Abstract
Background
The development of central airway obstruction during malignant diseases is an important cause of morbidity and mortality. Endobronchial therapies can decrease the patient’s symptoms and improve quality of life. Here, we compare airway recanalization methods: argon plasma coagulation with mechanical tumor resection (APC + MTR) and cryorecanalization (CR efficiency, complications, restenosis rate, and time to restenosis) in patients with malignant exophytic endobronchial airway obstruction.
Methods
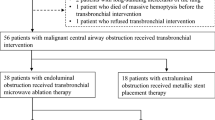
A total of 89 patients were included who were admitted to our hospital between 2005 and 2012. The data were analyzed retrospectively. Initially, a CR procedure was performed in 52 patients using rigid bronchoscopy under general anesthesia; the APC + MTR procedure was performed in 37 patients with malignant airway obstruction.
Results
The airway patency rate with APC + MTR was 97.3% (n = 36) and CR was 80.8% (n = 42). The APC + MTR procedure was more effective than CR for recanalization of malignant endobronchial exophytic airway obstruction. Additionally, the achievement rate of airway patency with APC + MTR was significantly higher in tumors with distal bronchial involvement. There was no statistically significant difference between groups in terms of complications, restenosis rate, and time to restenosis.
Conclusions
The APC + MTR procedure is preferred over CR to introduce and maintain airway patency in patients with malignancy-related endobronchial exophytic airway obstruction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Malignant airway obstruction presents with dyspnea, cough, hemoptysis, and atelectasis. It may lead to symptoms such as post-obstructive pneumonia and, thus, results in an increase in morbidity and mortality [1, 2]. Lung cancer is the most frequent cause of malignant airway obstruction, and 20–30% of patients exhibit significant symptoms associated with airway obstruction, usually due to local progression of disease. Unfortunately, 40% of these patients may not survive [3, 4]. Treatment of these symptoms with endobronchial methods is now recommended in the current guidelines [5].
Recently, various endobronchial therapy techniques have emerged for malignant airway obstruction, and these can be performed via a flexible or rigid bronchoscopy [6]. Cryotherapy was developed as an alternative utilization of the cryoprobe. It is now an established and rapid recanalization method that destroys tissues with high liquid contents (like tumor cells) by applying extreme cold to create adhesion (cryoadhesion) to the freezing source [7].
Argon plasma coagulation (APC) is an alternative non-contact electrocoagulation technique in which high-frequency current is delivered into the tissue through ionized argon gas to create plasma that thermally destroys tissue [8, 9]. In recent years, mechanical tumor resection with the cutting edge of a rigid bronchoscope after coagulation of the lesion by APC optimizes safety and offers a more efficient method to maintain airway patency [10, 11].
Here, we compare the airway recanalization methods including argon plasma coagulation with mechanical tumor resection (APC + MTR) and cryorecanalization (CR). We report the efficiency, complications, restenosis rate, and time to restenosis in patients with malignant exophytic endobronchial airway obstruction.
Materials and methods
We enrolled patients with symptomatic airway obstruction due to lung cancer who were admitted to our hospital between 2005 and 2012. The CR was initially performed in 52 patients between 2005 and 2011 using a rigid bronchoscopy followed by the APC + MTR procedure in 37 subjects in 2012. Until the establishment of interventional pulmonology clinic in 2012, these procedures were being performed only via the chest disease clinic between 2005 and 2011 so there are marked differences between case numbers per year.
A total number of 89 patients were analyzed retrospectively. Both groups had similar preoperative characteristics (Table 1).
The exclusion criteria included interventional operations performed via fiber optic bronchoscopy techniques during the same time period, other interventional operations due to malignancies (cryotherapy, APC, stent, intervention to hemoptysis), and interventions for benign lesions. We also excluded participants with major vascular invasion or external tumor compression in preoperative computed tomography, coagulation problems, or low platelet count, as well as pregnant subjects, those under the age of 18, and those who did not sign the informed consent.
Patients were taken to the operating room after the sedative pre-medication. General anesthesia was given via total intravenous anesthesia technique. Electrocardiogram, invasive arterial blood pressure, oxygen saturation, and arterial blood gases were monitored throughout the process. Patients were breathed with a high-frequency jet ventilation connected to a rigid bronchoscope via an adapter (Acutronic Medical Systems, Mistral Universal Jet Ventilator, Hirzel, Switzerland).
