Abstract
Background
Laparoendoscopic single-site surgery (LESS) has emerged as a technique that uses a natural scar, the umbilicus, within which a multiple-entry portal is placed into a 3.0–4.0-cm single incision to perform operations. The objective of this study was to compare incision size, wound complications, and postoperative pain of LESS compared with those of laparoscopic cholecystectomy (LC).
Methods
A prospective randomized controlled study was conducted between January and June 2011 at two university hospitals in Rio de Janeiro, Brazil. Fifty-seven patients were randomly assigned to undergo laparoscopic or LESS cholecystectomy. Skin and aponeurosis wound sizes were recorded. A 10-point visual analog scale (VAS) was used to assess pain at postoperative hours 3 and 24. Healing and wound complications were assessed at follow-up.
Results
A total of 57 patients, 53 women and 4 men with a mean age of 48.7 years, were randomly assigned to undergo LESS (n = 28) or LC (n = 29). The mean length of the umbilical skin incision was 4.0 cm (range = 2.1–5.8) in LESS and 2.7 cm (1.5–5.1) in LC (p < .0001). The mean internal aponeurosis diameter was 3.5 cm (2.0–5.5) in LESS and 2.3 cm (1.2–3.5) in LC (p < .0001). The mean operative time was 60.3 min (32–128) for LESS and 51.3 min (25–120) for LC (p = 0.11). Gallbladder perforation at detachment occurred in 15.69 % of the LESS cases and in 5.88 % of the LC cases (p = 0.028). The mean VAS score for pain at hour 3 was 2.0 points (0–7) for the LESS group and 4.0 (0–10) for the LC group (p = 0.07), and at postoperative hour 24 it was 0.3 points (0–6) for LESS and 2.3 (0–10) for LC (p = 0.03). There were no significant differences in wound complications. Incisional hernias were not found in either group.
Conclusions
The LESS single-port (SP) operations demand a bigger incision than LC surgery. However, there were no differences in healing, wound infections, and hernia development. We found a tendency of less postoperative pain associated with LESS/SP than with LC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic cholecystectomy (LC) is the gold standard for treating gallbladder lithiasis, which is currently the most common indication for elective surgery. Familiarity with video laparoscopic (VL) procedures, staff training, and the development of new materials have all contributed to the rapid increase in the number of these operations in recent years. Nonetheless, continued efforts to minimize surgical impact, morbidity, and complications include the development of even less invasive procedures that are comparable to LC that involve just one or no incisions without a loss in operability [1, 2].
Laparoendoscopic single-site surgery (LESS), also called single-port (SP) surgery [3], has emerged in recent years as a technique that uses a natural scar, the umbilicus, and a usual surgical access site, the skin [4]. This technique involves the use of a portal with multiple entry sites which is inserted into a single transumbilical incision that is approximately 3.0–4.0 cm in length. Into the entry sites of the portal are inserted the flexible or adapted VL instruments. The proposed clinical advantages of LESS cholecystectomy include less postoperative pain, faster recovery, an excellent cosmetic result, a single site of pain (which reduces the potential for infection) [5], and very low morbidity [6–16].
The objective of this study was to compare incision size in the skin and aponeurosis and wound complications such as seromas, infections, and hernia development in patients who underwent LESS versus patients who underwent video LC. We also studied postoperative pain associated with LESS and with traditional LC.
Methods
This prospective randomized controlled study was conducted between January and June 2011 at the Clementino Fraga Filho University Hospital and Gaffrée Guinle University Hospital in Rio de Janeiro, Brazil. The enrolled patients (n = 57) were randomly assigned to the LC or the LESS cholecystectomy group. All patients were >18 years old with symptomatic or asymptomatic cholelithiasis and gallbladder polyps larger than 1 cm. Postoperative analgesia was the same for both groups: routine administration of dipyrone and ketorolac tromethamine, with tramadol hydrochloride for additional analgesia upon request. Patients who showed acute cholecystitis, jaundice, and pancreatitis at the preoperative evaluation and who had a scleroatrophic gallbladder as shown by ultrasound (USG) were excluded from the study. The patients were distributed between the two groups in a randomized manner, and to confirm the similarity of the groups, they were analyzed by body mass index (BMI), sex, comorbid conditions, previous abdominal surgery, cholelithiasis time, and hematological and biochemical parameters.
