Abstract
Background
The objective of this review was to provide an overview of the components that comprise each of the eight barrier mesh prostheses commonly utilized for LVHR and to review the current literature related to the characteristics and effectiveness of these materials to guide the general surgeon in selecting the most appropriate material for LVHR.
Methods
Composite prostheses with permanent barriers (Bard™ Composix™ E/X, Bard™ Composix™ L/P, and DUALMESH® Biomaterial) were compared to composite prostheses with absorbable barriers (C-QUR™ Mesh, PROCEED™ Surgical Mesh, Bard™ Sepramesh™ IP Composite, Parietex™ Composite, and PHYSIOMESH™) using scanning electron microscopy and a review of the current preclinical and clinical literature.
Results
Clinical studies and preclinical animal models have attempted to determine the adhesion characteristics and effectiveness of barrier mesh prostheses available for ventral hernia repair applications. However, it is difficult to make any definitive statements about the adhesion characteristics and effectiveness of these materials because all meshes were not included in all studies and likewise not compared under identical conditions. Overall, Parietex™ Composite and DUALMESH® Biomaterial were cited most frequently for improvement of adhesion characteristics, followed closely by Bard™ Sepramesh™ IP Composite and C-QUR™ Mesh. Bard™ Composix™, PROCEED™ Surgical Mesh, and uncoated polypropylene were cited most frequently as having the most tenacious and extensive adhesions.
Conclusions
Differences observed between the various barrier prostheses are likely attributable to the chemical composition of the barrier or the conditions required for resorption and metabolism of the barrier components. It is likely that the components of these barriers incite a wide range of inflammatory responses resulting in the range of adhesion coverage and tenacity observed in the preclinical and clinical studies reviewed. Clinical trials are needed to more appropriately define the clinical effectiveness of these barriers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
During the past 50 years, hernia repair techniques have evolved from primary suture repair to the use of synthetic mesh products to accomplish a “tension-free” repair to minimally invasive laparoscopic techniques. Burger et al. have shown that the use of mesh to repair incisional hernias reduces recurrence rates from 63% to 32% at 10 years follow-up [1]. Laparoscopic techniques have further improved the field of hernia repair by not only reducing recurrence rates but also reducing complications and length of hospital stay compared with open techniques [2, 3]. One drawback of laparoscopic hernia repair (LVHR), however, is the placement of prosthetic mesh materials inside the abdomen. These mesh materials are in direct contact with the abdominal viscera and can form adhesions leading to pain, fistula formation, bowel obstruction, or adhesiolysis-related complications, such as enterotomy and unplanned bowel resection during subsequent surgical procedures [4–6].
In a recent study, Halm et al. evaluated patients with prior placement of mesh in the intraperitoneal or preperitoneal position and found that intraperitoneal mesh placement was associated with significantly greater adhesions (62% vs. 26%), resulting in difficult adhesiolysis and significantly greater perioperative complications (76% vs. 29%), small-bowel resections (21% vs. 0%), and surgical site infections (26% vs. 4%) [6]. The majority of the meshes (93%) were uncoated polypropylene without an adhesion barrier, which allowed the formation of dense adhesions and contributed to considerable complications during subsequent abdominal surgeries.
Furthermore, Gray et al. have shown that the incidence of enterotomy or unplanned bowel resection is almost four times higher in patients with previous intraperitoneal mesh repair compared with those repaired previously without mesh [5]. These complications were associated with increased operative time, length of hospital stay, risk of postoperative complications, and development of enterocutaneous fistula. Again, the types of meshes utilized in these cases were not fully identified, but the majority were uncoated polypropylene without an adhesion barrier. Thus, it is likely that dense adhesions and difficult adhesiolysis ultimately resulted in enterotomy or unplanned bowel resection.
