Abstract
Background
The purpose of this study was to compare the postoperative inflammatory response and severity of pain between single-incision laparoscopic surgery (SILS) cholecystectomy and conventional laparoscopic cholecystectomy (LC).
Methods
Two groups of 20 patients were prospectively randomized to either conventional LC or SILS cholecystectomy. Serum interleukin-6 (IL-6) levels were assayed before surgery, at 4–6 h, and at 18–24 h after the procedure. Serum C-reactive protein (CRP) levels also were assayed at 18–24 h after surgery. Pain was measured at each of three time points after surgery using the visual analogue scale (VAS). The number of analgesia doses administered in the first 24 h after the procedure also was recorded and 30-day surgical outcomes were documented.
Results
The groups had equivalent body mass index (BMI), age, and comorbidity distribution. Peak IL-6 levels occurred 4–6 h after surgery, and the median level was 12.8 pg/ml in the LC and 8.9 pg/ml in the SILS group (p = 0.5). The median CRP level before discharge was 1.6 mg/dl in the LC and 1.9 mg/dl in the SILS group (p = 0.38). There was no difference in either analgesic use or pain intensity as measured by the VAS between the two groups (p = 0.72). The length of the surgical procedure was significantly longer in the SILS group (p < 0.001). No intraoperative complications occurred in either group.
Conclusions
Single-incision laparoscopic surgery does not significantly reduce systemic inflammatory response, postoperative pain, or analgesic use compared with LC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The introduction of laparoscopic surgery was an important milestone in the evolution of general surgery. This approach is now known to shorten recovery and attenuate the inflammatory response [1, 2] resulting from surgical procedures. More recently, natural orifice transluminal endoscopic surgery (NOTES) and single incision laparoscopic surgery (SILS) have been introduced as new surgical approaches that could further improve patient recovery and alleviate pain. What is still not clear, however, is whether these approaches add any benefit beyond aesthetics when compared with laparoscopic cholecystectomy (LC) [3]. To address some of these issues, we compared the inflammatory response, postoperative pain, and short-term surgical outcomes between SILS and conventional LC.
Materials and methods
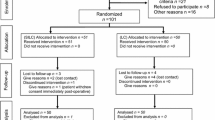
Patients and follow-up
Forty patients with symptomatic cholelithiasis, diagnosed based on clinical symptoms and confirmed with abdominal ultrasound scan, were randomly assigned to single-port cholecystectomy or LC from January 2010 to December 2010. Some of these patients also had an upper gastrointestinal endoscopy as part of the workup. Only patients with a body mass index (BMI) of 35 kg/m2 or less were included in the randomization. Intraoperatively, all patients had a thin-walled gallbladder with no adhesions or loose omental adhesions, which were bluntly dissected away from the gallbladder quite easily. All patients were followed for 30 days after surgery. The first follow-up visit was 7–10 days after the procedure, and a second follow-up visit was scheduled for 30 days after the operation. Any postoperative complications were diagnosed using either physical examination or standard diagnostic testing and were treated based on surgeon discretion using accepted standard methods of treatment. The trial was approved by local ethics committee, and informed consent was obtained from every patient before enrollment in the study.
Surgical technique
A conventional LC was performed with four ports as previously described [4]. A 10-mm port was placed at umbilicus and one at the subxiphoid position, whereas two 5-mm ports were placed in the right subcostal position. A 10-mm 30-degree scope was employed to establish the visual field.
In the SILS group, we used the SITRACC® device (EDLO, Rio Grande do Sul, Brazil), which contains one 10-mm and three 5-mm working ports. An angulated grasper and a folding coiled grasper for fundus retraction also were utilized in the procedure. A long, 7-mm, 30-degree scope was used. All other instruments were conventional laparoscopic implements.
The pneumoperitoneum was maintained at 12 mm Hg in both groups. An intraoperative cholangiogram is not performed routinely in our practice, and none were indicated in this series. No drains were placed in patients of either group.