This study was approved by the institutional review board of Clementino Fraga Filho University Hospital (UFRJ) (registration No. 196/96, July 2010). Each included patient signed an informed consent form.
The following surgical data were recorded for each patient: type of incision, skin and aponeurosis wound sizes, and detailed surgical time course. The wound measurements were taken at the end of the operation. The skin and aponeurosis sizes were measured using a sterilized caliper to measure the distance between two (vertical) opposing sides of incision. A standard 10-point visual analog scale (VAS) was used to measure pain at postoperative hours 3 and 24 [17]. Healing and wound complications such as infections, seromas, and hernias were assessed at follow-up.
Surgical technique
LESS surgeries were performed using SP/LESS portals that were introduced into the transumbilical position using open access. We used the SITRACC® portal (Edlo S.A., Curitiba, Brazil) [18, 19], the SILS™ Port (Covidien, Mansfield, MA, USA), and the X-cone® device (Karl Storz Endoskope, Tuttlingen, Germany). All procedures were SP surgeries that were performed the same way using 10-mm 30° optical, curved forceps in the left hand to the gallbladder infundibulum, and regular 5-mm instruments (including clip applier, hook, and Maryland cannula suction) in the right hand, with the bottom of the gallbladder retracted through the intercostal area, using a nylon suture. This configuration was comfortable for the surgeon and very similar to that used in conventional laparoscopy (Fig. 1). The LC was performed using traditional 10- and 5-mm four-trocar surgery, also using open laparoscopic access; the Veress needle was not used.
Statistical analysis
Data from the two groups were compared using statistical analysis. The mean or median was calculated for quantitative variables. Student’s t test was used to compare means. The χ2 test or Fisher’s exact test was used to analyze qualitative variables. A p value < 0.05 was considered statistically significant.
Results
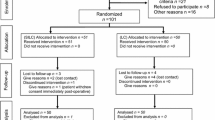
A total of 62 patients were selected for elective cholecystectomy; 5 patients were excluded from analysis because of acute cholecystitis: 3 patients in the LESS group and 2 in the LC group. Of the 57 patients included in the study, 53 were women and 4 were men with a mean age of 48.7 years (range = 18–78 years). They were randomly assigned to undergo LESS (n = 28) or LC (n = 29) (Fig. 2). The demographic and preoperative characteristics of the patients are given in Table 1. There were no statistically significant differences in BMI, sex distribution, comorbid conditions, previous abdominal surgery, ASA grade, or cholelithiasis time. Hemoglobin, hematocrit, and biochemical parameters were also similar between the two groups (Table 2).
In the 28 LESS surgeries, we used the SITRACC portal in 8, the SILS™ Port in 8, and the X-cone® device in 12. A vertical transumbilical incision was used in all surgeries. The mean length of umbilical skin incision (USI) was 4.0 cm (range = 2.1–5.8) in the LESS group and 2.7 cm (range = 1.5–5.1) in the LC group (p < 0.0001). The mean internal aponeurosis diameter (IAD) was 3.5 cm (range = 2.0–5.5) in the LESS group and 2.3 cm (range = 1.2–3.5) in the LC group (p < 0.0001) (Fig. 3). When the SP devices were compared, there was a significant difference between the X-cone® and SITRACC® devices in terms of the USI (p = 0.0047) and the IAD (p = 0.003) (Table 3).
The mean operative time (OPT) was 60.3 min (range = 32–128) in the LESS group and 51.3 min (range = 25–120) in the LC group (p = 0.11). The mean effective surgical time (EFT), excluding the portal introduction and wound closure time, was 34.9 min in the LESS group and 29.08 min in the LC group (p = 0.19). The mean gallbladder detachment time (Dt) (after ligation and section of the artery and cystic duct) was 8.3 min in the LESS group and 7.23 min in the LC group (p = 0.85). The mean closure time (CST) (time to close the aponeurosis and skin incisions) was 8.21 min in the LESS group and 9.14 min in the LC group (p = 0.083). There was no conversion to laparotomy, placement of drains, or ICU stay. There was one case of postoperative pneumonia in the LESS series.
