Abstract
Background
Symptomatic airway obstructions are common with endobronchial exophytic tumors and may result in lethal complications. Recently, a cryorecanalization procedure has emerged that plays a role in the immediate management of airway obstruction. This study was conducted to investigate the value of cryorecanalization for the immediate management of endobronchial obstructive pathology and to determine the factors that affect the success of the procedure.
Methods
We analyzed 40 patients with symptoms of airway obstruction who were admitted to our hospital from 2006 to 2010. Patients with exophytic stenosis due to primary bronchial or metastatic neoplasms who underwent cryorecanalization procedures were included. Patients were excluded if they had involvement of a major artery near the site of the intervention. The procedure was not performed on patients with coagulation abnormalities or thrombocyte count and aggregation problems. The data were collected retrospectively.
Results
Successful cryorecanalization was achieved in 72.5 % of patients. We found that the success rate was mainly related to the presence of the distal involvement and the older age of obstruction. Restenosis rate was 12.8 %. The mean survival time after the cryorecanalization procedure was 11 ± 12.7 months. No complications occurred in 14 patients. No severe bleeding was observed for any patients, and moderate hemorrhaging occurred in ten patients, which was stopped with an argon plasma coagulator. We experienced no intraoperative mortality.
Conclusions
Cryorecanalization is a successful and safe intervention for the immediate management of endobronchial stenosis. Appropriate patient selection and high success rates should be achieved after careful radiological assessments and with early management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Airway obstruction is commonly observed with endobronchial exophytic tumors. Up to 30 % of lung cancers cause obstructions at the level of the trachea and main bronchi [1]. The most common manifestations of these obstructions are dyspnea, cough, and hemoptysis [2], and they may result in lethal complications, such as respiratory failure, atelectasis, and postobstructive pneumonia. With regard to treatment, many interventional bronchoscopists prefer laser, electrocautery, argon plasma coagulation, mechanical recanalization, and stents because of their immediate effects [3].
Endobronchial cryotherapy is used to treat malignant airway tumors, but conventional usage is limited to the palliation of noncritical endobronchial exophytic lesions and early lung cancers and for the removal of foreign bodies and clots [4]. In addition, 8–10 days are required for a complete therapeutic effect [5]. Clean-up bronchoscopy is usually performed. Recently, a new technique, cryorecanalization, has emerged for immediate debulking of exophytic endobronchial tumors [2, 6, 7]. In this technique, a bronchoscopist retracts frozen tissue at the tip of the probe with a bronchoscope, resulting in immediate tumor removal and recanalization of the airway lumen. This technique seems to be feasible and has many advantages, including its use of flexible probes, immediate efficacy, and low risk of complications. The technique is easy to learn and has a low cost compared with other endobronchial treatment modalities [7]. This study was conducted to investigate the efficacy and safety of cryorecanalization for the immediate management of endobronchial obstructive pathology.
Materials and methods
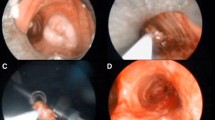
We analyzed 40 patients with symptoms of airway obstruction who were admitted to our hospital from 2006 to 2010. Patients with endoluminal protrusions of primary bronchial or metastatic neoplasms were included. The data were collected retrospectively. In all patients, computed tomography of the thorax was performed, and virtual bronchoscopic images were obtained (Fig. 1). Anatomic location, endobronchial length, infiltrative characteristics of obstructive lesions, and involvement of the distal bronchial tree were assessed before the procedures. Distal bronchial involvement was described as external compression and/or submucosal infiltration of a postobstructive bronchial segment (Figs. 2, 3). Endobronchial length was defined as the length of the exophytic portion. All patients had preoperative histological diagnoses. Disease stages were determined preoperatively. The age of tumor obstruction was defined as the time between the beginning of the obstruction and the day of the intervention. The beginning of the obstruction was determined either as the start of symptoms or when radiologic–bronchoscopic proof was obtained.
We conducted the procedures with patients randomly assigned to one of two different intubation techniques. One included general anesthesia with intravenous atracurium besylate and propofol. We intubated these patients with a rigid bronchoscope (Wolfe) and used a rigid cryorecanalization probe (53 cm in length, 2.5 mm in diameter, ERBE, Medizintechnik GmbH, Tübingen, Germany) for proximal lesions. For more distal lesions, a fiberoptic bronchoscope (Olympus, Japan) and flexible cryorecanalization probe (90 cm in length, 2.4 mm in diameter, ERBE, Medizintechnik GmbH, Tübingen, Germany) were introduced through the lumen of a rigid bronchoscope. The second technique was deep sedation with intravenous midazolam and propofol. We intubated these patients with a 7.5-mm bronchoflex tube (Rüsch, Germany) and used a fiberoptic bronchoscope and flexible cryorecanalization probe. The procedures were performed with continuous oxygen supplied at 6–12 L/min at all times.
