Abstract
Background
The volume–outcome relationship has been validated previously for surgical procedures and cancer treatments. However, no studies have longitudinally compared the relationships between volume and outcome, and none have systematically compared laparoscopic cholecystectomy (LC) surgery outcomes in Taiwan. This study purposed to explore the relationship between volume and hospital treatment cost after LC.
Methods
This cohort study retrospectively analyzed 247,751 LCs performed from 1998 to 2009. Hospitals were classified as low-, medium-, and high-volume hospitals if their annual number of LCs were 1–29, 30–84, ≥85, respectively. Surgeons were classified as low-, medium-, and high-volume surgeons if their annual number of LCs were 1–10, 11–24, ≥25, respectively. Hierarchical linear regression model and propensity score were used to assess the relationship between volume and hospital treatment cost.
Results
The mean hospital treatment cost was US $2,504.53, and the average hospital costs for high-volume hospitals/surgeons were 33/47 % lower than those for low-volume hospitals and surgeons. When analyzed by propensity score, the hospital treatment cost differed significantly between high-volume hospitals/surgeons and low/medium-volume hospitals/surgeons (2,073.70 vs. 2,350.91/2,056.73 vs. 2,553.76, P < 0.001).
Conclusions
Analysis using a hierarchical linear regression model and propensity score found an association between high-volume hospitals and surgeons and hospital treatment cost in LC patients. Moreover, the significant factors associated with hospital resource utilization for this procedure include age, gender, comorbidity, hospital type, hospital volume, and surgeon volume. Additionally, analysis of the treatment strategies adopted at high-volume hospitals or by high-volume surgeons may improve overall hospital treatment cost.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The medical literature consistently shows that, for many surgical procedures, desirable outcomes are positively associated with the frequency at which the procedure is performed by a hospital or surgeon [1, 2]. Therefore, volume is a common measure of surgical care quality, particularly that for prevalent or high-risk procedures, including laparoscopic cholecystectomy (LC) [3]. That is, lengths of stay (LOS), hospital costs, and complication rates associated with LC are expected to be high when volume is high [3–5]. However, even in high-volume medical centers, outcomes still depend on the volume of procedures performed by individual surgeons. For example, surgeon volume has been linked to patient outcomes in gastrointestinal surgery and may at least partly explain the apparent institutional volume effect [6].
Although convincing evidence suggests that hospital volume and surgeon volume contribute to favorable outcomes, other specific predictors of LOS, hospital treatment cost, and the reproducibility of health care practices that tend to obtain favorable outcomes have not been clearly defined [7]. Moreover, in most previous volume–outcome studies, a multiple linear regression was routinely used, raising the possibility that selection bias might still exit. Additionally, no studies have longitudinally compared the relationships between hospital/surgeon volume and outcome, and none have systematically compared LC surgery outcomes in Taiwan.
This study explored the association between hospital volume and surgeon volume and hospital treatment cost using population-based data, hierarchical linear regression analysis, and propensity score to minimize the effect of selection bias.
Materials and methods
Patients and study design
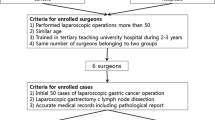
This study analyzed administrative claims data obtained from the Taiwan Bureau of National Health Insurance (BNHI). Because the BNHI is the sole payer in Taiwan, the BNHI data set was assumedly the most comprehensive and reliable data source for the study. Patients were classified as LC if their records revealed codes for primary or secondary diagnosis of gallbladder stones, gallbladder polyps, or acute cholecystitis (codes 574.00–576.99) and a procedure code for LC (code 51.23). Patients diagnosed with gallbladder cancer were excluded from the study sample. The final study sample included 247,751 patients who had received LC between January 1, 1998 and December 31, 2009. The study protocol was approved by the Institutional Review Board of Kaohsiung Medical University Hospital.