The patients were intubated with rigid scopes (“Hemer” scope, 43 cm length and 9.5 mm diameter or 35 cm length and 12 mm diameter, Richard Wolf Medical Instruments Corporation, Illinois, USA). CR used a rigid cryoprobe (53 cm length, 3 mm diameter, ERBE, Medizintechnik, GmbH, Tübingen, Germany) that was passed through the rigid bronchoscope.
The tip of the cryoprobe touched or was embedded in the tumor. A foot pedal activated the freezing, and tumor tissue adhered to probe via freezing was removed by the cryoprobe (Fig. 1). During the APC–MTR procedure, a rigid APC probe (50 cm length, 2.3 mm diameter, ERBE, Medizintechnik, GmbH, Tübingen, Germany) was pushed through the rigid bronchoscopy lumen. All visible tumor was coagulated with 60 W at 2 L/min flow rate and 3 s of firing. The tumor was then extracted by cutting the edge of the rigid bronchoscope or by snatching with rigid forceps. The FiO2 was decreased to below 40% during pyrexia in the APC procedure (Fig. 2).
We terminated the operation due to bleeding or cardiovascular complications. Bleeding during the operation was classified as mild, moderate, or severe bleedings as reported in the literature [12]. There were no long-term complications related to the procedure. All patients received the appropriate chemotherapy and/or radiotherapy according to the stage of their disease.
There was more than 50% ordinary diameter expansion of the bronchus diameter with malignant airway obstruction and the presence of distal healthy bronchus; these were accepted as procedure successes. Expansion below 50% and/or failure to reach a healthy bronchial at the distal narrowness were defined as failures [6, 10].
All patients were invited to the clinic to perform fiberoptic bronchoscopy to assess restenosis after 6 weeks from the first operation. All patients were followed for possible complications that may occur in the long term.
Statistical analysis
All data were analyzed with SPSS (Statistical Package for the Social Sciences) software for Windows Version 11.5. Individual and aggregate data were summarized using descriptive statistics including mean, standard deviations, medians (min–max), frequency distributions, and percentages. The normality of data distribution was verified by the Kolmogorov–Smirnov test. Variables were compared with a normal distribution using Student’s t test. For the continuous variables that were not normally distributed, the Mann–Whitney test was conducted to compare groups. Evaluation of categorical variables used a Pearson’s Chi-square test, Fisher’s exact test, and likelihood ratio test. A p value of <0.05 was considered statistically significant.
This study was performed with Institutional Review Board protocol approval date 27/06/2012 and number 98 from Keçiören Education and Research Hospital.
Results
The APC + MTR method achieved malignant airway patency in 36 (97.3%) of 37 patients. The CR method achieved patency in 42 (80.8%) of the 52 patients in our study. The APC + MTR procedure was significantly superior to the CR method (p = 0.023). In addition, the achievement of airway patency in the APC + MTR method was statistically higher in tumors with distal bronchial involvement (p = 0.017) (Table 2).
Restenosis was not observed within the first 6 weeks after successful interventions of maintaining airway patency in 31 (86.1%) of the 36 patients with the APC + MTR method and in 39 (92.9%) of the 42 patients with the CR method. Furthermore, 6 (22.2%) restenosis cases occurred in still alive 27 patients with successful interventions of APC + MTR method at a mean of 14 (3–71) weeks; 14 (35.0%) restenosis cases occurred in still alive 40 patients with successful CR interventions at a mean of 17 (2–112) weeks. There was no statistically significant difference between APC + MTR and CR methods regarding the restenosis rate and time to restenosis (Table 3).
There was no statistically significant difference between APC + MTR and CR methods in terms of incidence and variety of the complications that result in termination of the operation preoperatively (18.9% in APC + MTR method, 25.0% in CR method) (Table 4). Besides complications that require terminating the operations, there was no failure of patency in any APC + MTR cases. Frequency of moderate bleeding due to APC–MTR was 10.8%, but it does not affect the success of procedure. The CR method resulted in 5 patency failures including 1 case with severe bleeding (1%) and 4 with moderate bleeding (9%). Due to bleeding, airway patency procedure was resulted with failure and operation was turned into stop bleeding. All patients survived in both groups. There were no long-term complications with both techniques.