The cryorecanalization procedure has been described elsewhere [2, 7]. A successful intervention was defined as reduced airway obstruction leading to an improvement in the patient’s general condition that was associated with symptom relief. Failure was defined when the primary condition of the intervention could not be reached.
The most common complications of interventional techniques were bleeding and bronchial wall damage. We classified bleeding as mild, moderate, or severe [2]. Mild hemorrhagia was defined as bleeding that could be controlled with a cold 0.9 % NaCl solution (2–4 °C) or epinephrine solution (1 mg/10 ml saline water). Moderate hemorrhagia was defined as bleeding that could be controlled with argon plasma coagulation. Severe hemorrhagia was defined as bleeding that required additional treatments (transfusion of red blood cells, fresh-frozen plasma, or coagulation factors), vasopressor support, or a rescue operation.
Patients with significant vascular involvement adjacent to the site of the intervention, obstructions due purely to external compression of the surrounding tumor, and involvement of the posterior membranous walls of the bronchi (because they do not contain cryoresistant cartilage tissue) were excluded. The procedure was not performed on patients with coagulation abnormalities or thrombocyte count and aggregation problems.
All patients were followed in an intensive care unit after the interventions. Posteroanterior chest roentgenograms were taken before, just after, and every seventh day after the interventions (Fig. 4). All patients received chemotherapy and/or radiotherapy regimens that were appropriate for their cancer stages according to current lung cancer guidelines. We calculated the survival rates of patients by measuring the time from the intervention to the death of the patient or the time of retrospective data collection.
Statistical analysis was performed using SPSS 11.5 for Windows. Results of numerical data are presented as a mean ± standard deviation. Fisher’s exact test or chi-square test was used to statistically test whether there was any relationship between two categorical variables. A p value <0.05 was considered statistically significant.
This study has been approved by the local ethics committee. Informed consent was obtained from all patients.
Results
The mean patient age was 56.3 ± 11 years. Thirty patients were male, and ten were female. Descriptive characteristics of the obstructive lesions are summarised in Table 1. The mean operation time was 60.3 ± 20.1 minutes. The mean tumor length was 2.1 ± 0.6 cm. The mean duration of tumor obstruction was 5.5 ± 2.5 weeks.
The overall procedure success rate was 72.5 %. The cryorecanalization procedure failed in 11 patients. We summarized the factors affecting the success of the cryorecanalization procedure in Table 2. We detected no correlation between the success rate and histopathology, stage, anatomical location, or degree of obstruction.
The mean survival time after the cryorecanalization procedure was 11 ± 12.7 months. We continue to follow nine patients who have a mean survival time of 21.2 ± 4.4 months.
A summary of complications is listed in Table 3. No complications occurred in 14 patients. No severe bleeding was detected for any patient during the procedure. Mild hemorrhagia, which was bleeding that could be relieved by a bronchial cold water wash, was observed in 15 patients. Moderate hemorrhagia that required management with argon plasma coagulation occurred in ten patients, and intraoperative hypoxia and carbon dioxide retention occurred in one other patient. We experienced no perioperative mortality.
We had 12 patients with preoperative diagnoses of unclassified non-small cell carcinoma. With the larger tissue specimens obtained by cryorecanalization, eight were diagnosed with squamous cell carcinoma and two with adenocarcinoma. Two specimens remained unclassified.
Discussion
Symptomatic airway obstructions are life-threatening complications of bronchial neoplasms and require immediate management. Obstructions are caused by endobronchial exophytic growths, external compression of the airway, or both [3]. The immediate effects of laser, electrocautery, and argon plasma coagulation techniques are effective, especially for exophytic tumors. Bronchial stents are preferable for obstructions due to external compression. However, cryotherapy, brachytherapy, and photodynamic therapy are not considered therapeutic options for symptomatic airway obstructions, because their actions are delayed [5]. Recently, cryorecanalization procedures have been used to manage obstructive endobronchial masses. We performed this technique in our patients with symptomatic airway obstructions and present our retrospectively obtained results.