Potential confounders
The analyzed patient characteristics included age, gender, and comorbidity. Comorbidity was estimated using the Charlson index [8]. The analyzed hospital characteristics were hospital volume, surgeon volume, LOS, and hospital treatment cost. Hospitals/surgeons were further sorted by their total patient volume by using the unique hospital/surgeon identifiers in this database. Surgeon and hospital volume cut points were then selected to divide patients into approximately equal volume-based tertiles. Hospitals were classified as low-, medium-, and high-volume hospitals if their annual number of LCs were 1–29, 30–84, >85, respectively. Surgeons were classified as low-, medium-, and high-volume surgeons if their annual number of LCs were 1–10, 11–24, >25, respectively.
Statistical analysis
The study period was divided into three approximately equal time intervals: period 1: 1998–2001; period 2: 2002–2005; and period 3: 2006–2009. Regarding hospital treatment costs, the data analysis included costs in standard administrative claims data required by the Taiwan BNHI: operating room, radiology, physical therapy, hospital room, anesthetist, pharmacy, laboratory, special materials, surgeon, and others. Hospital treatment cost was adjusted for specific hospital levels according to their differences in BNHI reimbursements. To reflect changes in real dollar value, cost data also were adjusted by the consumer price index for each year of 1998–2009 (91.52, 93.06, 93.22, 94.39, 94.38, 94.19, 93.93, 95.45, 97.65, 98.23, 99.22, and 100.00, respectively). Additionally, all dollar values at the end of each year were adjusted to 2009 Taiwan currency values. Hospital treatment cost was then converted from Taiwan dollars to U.S. dollars at an exchange rate of 30.5:1, which was the average exchange rate during 1998–2009. Finally, multiple linear regression models and propensity analysis were used to compare hospital treatment cost between different volume groups.
The hierarchical linear regression model was used to analyze the relationship between hospital treatment cost of the different volume groups and those of the reference group after adjusting for age, gender, Charlson comorbidity index (CCI), hospital type, hospital volume, and surgeon volume. In this study, the hierarchical linear regression method was used because of concern over the potential for a hospital clustering effect where hospital policies, procedures, or surgeon compensation mechanisms that were unique to each hospital could impact on the quality and cost of care [9, 10].
Propensity analysis was used to reduce the effect of selection bias on our hypothesis as described by Joffe and Rosenbaum [11] and Rubin [12]. Propensity score stratification replaces these covariates that may be present in an observational study with a variable of these factors. To calculate the propensity score, patient characteristics and hospital characteristics in this study were entered into a logistic regression model predicting selection for high-volume hospitals/surgeons. The study population was then divided into four discrete strata on the basis of propensity score. The effect of volume assignment on hospital treatment cost was analyzed within each quartile. Comparisons of propensity-matched low/medium-volume and high-volume hospitals/surgeons of hospital treatment cost were undertaken using paired t tests or Wilcoxon signed-rank tests. The Mantel–Haenszel odds ratio was calculated in addition to the Cochran–Mantel–Haenszel χ 2 statistic.
Statistical analyses were performed with SPSS version 15.0 (SPSS Inc., Chicago, IL) and Stata Statistical Package, Version 9.0 (Stata Corp, College Station, TX). All tests were two-sided, and P values less than 0.05 were considered statistically significant.
Results
Table 1 lists the differences between low-, medium-, and high-volume hospitals in terms of patient characteristics and hospital characteristics. The mean hospital treatment cost was significantly lower for high-volume hospitals than for low-volume hospitals (P < 0.001). Otherwise, there was no statistical difference in patients’ gender, age, and CCI score between groups (Table 2). Additionally, patients who received LC by high-volume surgeons were more likely to get lower hospital treatment cost than those by low-volume surgeons (P < 0.001; Table 3).
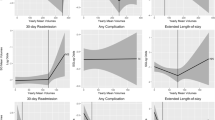
The hierarchical linear regression model showed that, compared with low-volume hospitals, mean hospital treatment cost was significantly lower in high-volume hospitals ($823.74 lower; P < 0.001). For all hospitals, the mean hospital treatment cost was $2,504.53 dollars. Average hospital treatment cost for high-volume was 33 % lower than those for low-volume hospitals after adjusting for patient characteristics and hospital characteristics. Moreover, mean hospital treatment cost for procedures performed by high-volume surgeons were significantly lower compared with those for procedures performed by low-volume surgeons ($1,182.68 dollars lower; P < 0.001). Similarly, average hospital costs for high-volume surgeons was 47 % lower than those for low-volume surgeons after adjusting for patient characteristics and hospital characteristics. Additionally, hospital treatment cost was significantly lower in females than in males and were significantly associated with age, hospital type, and CCI score (P < 0.001).