Gallbladder perforation at detachment occurred in 5.88 % of the LC cases and in 15.69 % of the LESS cases (p = 0.028). The mean time until food intake was 6 h in both groups. All patients were discharged within 24 h. There was no statistical difference in the use of additional analgesia, which was requested by 7.40 % of the patients in the LESS group and by 9.52 % of the patients in the LC group. The mean VAS score for pain at postoperative hour 3 was 2.0 (range = 0–7) in the LESS group and 4.0 (range = 0–10) in the LC group (p = 0.07). The mean VAS score for pain at postoperative hour 24 was 0.3 (range = 0–6) in the LESS group and 2.3 (range = 0–10) in the LC group (p = 0.03) (Fig. 4). The mean follow-up time was 5.92 months for both groups. There were no statistically significant differences in terms of wound healing, i.e., stitch removal, or development of wound infections for both groups; (p = ns) or seromas (p = 0.32). At the end of follow-up, no incisional hernias had been diagnosed in any of the patients.
Discussion
After the initial enthusiasm about procedures that utilize incisions through natural orifices (NOTES surgery), surgeons sought to reach a consensus on minimally invasive procedures that leave virtually no scarring and traditional operative access through the skin. The umbilical scar is an obvious choice as a surgical site. For this study we used the nomenclature adopted by the LESSCAR consortium, i.e., LESS.
A new surgical procedure that involves new concepts and claims to have advantages over traditional LC must be evaluated objectively. Many questions arise: Is this operation easier? Is it safe? Can it be used in all patients? Is it less expensive? Does it have more complications or cause more pain? This randomized controlled trial (RCT) aimed to answer these questions.
For the LESS group, we used three different portals, the SITRACC®, the SILS™ Port, and the X-cone® device. Using three devices allowed us to evaluate not only the devices but LESS surgery. The different portals allowed us to compare disposable versus reusable devices and flexible versus semirigid devices. Flexible SPs provide a wider opening that facilitates triangulation. The ergonomics are difficult for SP procedures due to the small size of the access site: having all instruments in the same opening leads to friction between forceps, the optical device, and the SP. Deformable material, which is used in the SILS™ and SITRACC® devices, helps decrease the friction and allows the portal to adapt to different incision sizes. However, the deformation characteristic also allows the pneumoperitoneum to vent and can cause the portal to become detached. Semirigid but self-expanding devices, such as the X-cone®, can be inserted in the smallest incisions and they attach very well to the abdominal wall. Their disadvantages include a cramped incision site and increased friction. Nevertheless, these differences between the devices did not result in statistical differences in operative time between the SPs or between the LC and LESS groups.
The lack of difference in OPT between the LC and LESS groups may give the wrong impression that these two methods are both consistently easy to perform. On the contrary, there was a learning curve of almost 20 patients before starting the study as the surgeons mastered the skills and, especially, standardized the method. Other studies also report a learning curve, which can involve five to ten operations [20, 21]. After mastery was achieved, the surgeries were similar in the two groups, and almost the same surgical instruments were used for both procedures. New items included a curved Maryland and grasper forceps, a 5-mm clip applier, and the X-cone® device. All other equipment were standard laparoscopic instruments. The sole extraordinary cost was that of the SP disposable device (when one is used). Such devices are similar in cost to that of disposable trocars used in regular LC.
Two cases at the beginning of the series required the use of additional trocars. In these two operations, we were surprised by scleroatrophic cholecystitis and by a hydropic gallbladder. These cases were excluded from the study.
The choice of a vertical transumbilical incision allowed for a longer incision. The umbilicus has an inverted cone shape that when incised all the way, easily allows a 4.0–5.0-cm-long incision. Furthermore, this longer incision enables rapid and effortless removal of the gallbladder and synthesis of the aponeurosis. After healing, an excellent cosmetic result was achieved.
It is important to note that the measured means of the USIs and the IADs were significantly larger in the LESS group than in the LC group. One can argue that this would increase the risk of immediate and late wound complications. However, there was a low incidence of seroma (8 % for LESS and 12 % for LC), wound infection (2 % for both methods), and no hernias. In the literature, wound complications vary from 2 to 10 % [10, 13, 14, 22–24]. There is a possibility that the present study was too small to detect a difference in complications. In this study the wound measurements were taken at the end of surgery because the final incision size depends of the size and amount of calculi in the gallbladder. At the end of LC surgery it is common to have the gallbladder and calculus stuck at the wound and to have to increase the incision and dirty the operating field. Such increases in incision size explain why even the use of a 10-mm trocar at the umbilicus results in a mean incision length of 2.3–2.7 cm. In SP, the piece is retrieved inside the portal without difficulty and with less contamination.