The success rates of an Nd-YAG laser are reported to be 50–80 % [1]. Reichle et al. [8] reported success rates of 67% with Argon plasma coagulator (APC). In two previous studies [2, 7], the success rates of cryorecanalization were found to be 83 and 91 %, respectively. Our success rate was 72.5 % and was not related to histopathology, stage, anatomical location, or degree of obstruction. We found that the success rate was mainly related to the involvement of postobstructive bronchial segments and the duration of tumor obstruction. Intervention usually fails when tumor closure extends, and the distal respiratory tract cannot be reached [7]. In all successful operations in our study, distal involvement of the bronchial tree was absent. When it was present, the intervention definitely failed. We did not perform a patient selection test before the intervention to determine the ones likely to be reopened, avoiding a bias and also leading to diminished success rates. With a careful preoperative assessment, appropriate selection could be achieved (Fig. 5). Virtual bronchoscopy and thin-slice computed tomography are excellent guides for patient selection [7]. Also, distal bronchial involvement can be reliably assessed with radial probe endobronchial ultrasound equipped with Doppler function in cases with subtotal obstruction.
Types of malignant airway obstruction with a primary exophytic compound. Bronchial mucosa is expressed with red colour and the tumoral tissue with orange. Note the bronchial mucosa distal to the exophytic tumoral obstruction. Distal involvement is absent in type A. Distal bronchial mucosa seems to be normal. In type B, distal bronchial lumen is compressed externally by the tumor. In type C, exophytic obstructing tumor continues submucosally through the distal bronchus. Proper bronchial tree could not be achieved both in type B and C, we mentioned this situation as the distal involvement (Color figure online)
It is said to be easier to reopen tumor obstructions that are 4–6 weeks old [2]. Most of our failed interventions were performed on obstructions that were older than 6 weeks. The risk of a failed intervention is increased 280-fold for older obstructions. Therefore, we conclude that pulmonary specialists and oncologists should be aware of the efficacy of early management. It must be noted that 10 patients of 11 unsuccessful interventions had both older obstruction and distal bronchial involvement.
Restenosis rate after 29 successful interventions was found to be 12.8 %. Mean time to restenosis was 20 (range, 4–104) weeks. Reported relapse rates of cryotherapy are 24.8–28 % within a follow-up period of 2–45 months [7, 9]. Airway patency after 6 weeks in the patients without stenting was 0 % after mechanical debridement, 60 % after laser resection, 72 % after APC, 72 % after combined mechanical, and laser resection and 70 % after combined AP-C and mechanical debridement [10]. Cryorecanalization is related to improved restenosis rates.
The majority of our patients had epidermoid carcinomas. These cancers primarily involve the central bronchial tree and commonly cause airway obstruction. High-stage neoplasms of the bronchial tree frequently lead to bronchial obstruction, and patients with symptomatic airway obstruction are at risk of death due to respiratory failure. With cryorecanalization, the airway passage is immediately restored, and early deaths are successfully avoided. In this study, we reached a mean survival rate of eleven months after performing cryorecanalization. Note that cryorecanalization may provide an appropriate treatment option to a patient with a life-threatening airway obstruction and risk of early death.
Other therapeutic options that have immediate effects (argon plasma coagulation, laser, and electrocautery) have significant rates of severe complications, including bleeding, fire, airway perforation, and stenosis [4]. The oxygen supply must be stopped while shooting to avoid the risk of a fire, resulting in hypoxia. Cryotherapy, however, is a procedure that is easy to learn, relatively safe, and cheap [4, 7]. The oxygen supply does not need to be stopped (except the period that APC used to control bleeding), and there is a nearly 0 % risk of bronchial wall perforation. In addition, it is very useful for the ingrowth of stents. Cryotherapy also increases the efficacy of chemotherapy and radiotherapy [5, 11].We did not experience any severe hemorrhages or bronchial wall perforations in our 40 interventions. Moderate hemorrhage was observed in ten patients and was easily stopped with argon plasma coagulation.
Using a cryorecanalization probe, the airway lumen could be restored by removing a large fragment of tissue. This removal provides a chance to obtain a proper histopathological diagnosis [12, 13]. Cryoprobes have increased diagnostic performance for endobronchial lesions compared with forceps biopsies. They also can be used to obtain larger transbronchial lung biopsies with high histological quality [14]. We had 12 patients diagnosed with non-small cell carcinoma by using pathologic specimens obtained with bronchoscopic forceps. After evaluating large cryobiopsies, we obtained diagnoses of squamous cell carcinoma in eight and adenocarcinoma in two. Recently, because therapeutic agents with differential activities or limited indications have emerged, the proper subtyping of non-small cell carcinoma has gained special importance [15].