Discussion
Laser (L), electrocautery (EC), APC, cryotherapy (CT), brachytherapy, photodynamic therapy, and stents are classic methods for intervention of malignant airway obstruction [7]. In recent years, bronchoscopists have achieved more accurate results with a combination of mechanical tumor resection and hot techniques such as L, EC, and APC compared to individual techniques [7, 10]. The success rate of MTR alone ranges between 76 and 82% and that of APC between 54 and 91%. Finally, the combination of MTR and APC achieved a success rate of 96% in malignant airway patency [10, 13, 14]. In several studies, we reported airway patency success rates of 72–91% in the CR method, which is new and relatively different from classic CT. In our study, we demonstrated that the APC + MTR procedure is significantly superior to the CR method, which provides and maintains airway patency in patients with malignant endobronchial exophytic airway obstruction.
Another feature evaluated during these operations was the impact of tumor extension from the narrow area to the distal airways on procedure success. Distal bronchial involvement significantly reduced the achievement of airway patency in the CR method versus the APC + MTR method. There was distal bronchial involvement in all operations terminated with failure to achieve airway patency. In addition, distal bronchial involvement did not affect the success of the APC + MTR procedure. Moreover, the failure of airway patency observed in the CR method was comparable to published studies [15]. We conclude that the APC + MTR method is preferred to the CR method in tumors with preoperative distal bronchial involvement.
In a prospective randomized multicenter study, the rates of maintaining airway patency for 6 weeks via the MTR, APC, and APC + MTR methods were 0, 72, and 70%, respectively. Restenosis occurred within the first 6 weeks in most MTR patients [11]. Similarly, there was no statistically significant difference between APC + MTR and CR according to the rates of maintaining airway patency for 6 weeks after successful procedures.
There were no statistically significant differences between APC + MTR and CR according to the restenosis rate and time to restenosis. Other studies suggested the restenosis rates of 17.2–28% with the CR method [15, 16]. The restenosis rate seen here is comparable to the literature.
The mean time to restenosis was 20 weeks (range 4–104 weeks) from CR intervention to the detection of restenosis. There were no statistically significant differences between the APC + MTR and CR methods according to the time to restenosis observed here [15]. The average benefit time was 2–3 months (8–12 weeks) from interventional bronchoscopy in published data [17]. The average benefit time obtained here was comparable to the published data when considering the time to restenosis.
There was no statistically significant difference between the APC + MTR and CR methods in terms of incidence and variety of the complications that might cause termination of the interventional procedure. Moderate bleeding complications in the APC or APC + MTR method have not been reported in the literature before [10, 13]. Moderate bleeding was not reported as a complication of APC + MTR operations because the same device was used for both the APC + MTR procedure and to terminate moderate bleeding. Moderate bleeding occurred in both methods and was easily stopped via APC.
Moderate bleeding in the CR method was reported at 8–25% in the literature, which is comparable to our CR data. Severe bleeding during CR has not been reported previously [12, 15, 16]. In our study, severe bleeding was terminated with double-lumen endotracheal intubation at 72 h. Blood clots were cleaned with rigid bronchoscopy after two units of erythrocyte suspension replacement and successful extubation. Although it was not statistically significant, we suggest that necessary measures should be taken for severe and moderate bleeding during CR.
Despite being established for over 100 years, MTR remains dangerous because of bleeding complications. APC has a 100% success rate in terms of stopping bleeding originating from the visible side. Therefore, the combination of these two procedures is a reliable and successful method to rapidly open airways. Cryorecanalization is a mechanical resection method. The probe diameter limits tumor removal. Thus, it is a less reliable method to open airways.
The strongest point of our study is the comparison of two new methods for malignant airway obstruction intervention. Although there are numerous studies related to the utilization of these methods, there are a limited number of comparative studies in the literature. To the best of our knowledge, this is the first study to compare the APC + MTR method to the CR method.
Limitations of our study include the retrospective design and the case numbers being not equal in the two groups at the end of the study. In conclusion, the APC + MTR procedure is superior to the CR method to provide and maintain airway patency for the intervention of malignant airway obstruction and tumors with distal bronchial involvement. There was no statistically significant difference between methods according to the complications, restenosis rate, and time to restenosis. Therefore, these findings suggest that the APC + MTR procedure might be preferred to the CR method for airway patency in patients with malignancy-related endobronchial exophytic airway obstruction.