We should address the questions posed earlier, i.e., is LESS surgery easier? Is it safe? Can it be used in all patients? At first, the LESS/SP operation does not seem easier as when one first learns how to perform laparoscopic surgery. However, after training and experience, both methods are very similar. There are no data that challenge the safety of the procedure [10, 12, 14, 20–23, 25–30, 32, 33]. A systematic review of 24 studies conducted by Allemann et al. [2] found that 15 of the studies provided safety information. All concluded that SP is safe. In our study with randomization, the cohorts were very similar, but the BMI in the SP series was greater than that in the LC group. In the SP group, there was a patient with a BMI of 43.75. There were no differences between the groups with respect to previous abdominal surgery. Our data are supported by that from several earlier studies which suggested that a high BMI is not a limiting factor for LESS surgery [10, 14, 20, 22, 31–33]. This study did not include urgent or emergency operations, and further study is needed to determine whether LESS is appropriate in these situations.
Comparing VAS pain scores at postoperative hours 3 and 24, there was a tendency toward less pain for the LESS/SP patients compared to the LC patients at both time points (p = 0.07 and p = 0.03, respectively). This is important because this kind of operation is minimally invasive, with the idea that the fewer the incisions, the less aggressive the approach and possibly less postoperative pain. In agreement with the results of Asakuma et al. [34], our data suggested that despite the larger size of the single incision, there was less pain for the LESS/SP patients.
Conclusions
The LESS/SP operation demands a bigger incision than that in LC surgery. However, there were no differences in healing, wound infections, and hernia development. There was a tendency of less postoperative pain associated with LESS/SP than with traditional LC and there are no data that challenge the safety of the LESS/SP procedure.
References
Ma J, Cassera MA, Spaun GO, Hammill CW, Hansen PD, Aliabadi-Wahle S (2011) Randomized controlled trial comparing single-port laparoscopic cholecystectomy and four-port laparoscopic cholecystectomy. Ann Surg 1:22–27
Allemann P, Schafer M, Demartines N (2010) Critical appraisal of single port access cholecystectomy. Br J Surg 97:1476–1480
Gill IS, Advincula AP, Aron M et al (2010) Consensus statement of the consortium for laparoendoscopic single-site surgery. Surg Endosc 24:762–768
Canes D, Desai MM, Aron M et al (2008) Transumbilical single-port surgery: evolution and current status. Eur Urol 54(5):1020–1029
Chuang SC, Lee KT, Chang WT et al (2004) Risk factors for wound infection after cholecystectomy. J Formos Med Assoc 103(8):607–612
Gill IS, Canes D, Aron M, Haber GP, Goldfarb DA, Flechner S, Desai MR, Kaouk JH, Desai MM (2008) Single port transumbilical (E-NOTES) donor nephrectomy. J Urol 180(2):637–641 discussion 641
Msezane LP, Mushtaq I, Gundeti MS (2009) An update on experience with the single-instrument port laparoscopic nephrectomy. BJU Int 103(10):1406–1408 discussion 1408–1409
Aron M, Canes D, Desai MM, Haber GP, Kaouk JH, Gill IS (2009) Transumbilical single-port laparoscopic partial nephrectomy. BJU Int 103(4):516–521
Bresadola F, Pasqualucci A, Donini A et al (1999) Elective transumbilical compared with standard laparoscopic cholecystectomy. Eur J Surg 165(1):29–34
Tacchino R, Greco F, Matera D (2009) Single-incision laparoscopic cholecystectomy: surgery without a visible scar. Surg Endosc 23(4):896–899
Cuesta MA, Berends F, Veenhof AA (2008) The “invisible cholecystectomy”: a transumbilical laparoscopic operation without a scar. Surg Endosc 22(5):1211–1213
Rao PP, Bhagwat SM, Rane A (2008) The feasibility of single port laparoscopic cholecystectomy: a pilot study of 20 cases. HPB (Oxford) 10(5):336–340
Merchant AM, Cook MW, White BC et al (2009) Transumbilical Gelport access technique for performing single incision laparoscopic surgery (SILS). J Gastrointest Surg 13(1):159–162