Future large, randomized, controlled trials are needed to compare this technique with other modalities and highlight the definitive indications for this procedure.
Cryorecanalization is a safe and effective method for the immediate management of airway obstruction. Recently, this technique gained its place in the treatment of malignant endobronchial obstruction both with and without critical airway narrowing [16].
Conclusions
Appropriate patient selection and high success rates should be achieved after careful radiological assessments and with early management. Despite its high efficacy, low cost, and relative safety, this technique remains underutilized.
References
Cavaliere S, Venuta F, Foccoli P, Toninelli C, La Face B (1996) Endoscopic treatment of malignant airway obstructions in 2,008 patients. Chest 110:1536–1542
Schumann C, Hetzel M, Babiak AJ, Hetzel J, Merk T, Wibmer T et al (2010) Endobronchial tumour debulking with a flexible cryoprobe for immediate treatment of malignant stenosis. J Thorac Cardiovasc Surg 139:997–1000
Bolliger CT, Sutedja TG, Strausz J, Freitag L (2006) Therapeutic bronchoscopy with immediate effect: laser, electrocautery, argon plasma coagulation and stents. Eur Respir J 27:1258–1271
Bolliger CT, Sutedja TG, Strausz J, Freitag L (2002) ERS/ATS statement on interventional pulmonology. Eur Respir J 19:356–373
Vergnon JM, Huber RM, Moghissi K (2006) Place of cryotherapy, brachytherapy and photodynamic therapy in therapeutic bronchoscopy of lung cancers. Eur Respir J 28:200–218
Schumann C, Lepper PM, Barth TFE, Moller P, Kruger S (2009) Successful immediate cryorecanalization of a simultaneous high-grade tracheal and bronchial stenosis as rare manifestations of bronchial-associated lymphoid tissue lymphoma. J Thorac Cardiovasc Surg 137:e17–e19
Hetzel M, Hetzel J, Schumann C, Marx N, Babiak A (2004) Cryorecanalization: a new approach for the immediate management of acute airway obstruction. J Thorac Cardiovasc Surg 127:1427–1431
Reichle G, Freitag L, Kullmann HJ, Prenzel R, Macha HN, Farin G (2000) Argon plasma coagulation in bronchology: a new method—alternative or complementary? Pneumologie 54:508–516
Deygas N, Froudarakis M, Ozenne G, Vergnon JM (2001) Cryotherapy in early superficial bronchogenic carcinoma. Chest 120:26–31
Herth FJ, Eberhardt R, Becker HD, Ernst A (2005) Relief of malignant airway obstruction: a prospective and randomised comparison of five different endoscopic techniques. Chest 128(4):209S
Mathur PN, Wolf KM, Busk MF, Briete WM, Datzman M (1996) Fiberoptic bronchoscopic cryotherapy in the management of tracheobronchial obstruction. Chest 110:718–723
Hetzel J, Hetzel M, Hasel C, Moeller P, Babiak A (2008) Old meets modern: the use of traditional cryoprobes in the age of molecular biology. Respiration 76:193–197
Aktas Z, Gunay E, Taci Hoca N, Yilmaz A, Demirag F, Gunay S, Sipit T, Kurt EB (2010) Endobronchial cryobiopsy or forceps biopsy for lung cancer diagnosis. Ann Thorac Med 5(4):242–246. doi:10.4103/1817-1737.69117
Babiak A, Hetzel J, Krishna G, Fritz P, Moeller P, Balli T, Hetzel M (2009) Transbronchial cryobiopsy: a new tool for lung biopsies. Respiration 78:203–208
Loo PS, Thomas SC, Nicolson MC, Fyfe MN, Kerr KM (2010) Subtyping of undifferentiated non-small cell carcinomas in bronchial biopsy specimens. J Thorac Oncol 5:442–447
Du Rand IA, Barber PV, Goldring J et al (2011) British Thoracic Society guideline for advanced diagnostic and therapeutic flexible bronchoscopy in adults. Thorax 66:iii1–iii21
Disclosures
Dr. Aydın Yilmaz, Dr. Zafer Aktaş, Dr. Ibrahim O. Alici, Mr. Atalay Caglar, Dr. Hilal Sazak, and Dr. Fatma Ulus have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yılmaz, A., Aktaş, Z., Alici, İ.O. et al. Cryorecanalization: keys to success. Surg Endosc 26, 2969–2974 (2012). https://doi.org/10.1007/s00464-012-2260-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2260-1