Prosthetic mesh materials have evolved since Usher first introduced uncoated polypropylene mesh in the late 1950s [7]. The hernia mesh industry now includes a wide variety of products, including permanent synthetic polymer materials, biological tissue-based materials, composite prostheses, and absorbable synthetic polymer materials. Composite prostheses represent the ideal design for LVHR applications, because these materials are comprised of a permanent synthetic mesh material on the parietal side and an adhesion barrier layer on the visceral side. The mesh side is intended to promote tissue ingrowth and anchor the prosthesis to the abdominal wall, whereas the barrier layer prevents adhesion of the abdominal viscera to the underlying mesh. The barrier layer also minimizes spontaneous difficulties, such as bowel obstruction, erosion, and fistula formation, and potentially reduces complications related to enterotomy or unplanned bowel resection associated with difficult adhesiolysis during subsequent abdominal surgeries.
A variety of composite barrier prostheses have been developed and can be divided into two basic categories: those with permanent barrier layers, and those with absorbable (temporary) barrier layers or coatings. Prostheses, such as Bard™ Composix™ E/X (C.R. Bard/Davol, Inc., Warwick, RI) Bard™ Composix™ L/P (C.R. Bard/Davol, Inc., Warwick, RI), and DUALMESH® Biomaterial (W.L. Gore & Associates, Inc., Flagstaff, AZ) are examples of composite prostheses with permanent barrier layers, whereas C-QUR™ Mesh (Atrium Medical Corp., Hudson, NH), PROCEED™ Surgical Mesh (Ethicon, Inc., Somerville, NJ), Bard™ Sepramesh™ IP Composite (C.R. Bard/Davol, Inc., Warwick, RI), Parietex™ Composite (Covidien, Mansfield, MA), and PHYSIOMESH™ (Ethicon, Inc., Somerville, NJ) are examples of prostheses with absorbable barrier layers/coatings. These absorbable barriers are typically degraded by the body over the course of 30 days with some components lasting up to 240 days [8–11]. After the barrier layer is fully resorbed, the permanent, synthetic mesh material is left behind for the long-term hernia repair. The injured peritoneum forms a new mesothelial layer as quickly as 5–7 days after surgery, so the first postoperative week is the critical period for preventing adhesions to the prosthetic mesh [12]. However, some recent studies have shown increased adhesion formation between 7 and 30 days, likely due to increased inflammation while the barrier layers are being degraded and resorbed [13].
Due to the variety of prosthetic mesh materials now available, the general surgeon is faced with the difficult decision of determining which material is most appropriate for a particular hernia repair application. The objectives of this review are to provide an overview of the components comprising each of the eight barrier mesh prostheses commonly utilized for LVHR, as well as to review the current literature relevant to the characteristics and effectiveness of these materials.
Materials and methods
Materials evaluated
Permanent barriers
-
Bard™ Composix™ E/X (C.R. Bard/Davol, Inc., Warwick, RI)
-
Bard™ Composix™ L/P (C.R. Bard/Davol, Inc.)
-
DUALMESH® Biomaterial (W.L. Gore & Associates, Inc. Flagstaff, AZ)
Absorbable barriers
-
C-QUR™ Mesh (Atrium Medical Corp., Hudson, NH)
-
PROCEED™ Surgical Mesh (Ethicon, Inc., Somerville, NJ)
-
Bard™ Sepramesh™ IP Composite (C.R. Bard/Davol, Inc.)
-
Parietex™ Composite (Covidien, Mansfield, MA)
-
PHYSIOMESHTM (Ethicon, Inc.)
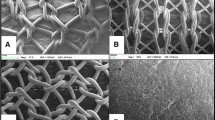
Scanning electron micrographs
Samples of each mesh were prepared for scanning electron microscopy (SEM) by mounting 0.5- × 0.5-mm specimens on SEM stubs using double-sided Scotch tape and silver paint. The samples were sputter coated with approximately 100 Å of Au/Pd alloy using a Technics Hummer V Sputter Coater (San Jose, CA). A LEO 435VP SEM (LEO Electron Microscopy Ltd, Cambridge, England) was then utilized at 20 kV and approximately 8.0 × 10−6 torr to capture images at ×60, ×200, and ×3000 magnifications.
Results
Table 1 provides an overview of the components of each of the composite mesh prostheses, including the expected resorption time of each component, and Fig. 1 depicts scanning electron micrographs taken of the cross-section of each of the prostheses at ×60 and ×200 magnifications.
