrointest Surg 16:535–539
Bignell M, Hindmarsh A, Nageswaran H, Mothe B, Jenkinson A, Mahon D, Rhodes M (2011) Assessment of cosmetic outcome after laparoscopic cholecystectomy among women 4 years after laparoscopic cholecystectomy: is there a problem? Surg Endosc 25:2574–2577
Disclosures
Dr. Brown and Dr. Margolin received a research Grant from Covidien to fund the current study. Dr. Moore and Dr. Sorensen have received honoraria and proctor fees from Covidien and Ethicon. Mr. Boettger, Ms. Tang, and Mr. Jones have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brown, K.M., Moore, B.T., Sorensen, G.B. et al. Patient-reported outcomes after single-incision versus traditional laparoscopic cholecystectomy: a randomized prospective trial. Surg Endosc 27, 3108–3115 (2013). https://doi.org/10.1007/s00464-013-2914-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-2914-7