Romanelli JR, Roshek TB 3rd, Lynn DC, Earle DB (2009) Single-port laparoscopic cholecystectomy: initial experience. Surg Endosc 24(6):1374–1379
Gumbs AA, Milone L, Sinha P, Bessler M (2009) Totally transumbilical laparoscopic cholecystectomy. J Gastrointest Surg 13(3):533–534
Palanivelu C, Jani K, Maheshkumar GS (2007) Single-center experience of laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A 17(5):608–614
Aitken RC (1969) Measurement of feelings using visual analogue scales. Proc R Soc Med 62:989–993
Martins MVDC, Skinovsky J, Coelho DE (2009) Laparoscopic cholecystectomy by single trocar access (SITRACC®) - A new option. Rev Col Bras Cir 36(2):177–179
Martins MVDC, Skinovsky J, Coelho DE, Torres MF (2008) SITRACC - single trocar access: a new device for a new surgical approach. Bras J Video-Sur 1(2):061–063
Hodgett SE, Hernandez JM, Morton CA, Ross SB, Albrink M, Rosemurgy AS (2009) Laparoendoscopic single site (LESS) cholecystectomy. J Gastrointest Surg 13:188–192
Erbella J Jr, Bunch GM (2010) Single-incision laparoscopic cholecystectomy: the first 100 outpatients. Surg Endosc 24:1958–1961
Curcillo PG II, Wu AS, Podolsky ER, Graybeal C, Katkhouda N, Saenz A et al (2010) Single-port-access (SPA) cholecystectomy: a multi-institutional report of the first 297 cases. Surg Endosc 24:1854–1860
Roberts KE, Solomon D, Duffy AJ, Bell RL (2001) Single-incision laparoscopic cholecystectomy: a surgeon’s initial experience with 56 consecutive cases and a review of the literature. J Gastrointest Surg 14:506–510
Kuon Lee S, You YK, Park JH, Kim HJ, Lee KK, Kim DG (2009) Single-port transumbilical laparoscopic cholecystectomy: a preliminary study in 37 patients with gallbladder disease. J Laparoendosc Adv Surg Tech A 19:495–499
Rivas H, Varela E, Scott D (2009) Single-incision laparoscopic cholecystectomy: initial evaluation of a large series of patients. Surg Endosc 24:1403–1412
Hu H, Zhu J, Wang W, Huang A (2010) Optimized transumbilical endoscopic cholecystectomy: a randomized comparison of two procedures. Surg Endosc 24:1080–1084
Hodgett SE, Hernandez JM, Morton CA, Ross SB, Albrink M, Rosemurgy AS (2009) Laparoendoscopic single site (LESS) cholecystectomy. J Gastrointest Surg 13:188–192
Vidal O, Valentini M, Espert JJ, Ginesta C, Jimeno J, Martinez A et al (2009) Laparoendoscopic single-site cholecystectomy: a safe and reproducible alternative. J Laparoendosc Adv Surg Tech A 19:599–602
Chow A, Purkayastha S, Paraskeva P (2009) Appendicectomy and cholecystectomy using single-incision laparoscopic surgery (SILS): the first UK experience. Surg Innov 16:211–217
Rothenberg SS, Shipman K, Yoder S (2009) Experience with modified single-port laparoscopic procedures in children. J Laparoendosc Adv Surg Tech A 19:695–698
Philipp SR, Miedema BW, Thaler K (2009) Single-incision laparoscopic cholecystectomy using conventional instruments: early experience in comparison with the gold standard. J Am Coll Surg 209:632–637
Hong TH, You YK, Lee KH (2009) Transumbilical single-port laparoscopic cholecystectomy: scarless cholecystectomy. Surg Endosc 23:1393–1397
Bucher P, Pugin F, Morel P (2010) From single-port access to laparoendoscopic single-site cholecystectomy. Surg Endosc 24:234–235
Asakuma M, Hayashi M et al (2011) Impact of single-port cholecystectomy on postoperative pain. Br J Surg 98(7):991–995
Disclosures
Dr. Fernando Athayde Veloso Madureira, Dr. José Eduardo Ferreira Manso, Dr. Delta Madureira Filho, and Dr. Antonio Carlos Garrido Iglesias have no conflicts of interest or any financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Madureira, F.A.V., Manso, J.E.F., Madureira Fo, D. et al. Randomized clinical study for assessment of incision characteristics and pain associated with LESS versus laparoscopic cholecystectomy. Surg Endosc 27, 1009–1015 (2013). https://doi.org/10.1007/s00464-012-2556-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2556-1