Patients were stratified by propensity score and the effect of hospital volume on hospital treatment cost was assessed. The population was stratified into propensity quartiles as previously described. Table 4 shows the percentage of patients treated at low/medium-volume hospitals from the first propensity quartile to the fourth as predicted by the propensity model. In each of the four strata, patients treated at high-volume hospitals had a lower hospital treatment cost. The P value for the Cochran–Mantel–Haenszel statistic for the difference in hospital treatment cost between patients treated at low/medium- and high-volume hospitals, while controlling for propensity score, was <0.001 (adjusted odds ratio = 0.57; 95 % confidence interval (CI), 0.38–0.77). The adjusted hospital treatment cost for low/medium- and high-volume hospitals were 70 and 41 % (P < 0.001). It also shows the percentage of patients treated by low/medium-volume surgeons from the first propensity quartile to the fourth as predicted by the propensity model (Table 5). In each of the four strata, patients treated by high-volume surgeons had a lower hospital treatment cost. The adjusted hospital treatment costs for low/medium- and high-volume surgeons were 71 and 40 % (P < 0.001).
In summary, the robustness of this result was demonstrated by two different multivariate analyses, the hierarchical linear regression model and stratification by propensity score.
Discussion
Using a hierarchical linear regression model and propensity score, the relative benefit of treatment at high-volume hospitals or by high-volume surgeons over low/medium-volume hospitals or low/medium-volume surgeons was evaluated in LC. After controlling for patient characteristics and hospital characteristics in the hierarchical linear regression model, the adjusted parameter estimate was −$823.74 dollars for high-volume hospitals or −$1,182.68 dollars for high-volume surgeons, indicating that LC patients treated at high-volume hospitals or by high-volume surgeons had a lower hospital treatment cost. When analyzed by propensity score, the adjusted hospital treatment cost was 41 % for patients treated at high-volume hospitals or 40 % by high-volume surgeons and 70 % for patients treated at low/medium-volume hospitals or 71 % by high-volume surgeons. Moreover, fewer patients treated at high-volume hospitals or by high-volume surgeons had a high hospital treatment cost. The results of both forms of analyses led to the conclusion that hospital treatment cost for LC patients treated at high-volume hospitals or by high-volume surgeons were significantly better, which is consistent with the literature [13–15].
Although precise cutoffs for LC volume could not be defined, surgeon volume and hospital volume consistently showed a positive association with outcome. As reported elsewhere, factors that correlated positively with hospital treatment cost included advanced age, male gender, high CCI score, current treatment at a district hospital, current treatment at low-volume hospitals, and current treatment by low-volume surgeons [5–7].
In comparison with reports that used data for a single medical center, this national registry study based on data from the BNHI in Taiwan gives a better overview of the current practice of LC surgery. Unlike single-center series studies, data from registry studies provide an overview of practices in large populations while avoiding referral bias or bias reflecting the practices of individual surgeons or institutions [3, 16]. Moreover, all BNHI copayments are standardized throughout the country. Additionally, in the hierarchical linear regression model applied in this study, the two-level model was adjusted for cluster effects to avoid overemphasizing association [17].
The use of propensity scores to create a risk-adjusted, matched model based on hospital volume or surgeon volume was an important advantage of our study. Propensity score measures the likelihood that a person would have been treated using the covariates score [11, 12]. This allowed for a straightforward analysis of whether the low/medium-volume and high-volume groups had enough overlap with respect to observed covariates for a true assessment of the effect that hospital volume and surgeon volume had on the use of LC. These two volume groups in our propensity-matched model were virtually identical with respect to entire patient characteristics and hospital characteristics.