Anesthetic and analgesic protocol
Anesthestic induction was achieved using propofol 2.5 mg/kg, remifentanil 0.25–1 μg/(kg min), and vecuronium 0.1 mg/kg. Anesthesia was maintained with sevoflorane 1–2 minimal alveolar concentration (MAC) with 50 % oxygen and 50 % air. The descurarization was done with atropine 0.02 mg/kg and neostigmine 0.04 mg/kg. The only antiemetics administered in the operating room were metoclopramide 10 mg and dexamethasone 10 mg. Further use of metoclopramide was on an as-needed basis in the postoperative period until discharge. Ondansetron was only administered if the patient had nausea after metoclopramide was used. At the completion of the procedure, 1 % lidocaine without epinephrine was used for local analgesia at a dose of 5 mg/kg, with 50 % injected in the umbilical incision and the rest distributed through other incisions in the LC group. The entire dose was injected in the umbilical incision in the SILS group. One hundred milligrams of ketoprofen and 30 mg/kg of dipirona were administered intravenously in the operating room at the end of procedure. A second dose of ketoprofen was administered 12 h after the first dose. Intravenous dipirona, at a dose of 30 mg/kg was administered according to patient request every 4 h until discharge home. Tramadol 50 mg intravenously, every 6 h, also was provided on an as-needed basis.
Analysis of inflammatory response
Blood was drawn for an interleukin-6 (IL-6) assay just before anesthetic induction, at 4–6 h postoperatively, and again at 18–24 h after the completion of the procedure. The blood was immediately centrifuged and the plasma frozen at −20 °C and stored for no more than 60 days. An Elecsys IL-6 assay kit (Roche Diagnostics®, Sao Paulo, Brazil) was used to measure plasma IL-6 levels. C-reactive protein (CRP) was assayed at 18–24 h after the procedure, before patient discharge using a Vitros 250 kit (Johnson & Johnson®, Sao Paulo, Brazil). The blood sample was processed without delay in the hospital’s central laboratory.
Pain measurement
The pain intensity was measured at 3 h, 6–8 h, and at 16–24 h after the completion of the procedure using the visual analogue scale (VAS) where values range from 0 (no pain) to 10 (worst pain ever experienced). In the perioperative setting, all patients were provided with the same anesthetic and analgesic protocol. During the postoperative period, analgesics were only administered after a patient requested them.
Statistical analysis
The Student’s t test was used to compare groups in terms of demographic and outcomes. The Mann–Whitney test was used for comparisons of IL-6 levels, CRP, and postoperative pain. A p value <0.05 was considered significant. SPSS version 17 software was utilized for the statistical analysis.
Results
There were 20 patients enrolled in each group. All patients completed follow-up at 30 days. The two groups were similar in regard to age, BMI, and comorbidities (Table 1). No intraoperative complications were observed, and there were no mortalities. The operative time was longer with SILS cholecystectomy than LC (92 ± 27.7 vs. 41.9 ± 14; p < 0.001). Two patients (10 %) in the SILS group needed extra ports placed during the operation to complete the procedure. The overall results did not differ when these patients were excluded from the analysis. One patient needed one 5-mm port, and another patient needed two 5-mm ports. In addition, instrument clashing precluded adequate exposure of the biliary pedicle in two other patients in the SILS group, so a transabdominal 2.0 nylon stitch was placed to retract the gallbladder fundus (puppeteer technique). One SILS patient had a surgical site infection, as did two patients in the conventional laparoscopic group. No other complications were observed at 30 days. The critical view was documented in all cases, and in all but one SILS case, the cystic artery was ligated before the cystic duct.
Interleukin-6 levels did not show a significant difference at any of the three time points between SILS and LC. The median preoperative IL-6 level was 2.3 pg/ml for SILS and 3.5 pg/ml for LC (p = 0.51; Table 2). At 4–6 h, it was 8.9 and 12.8 pg/ml (p = 0.5) for SILS and LC respectively and 8.2 and 5.1 pg/ml (p = 0.37) at 18–24 h after the procedure. IL-6 levels decreased faster in the laparoscopic group than in the SILS group (Table 2). CRP levels at discharge were 1.9 mg/dl in SILS and 1.6 mg/dl in the LC group (p = 0.38).
There was no significant difference in severity of pain as measured by the VAS at any of the time points. Three hours after the surgery, the mean scores were 3.5 for the SILS group and 4.3 for the LC group (p = 0.37). The scores 6–8 h after the procedures were 2.1 for the SILS group and 2.8 for the LC group (p = 0.4). At discharge, the scores for SILS and LC groups were 1.4 and 0.8, respectively (p = 0.21). The severity of pain decreases as time progresses (Table 3). Six patients in the single-port group and five patients in the laparoscopic group needed on-demand analgesic medication (p = 0.723). In total, 12 doses of analgesics were used in the SILS group, and 15 doses in the LC group. Tramadol was used in two patients who underwent SILS and two who underwent LC. Only one dose per patient was administered.