Scanning electron micrographs. A Composix E/X, ×60; B Composix E/X, ×200; C Composix L/P, ×60; D Composix L/P, ×200; E DualMesh, ×60; F DualMesh, ×200; G Sepramesh, ×60; H Sepramesh, ×200; I C-QUR, ×60; J C-QUR, ×200; K Parietex Composite, ×60; L Parietex Composite, ×200; M Proceed, ×60; N Proceed, ×200; O Physiomesh, ×60; P Physiomesh, ×200
Permanent barrier prostheses
Bard™ Composix™ E/X & Bard™ Composix™ L/P
Bard™ Composix™ E/X (Fig. 1A and B) and Bard™ Composix™ L/P (Fig. 1C and D) are both comprised of a permanent synthetic mesh layer (polypropylene, PP) combined with a permanent barrier layer (expanded polytetrafluoroethylene, ePTFE). The two layers are attached to each other via concentric rings of monofilament polytetrafluoroethylene stitches, which allow the prostheses to be trimmed to fit a variety of defect sizes without permitting the layers to delaminate [14, 15]. The difference between Bard™ Composix™ E/X and Bard™ Composix™ L/P is the density of the polypropylene mesh layer. Bard™ Mesh (density: 102.5 ± 1.7 g/m2) [14, 16] is utilized in the Bard™ Composix™ E/X meshes, and Bard™ Soft Mesh (density: 40.7 ± 0.7 g/m2) [15, 16] is utilized in the Bard™ Composix™ L/P meshes, allowing the surgeon to choose the most appropriate density for a particular repair.
DUALMESH® biomaterial and DUALMESH® PLUS biomaterial
DUALMESH® Biomaterial is comprised of a permanent dual-sided expanded polytetrafluoroethylene (ePTFE) material (Fig. 1E and F). One side is textured with pore sizes conducive to tissue ingrowth, whereas the other side has a smooth texture and a closed structure to prevent adhesions [17]. A further enhancement of DUALMESH® Biomaterial is the DUALMESH® PLUS Biomaterial, which is impregnated with silver carbonate and chlorhexidine diacetate and has been shown to inhibit microbial colonization, such as E. coli, S. aureus, P. aeruginosa, K. pneumoniae, S. epidermidis, and C. albicans using in vitro models [18, 19].
Absorbable barrier prostheses
Bard™ Sepramesh™ IP Composite
Bard™ Sepramesh™ IP Composite is comprised of a permanent synthetic mesh (polypropylene, PP) co-knitted with absorbable polyglycolic acid fibers (PGA). An absorbable hydrogel layer comprised of sodium hyaluronate (HA), carboxymethylcellulose (CMC), and polyethylene glycol (PEG) is coated on the PGA side of the co-knitted mesh to form an absorbable adhesion barrier layer (Fig 1G and H) [9]. The PGA fibers are utilized to improve binding of the hydrogel layer to the polypropylene mesh layer. The PGA is hydrolytically degraded during a period of approximately 50–80 days into glycolic acid, which is absorbed and metabolized by the body [9, 20]. The HA/CMC/PEG hydrogel barrier layer is absorbed within approximately 30 days. HA is a linear polysaccharide comprised of d-glucuronic acid and N-acetyl-d-glucosamine [21]. HA molecules can enter the lymphatic system and be broken down into both high and low molecular weight byproducts, which enter the bloodstream and are metabolized by the liver [21]. CMC is a derivative of cellulose, which is enzymatically hydrolyzed, metabolized by macrophages, and finally excreted [22]. The plasticizer, PEG, is absorbed by the lymphatic system, circulated in the blood, and finally cleared through the kidneys [23].
C-QUR™ Mesh
C-QUR™ Mesh is comprised of a permanent synthetic mesh layer (polypropylene: ProLite™) with an absorbable gel coating comprised of omega-3 fatty acids, lipids, and glycerides derived from fish oil (Figs. 1I and J) [24, 25]. This gel material is coated onto the individual polypropylene mesh monofilaments and undergoes a gentle, thermal crosslinking process to form the protective semi-solid gel coating [26]. This coating is absorbed in vivo during a period of approximately 90-120 days via hydrolysis by body fluids and lipase enzymes [26]. Once the crosslinked bonds of the gel are cleaved, the coating is converted into naturally occurring fatty acids, glycerides, and fatty alcohols, which are absorbed and then consumed via normal lipid metabolism [26]. It is believed that this omega-3 fatty acid coating possesses antimicrobial [27, 28] and anti-inflammatory properties [29, 30].