The literature shows not only an increasing incidence of LC procedures, but also an increase in associated hospital treatment costs [18]. This study found that hospital treatment cost for inpatient care of patients who had received LC at high-volume hospitals and by high-volume surgeons were significantly lower than those of patients who had received LC at low-volume hospitals and by low-volume surgeons. Hospital costs were 33 % lower in high-volume hospitals than in low-volume hospitals and 47 % lower in high-volume surgeons than in low-volume surgeons. Therefore, limiting LC procedures in Taiwan to high-volume hospitals or high-volume surgeons would potentially save $205–292 million dollars in annual hospital costs. The observed inverse volume-cost relationship is consistent with cost analyses showing that the costs of other procedures [7]. However, few studies have explored how the economic burden of LC procedures is related to hospital volume or surgeon volume [19].
Previous studies reveal that several patient characteristic and hospital characteristics have strong correlations with hospital treatment cost [4, 14]. However, the limited availability of claims data in the present study precluded analysis of many patient and hospital parameters. Advanced age reportedly has a strong positive association with a high CCI score. The literature also shows that hospital treatment cost tends to be higher in patients with CCI score [10]. Analysis of gender differences in hospital treatment cost incurred by the LC surgery patients in this study also indicated that females tended to have lower hospital treatment cost than males did. Although further study is needed, one possibility is that the disease tends to be more severe in males than in females at the time of surgery because males tend to delay surgery [20].
Several hypotheses for the cost-volume relationship have been proposed. The “practice makes perfect” hypothesis proposes that high surgical volumes increase the opportunities to improve not only surgical skills, but also the implementation and cost-effectiveness of the overall treatment [7]. Surgical skill clearly improves with experience. Compared to a low-volume surgeon, a high-volume surgeon with well-trained staff tends to have a shorter operating time and better performance in selecting appropriate antimicrobials and surgical procedures and in planning for discharge, which reduces complication rates, LOS, mortality rate, and hospital treatment cost [7, 13–15]. Regarding the selective referral hypothesis, surgical patients in Taiwan tend to rely on their own judgment when selecting a surgeon or hospital due to lack of a formal referral system [21, 22]. Because no source of official performance data is available for reference when selecting a healthcare provider, patients tend to select surgeons or hospitals based on the recommendations of friends and relatives [21, 22].
We acknowledge several limitations of this study. First, the clinical picture obtained by analyzing claims data is not as precise as that obtained by analyzing prospective clinical trial data due to possible errors in the coding of primary diagnoses and surgical modalities. Second, complications associated with LC surgical procedures were not assessed, which limits the validity of the prediction. Finally, the analysis did not examine outcome data, such as patient-reported quality of life and indirect costs incurred after discharge. However, given the robust magnitude of the effects and the statistical significance of the effects in this study, these limitations are unlikely to compromise the results.
Conclusions
This population-based study is the first to examine associations between volume and outcome in LC patients in Taiwan. Analysis using a hierarchical linear regression model and propensity score found an association between high-volume hospitals and surgeons and hospital treatment cost in LC patients. Moreover, the significant factors associated with hospital resource utilization for this procedure include age, gender, CCI score, hospital type, hospital volume, and surgeon volume. Additionally, analysis of the treatment strategies adopted at high-volume hospitals or by high-volume surgeons may improve overall hospital treatment cost.