A 30-day follow-up, we observed three superficial wound infections: two in the LC and one in the SILS group. All patients were treated in an outpatient setting with wound dressing and oral antibiotics. No other complications were observed.
Discussion
In this study, the groups were similar according BMI, age, and comorbidity distribution. Peak IL-6 levels occurred 4–6 h after surgery with no differences noted at the median levels. The median CRP level before discharge was similar between the two groups. There was no difference in analgesic use or pain intensity as measured by the VAS, although the length of the surgical procedure was significantly longer in the SILS. No intraoperative complications transpired in either group.
The systemic inflammatory response to surgery is considered to be a consequence of tissue trauma [5], and this, in turn, influences surgical outcome [2]. The laparoscopic approach has been shown to attenuate the inflammatory response when compared with open surgery [1, 6, 7]. Clinically, this results in less pain and a faster recovery [8]. We found that the inflammatory response, as measured by serum IL-6 and CRP levels, was similar in both the single-port and laparoscopic groups. The peak of IL-6, as expected, occurred around 6 h after surgery, and then decreased at 24 h. Not only were the groups similar (Table 2), but the amount of variation of IL-6 was similar as well (data not shown). CRP level at 18–24 h also was similar in the two groups. Our results are in agreement with a recently published trial that investigated systemic inflammatory response after surgery [9]. In this study, McGregor et al. found no difference between the groups in IL-6 levels at 6 h after surgery; however, the investigators did not randomize patients, nor did they assay IL-6 at 24 h. Another interesting finding in our investigation is that there was a trend toward decreased IL-6, CRP, and pain at 24 h in the LC group compared with SILS group. It is not clear whether these findings occurred by chance, secondary to a longer operative time in the SILS group, or because of a larger surgical incision in the SILS group. As our experience with single-port surgery increases, the operative time will likely diminish [10] and greater differences between SILS and LC may become more apparent.
We used patient perception of pain as a surrogate clinical indicator of systemic inflammation. Patient reported pain was measured at three different time points after surgery using a VAS. We found no significant differences between the two groups of patients in terms of reported pain and the quantity of on-demand analgesics delivered was similar in both groups. The current literature on this particular topic is mixed. Authors have reported either equivalent [3, 11, 12], less [13, 14], or more pain [15, 16] after SILS. The only multicenter, randomized trial to date reports a similar pain scores in both groups, except on days 3 and 5 when the pain scores were higher in SILS group [17]. Even though some difference was noted, the average difference of pain score was less than 1 on a 10-point scale. On postoperative day 1, at 1 week, and at 2 weeks, no differences were observed. There also was no difference in pain medication use. However, there might be a limitation, because in this study the postoperative care was done at the surgeon’s discretion. Our results suggest that the differences of postoperative pain intensity do not seem to be of sufficient magnitude to tip the balance for or against SILS. The discrepancy between the studies is difficult to explain and could be attributable to differences in analgesic regimens, type 2 error, selection bias in some studies, lack of strict analgesic protocols, or because of differences related to the frequency of pain measurement between the protocols.
Most investigators have found that operative time for SILS is much longer than for LC [11–13, 15, 17, 18], which also was our experience. Most groups who find similar operative time between the procedures have reported a longer operative time for LC, as opposed to a shorter operative time for SILS [14]. This probably reflects the technical difficulty of the procedure during SILS, including difficulty with gallbladder retraction and exposure of Calot’s triangle. Consequently, because of these limitations the amount of time required to achieve the critical view was longer in the SILS group. An important lesson from our series is that the surgeon should not sacrifice obtaining the critical view of safety in order to record a faster procedure. When it is not technically possible to achieve the critical view with the single-port approach, more ports should be added for safety. Two patients (10 %) in our SILS group required additional ports to complete the procedure, and two patients required the “puppeteer” technique to achieve adequate exposure of Calot’s triangle. In one of our cases, an additional port was inserted due to difficulty exposing the biliary pedicle. After insertion, the procedure was completed without further struggle. Another patient required two additional ports. This patient was initially thought to have a thin walled gallbladder, but after the insertion of the single port and the manipulation of the gallbladder, the organ was found to be hydropic with dense omental adhesions. In our intention to follow protocol, these patients were analyzed in the single-port group. The decision to insert an extra port was based solely on the surgeon’s best judgment, and even when these patients were excluded, the results did not differ. The frequency of extra port placement during SILS in the literature ranges from 0 to 67 % [16, 18, 19], and such a wide range tends to reflect different thresholds among surgeons.