References
Martini N, Bains MS, Burt ME et al (1995) Incidence of local recurrence and second primary tumors in resected stage I lung cancer. Thorac Cardiovasc Surg 109:120–129
El Badrawy MK, Shalabi NM, Hewidy AA et al (2015) Sequential use of cryoextraction postelectrocautery for airway recanalization using fiberoptic bronchoscopy. Egypt J Bronchol 9(3):269
Honings J, Gaissert HA, Van Der Heijden H et al (2010) Clinical aspects and treatment of primary tracheal malignancies. ActaOto-Laryngol 130(7):763–772
Ginsberg RJ, Vokes EE, Ruben A (1997) Non–small cell lung cancer. In: DeVita VT et al (eds) Cancer: principles and practice of oncology. Lippincott-Raven, Philadelphia, pp 858–911
Noppen M, Meysman M, D’Haese J et al. (1997) Interventional bronchoscopy: 5-year experience at the Academic Hospital of the Vrije Universiteit Brussel (AZ-VUB). Acta Clin Belg 52:371–380
Bolliger CT, Mathur PN, Beamis JF et al (2002) ERS/ATS statement on interventional pulmonology. European Respiratory Society/American Thoracic Society. Eur Respir J 19:356–373
Vergnon JM, Huber RM, Moghissi K (2006) Place of cryotherapy, brachytherapy and photodynamic therapy in therapeutic bronchoscopy of lung cancers. Eur Respir J 28:200–218
Miller SM, Christina RB, Arjun C (2013) Argon plasma coagulation and electrosurgery for benign endobronchial tumors. J Bronchol Interv Pulmonol 20(1):38–40
Morice RC, Ece T, Ece F, Keus L (2001) Endobronchial argon plasma coagulation for treatment of hemoptysis and neoplastic airway obstruction. CHEST J 119(3):781–787
Reichle G, Freitag L, Kullmann HJ et al (2000) Argon plasma coagulation in bronchology: a new method–alternative or complementary? Pneumologie 54:508–516
Herth FJ, Eberhardt R, Becker HD, Ernst A (2005) Relief of malignant airway obstruction: a prospective and randomised comparison of five different endoscopic techniques. Chest 128(4):209
Schumann C, Hetzel M, Babiak AJ et al (2010) Endobronchial tumour debulking with a flexible cryoprobe for immediate treatment of malignant stenosis. J Thorac Cardiovasc Surg 139(4):997–1000
Crosta C, Spaggiari L, De Stefano A et al (2001) Endoscopic argon plasma coagulation for palliative treatment of malignant airway obstructions: early results in 47 cases. Lung Cancer 33(1):75
Jin FG, Mu DG, Chu DL et al (2008) Efficacy and safety of argon plasma coagulation in the treatment of obstructive tracheobronchial stenosis. ZhonghuaZhong Liu ZaZhi 30(6):462–464
Yılmaz A, Aktaş Z, Alici IO, et al. (2012) Cryorecanalization: keys to success. Surg Endosc 26(10):2969–2974
Hetzel M, Hetzel J, Schumann C et al (2004) Cryorecanalization: a new approach for the immediate management of acute airway obstruction. J Thorac Cardiovasc Surg 127:1427–1431
Bolliger CT, Probst R, Tschopp K, Solèr M, Perruchoud AP (1993) Silicone stents in the management of inoperable tracheobronchial stenoses. Indications and limitations. Chest 104:1653–1659
Acknowledgements
We would like to thank Zafer Aktaş for his kind help and advice in the course of the present study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Derya Kızılgöz, Zafer Aktaş, Aydın Yılmaz, Ayperi Öztürk, and Fatih Seğmen declare that they have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Kızılgöz, D., Aktaş, Z., Yılmaz, A. et al. Comparison of two new techniques for the management of malignant central airway obstruction: argon plasma coagulation with mechanical tumor resection versus cryorecanalization. Surg Endosc 32, 1879–1884 (2018). https://doi.org/10.1007/s00464-017-5877-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5877-2