References
Singla A, Simons JP, Carroll JE, Li Y, Ng SC, Tseng JF, Shah SA (2010) Hospital volume as a surrogate for laparoscopically assisted colectomy. Surg Endosc 24:662–669
Saad S, Paul A, Treckmann J, Tarabichi A, Nagelschmidt M, Arns W (2010) Laparoscopic live donor nephrectomy: are ten cases per year enough to reach the quality standards? A report from a single small-volume transplant center. Surg Endosc 24:594–600
Lehmann KS, Ritz JP, Wibmer A, Gellert K, Zornig C, Burghardt J, Büsing M, Runkel N, Kohlhaw K, Albrecht R, Kirchner TG, Arlt G, Mall JW, Butters M, Bulian DR, Bretschneider J, Holmer C, Buhr HJ (2010) The German registry for natural orifice translumenal endoscopic surgery: report of the first 551 patients. Ann Surg 252:263–270
Shi HY, Lee HH, Tsai MH, Chiu CC, Uen YH, Lee KT (2011) Long-term outcomes of laparoscopic cholecystectomy: a prospective piecewise linear regression analysis. Surg Endosc 25:2132–2140
Mercado MÁ, Franssen B, Dominguez I, Arriola-Cabrera JC, Ramírez-Del Val F, Elnecavé-Olaiz A, Arámburo-García R, García A (2011) Transition from a low- to a high-volume centre for bile duct repair: changes in technique and improved outcome. HPB (Oxford) 13:767–773
Csikesz NG, Singla A, Murphy MM, Tseng JF, Shah SA (2010) Surgeon volume metrics in laparoscopic cholecystectomy. Dig Dis Sci 55:2398–2405
Livingston EH, Cao J (2010) Procedure volume as a predictor of surgical outcomes. JAMA 304:95–97
D’Hoore W, Sicotte C, Tilquin C (1993) Risk adjustment in outcome assessment: the Charlson comorbidity index. Methods Inf Med 32:382–387
Marí-Dell’Olmo M, Martínez-Beneito MA, Borrell C, Zurriaga O, Nolasco A, Domínguez-Berjón MF (2011) Bayesian factor analysis to calculate a deprivation index and its uncertainty. Epidemiology 22:356–364
Hobbs BP, Carlin BP, Mandrekar SJ, Sargent DJ (2011) Hierarchical commensurate and power prior models for adaptive incorporation of historical information in clinical trials. Biometrics 67:1047–1056
Joffe MM, Rosenbaum PR (1999) Invited commentary: propensity scores. Am J Epidemiol 150:327–333
Rubin DB (1997) Estimating causal effects from large data sets using propensity scores. Ann Intern Med 127:757–763
Okrainec A, Ferri LE, Feldman LS, Fried GM (2011) Defining the learning curve in laparoscopic paraesophageal hernia repair: a CUSUM analysis. Surg Endosc 25:1083–1087
Kiran RP, Kirat HT, Ozturk E, Geisler DP, Remzi FH (2010) Does the learning curve during laparoscopic colectomy adversely affect costs? Surg Endosc 24:2718–2722
Bergamini C, Martellucci J, Tozzi F, Valeri A (2011) Complications in laparoscopic adrenalectomy: the value of experience. Surg Endosc 25:3845–3851
Harboe KM, Bardram L (2011) The quality of cholecystectomy in Denmark: outcome and risk factors for 20,307 patients from the national database. Surg Endosc 25:1630–1641
Panageas KS, Schrag D, Riedel E, Bach PB, Begg CB (2003) The effect of clustering of outcomes on the association of procedure volume and surgical outcomes. Ann Intern Med 139:658–665
Tiwari MM, Reynoso JF, High R, Tsang AW, Oleynikov D (2011) Safety, efficacy, and cost-effectiveness of common laparoscopic procedures. Surg Endosc 25:1127–1135
Jacobson KM, Hall Long K, McMurtry EK, Naessens JM, Rihal CS (2007) The economic burden of complications during percutaneous coronary intervention. Qual Saf Health Care 16:154–159
Lai CL, Fan CM, Liao PC, Tsai KC, Yang CY, Chu SH, Chien KL (2009) Impact of an audit program and other factors on door-to-balloon times in acute ST-elevation myocardial infarction patients destined for primary coronary intervention. Acad Emerg Med 16:333–342
Wang MJ, Lin SP (2010) Study on doctor shopping behavior: insight from patients with upper respiratory tract infection in Taiwan. Health Policy 94:61–67
Cheng SH, Song HY (2004) Physician performance information and consumer choice: a survey of subjects with the freedom to choose between doctors. Qual Saf Health Care 13:98–101
Disclosures
Hon-Yi Shi, King-Teh Lee, Chong-Chi Chiu, and Hao-Hsien Lee have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shi, HY., Lee, KT., Chiu, CC. et al. The volume–outcome relationship in laparoscopic cholecystectomy: a population-based study using propensity score matching. Surg Endosc 27, 3139–3145 (2013). https://doi.org/10.1007/s00464-013-2867-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-2867-x