Perioperative and 30-day complications were similar in both groups. We had superficial wound infection in three cases, and these were treated on an outpatient basis with dressing changes and antibiotics. In a recent meta-analysis of seven prospective trials, Markar et al. [20] reported a 10.26 % complication rate for SILS and 8.89 % for LC. They also reported wound infections in 1.5 % of SILS patients and 2.2 % in LC group. In an intermediate report of a multicenter randomized trial [17], superficial wound complications were described more frequently in a SILS group compared with LC (10 % vs. 3 %), as well as trend to a higher incidence of incisional hernias (3.4 % in SILS vs. 1.3 % in LC group).
The main limitations of our study include the difference of surgeons experience between the conventional laparoscopic procedure and SILS and lack of a previous power analysis and sample size calculation. The lack of previous studies when this protocol was initiated precluded any sample size calculation. Both of these limitations are routinely seen when a new technique is evaluated, and because of the learning curve associated with SILS, we must be cautious about any definitive conclusion. Also, long-term complications were not addressed by this study. The frequency of events, such as incisional hernia and bile duct stricture, still needs to be evaluated by long-term trials. The main strengths of this study are the randomized design, strict postoperative protocol, and the measurement of all variables—clinical and inflammatory—in the same population.
Conclusions
In our prospective, randomized study of SILS versus LC, we found no significant differences in inflammatory response or pain between the two groups. This study also demonstrates that single-port surgery can be performed safely and without increased short-term surgical complications.
References
Glaser F, Sannwald GA, Buhr HJ, Kuntz C, Mayer H, Klee F, Herfarth C (1995) General stress response to conventional and laparoscopic cholecystectomy. Ann Surg 221(4):372–380
Biffl WL, Moore EE, Moore FA, Peterson VM (1996) Interleukin-6 in the injured patient. Marker of injury or mediator of inflammation? Ann Surg 224(5):647–664
Pfluke JM, Parker M, Stauffer JA, Paetau AA, Bowers SP, Asbun HJ, Smith CD (2011) Laparoscopic surgery performed through a single incision: a systematic review of the current literature. J Am Coll Surg 212(1):113–118
Spaw AT, Reddick EJ, Olsen DO (1991) Laparoscopic laser cholecystectomy: analysis of 500 procedures. Surg Laparosc Endosc 1(1):2–7
Lin E, Calvano SE, Lowry SF (2000) Inflammatory cytokines and cell response in surgery. Surgery 127(2):117–126
Vittimberga FJ Jr, Foley DP, Meyers WC, Callery MP (1998) Laparoscopic surgery and the systemic immune response. Ann Surg 227(3):326–334
Bruce DM, Smith M, Walker CB, Heys SD, Binnie NR, Gough DB, Broom J, Eremin O (1999) Minimal access surgery for cholelithiasis induces an attenuated acute phase response. Am J Surg 178(3):232–234
Kristiansson M, Saraste L, Soop M, Sundqvist KG, Thörne A (1999) Diminished interleukin-6 and C-reactive protein responses to laparoscopic versus open cholecystectomy. Acta Anaesthesiol Scand 43(2):146–152
McGregor CG, Sodergren MH, Aslanyan A, Wright VJ, Purkayastha S, Darzi A, Paraskeva P (2011) Evaluating systemic stress response in single port vs. multi-port laparoscopic cholecystectomy. J Gastrointest Surg 15(4):614–622
Solomon D, Bell RL, Duffy AJ, Roberts KE (2010) Single-port cholecystectomy: small scar, short learning curve. Surg Endosc 24(12):2954–2957
Marks J, Tacchino R, Roberts K, Onders R, Denoto G, Paraskeva P, Rivas H, Soper N, Rosemurgy A, Shah S (2011) Prospective randomized controlled trial of traditional laparoscopic cholecystectomy versus single-incision laparoscopic cholecystectomy: report of preliminary data. Am J Surg 201(3):369–372 discussion 372–373
Aprea G, Coppola Bottazzi E, Guida F, Masone S, Persico G (2011) Laparoendoscopic single site (LESS) versus classic video-laparoscopic cholecystectomy: a randomized prospective study. J Surg Res 166(2):e109–e112
Tsimoyiannis EC, Tsimogiannis KE, Pappas-Gogos G, Farantos C, Benetatos N, Mavridou P, Manataki A (2010) Different pain scores in single trans-umbilical incision laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc 24(8):1842–1848
Asakuma M, Hayashi M, Komeda K, Shimizu T, Hirokawa F, Miyamoto Y, Okuda J, Tanigawa N (2011) Impact of single-port cholecystectomy on postoperative pain. Br J Surg 98(7):991–995
Ma J, Cassera MA, Spaun GO, Hammill CW, Hansen PD, Aliabadi-Wahle S (2011) Randomized controlled trial comparing single-port laparoscopic cholecystectomy and four-port laparoscopic cholecystectomy. Ann Surg 254(1):22–27
Lai EC, Yang GP, Tang CN, Yih PC, Chan OC, Li MK (2011) Prospective randomized comparative study of single incision laparoscopic cholecystectomy versus conventional four-port laparoscopic cholecystectomy. Am J Surg 202(3):254–258
Phillips MS, Marks JM, Roberts K, Tacchino R, Onders R, Denoto G, Rivas H, Islam A, Soper N, Gecelter G, Rubach E, Paraskeva P, Shah S (2011) Intermediate results of a prospective randomized controlled trial of traditional four-port laparoscopic cholecystectomy versus single-incision laparoscopic cholecystectomy. Surg Endosc. doi:10.1007/s00464-011-2028-z
Fronza JS, Linn JG, Nagle AP, Soper NJ (2010) A single institution’s experience with single incision cholecystectomy compared to standard laparoscopic cholecystectomy. Surgery 148(4):731–734 discussion 734–736
Curcillo PG 2nd, Wu AS, Podolsky ER, Graybeal C, Katkhouda N, Saenz A, Dunham R, Fendley S, Neff M, Copper C, Bessler M, Gumbs AA, Norton M, Iannelli A, Mason R, Moazzez A, Cohen L, Mouhlas A, Poor A (2010) Single-port-access (SPA) cholecystectomy: a multi-institutional report of the first 297 cases. Surg Endosc 24(8):1854–1860
Markar SR, Karthikesalingam A, Thrumurthy S, Muirhead L, Kinross J, Paraskeva P (2011) Single-incision laparoscopic surgery (SILS) vs. conventional multiport cholecystectomy: systematic review and meta-analysis. Surg Endosc. doi:10.1007/s00464-011-2051-0
Acknowledgments
The authors thank Dr. Daltro Ibiapina and all the members of the Second Surgical Clinics who assisted with the process of admission and care of our patients and to the Department of Anesthesiology for complying with the study protocol. Special thanks are extended to Dr. Lucas Prata and Dr. Rafael Diniz who assisted with the elaboration of this protocol. And finally, thanks to Dr. Nathan Bronson for the kind review of this paper.
Disclosures
Drs. Renato A. Luna, Daniel B. Nogueira, Pablo S. Varela, Eduardo de O. Rodrigues Neto, Maria Júlia R. Norton, Luciana do Carmo B. Ribeiro, Agatha M. Peixoto, Yara L. de Mendonça, Isidro Bendet, Rossano A. Fiorelli, and James P. Dolan have no conflicts of interest or financial ties to disclose.
Funding
All single-port devices were provided without cost by EDLO S/A Produtos Médicos, the IL-6 assays were performed by Sergio Franco Medicina Diagnostica laboratory at no costs for the investigator, and all of the patients were treated under the Brazilian public health system.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Luna, R.A., Nogueira, D.B., Varela, P.S. et al. A prospective, randomized comparison of pain, inflammatory response, and short-term outcomes between single port and laparoscopic cholecystectomy. Surg Endosc 27, 1254–1259 (2013). https://doi.org/10.1007/s00464-012-2589-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2589-5