Parietex™ Composite
Parietex™ Composite is comprised of a permanent synthetic mesh layer of multifilamented polyester (polyethylene terephthalate, PET). An absorbable coating comprised of porcine collagen, polyethylene glycol, and glycerol is then coated onto the mesh to provide an absorbable adhesion barrier layer (Fig. 1K and L) [31]. The collagen film is created using type I porcine atelocollagen (a partially digested collagen typically produced by removal of the antigenic telopeptides using a protease such as pepsin) with a nonreactive additive, such as polyethylene glycol or glycerol [32, 33]. This collagen film is expected to degrade via neutrophil collagenase (MMP-8) activity [34] within approximately 30 days, leaving behind the polyester mesh as the permanent hernia repair material. The glycerol component of the film is readily absorbed by the cells in vivo and enzymatically converted into glycerol-3-phosphate for cellular energy production [35]. Polyethylene glycol is expected to be absorbed by the lymphatic system, circulated in the blood, and finally cleared through the kidneys [23].
PROCEED™ Surgical Mesh
PROCEED™ Surgical Mesh is comprised of a permanent synthetic mesh layer (polypropylene: PROLENE™ Soft Mesh) encapsulated by an absorbable film (polydioxanone, PDS), which is utilized to bind the permanent mesh layer to the absorbable adhesion barrier layer comprised of oxidized regenerated cellulose (ORC) fabric (Fig. 1M and N) [8].
The polydioxanone (PDS) film is a polyester material that was originally developed for use as an absorbable suture material. PDS is created by ring-opening polymerization of p-dioxanone along with heat and the addition of a catalyst [36]. When the PROCEED™ Surgical Mesh is assembled, the PDS is sandwiched between the ORC and the polypropylene mesh and is designed to degrade at a much slower rate than the ORC fabric. According to the PROCEED™ Surgical Mesh instructions for use, the PDS is expected to be resorbed within approximately 180 days [8]. PDS contains ether and ester linkages, which degrade via hydrolysis to form byproducts that are converted into carbon dioxide and water [37].
Oxidized regenerated cellulose (ORC) is created from Rayon fabric (regenerated cellulose), which has the same chemical structure as cellulose. Regenerated cellulose is created by extraction of cellulose from wood pulp that is treated by the Viscose process to create regenerated cellulose fibers [38]. Rayon fabric (consisting of primarily d-glucose units) must be further oxidized to become bioabsorbable ORC (consisting of a mixture of d-glucose and d-glucuronic acid units) [39–41]. According to the PROCEED™ Surgical Mesh instructions for use, the ORC is absorbed within approximately 28 days [8]. The mechanism of ORC degradation has been previously studied both in vitro and in vivo [41, 42]. Dimitrijevich et al. exposed ORC to plasma and serum in vitro and determined that the ORC undergoes chain shortening, which yields oligomers. These oligomers then hydrolyze into smaller fragments, such as d-glucuronic acid and d-glucose [41]. Dimitrijevich’s in vivo studies also have demonstrated that rabbit peritoneal macrophages digest and hydrolyze ORC [42].
PHYSIOMESH™
PHYSIOMESH™ is comprised of a permanent synthetic mesh material (polypropylene, PP) encapsulated with polydioxanone (PDS) to facilitate bonding of two polyglecaprone-25 absorbable barrier layers, one to each side of the polypropylene mesh (Fig. 1O and P) [11]. PDS is a polyester material that was originally developed for use as an absorbable suture material, which is created by ring-opening polymerization of p-dioxanone along with heat and the addition of a catalyst [36]. PDS contains ether and ester linkages, which degrade via hydrolysis and form byproducts that are converted into carbon dioxide and water [37], and the PDS is expected to be fully resorbed within approximately 180 days. The polyglecaprone-25 layer is comprised of a copolymer of ε-caprolactone and glycolide, which degrade through hydrolysis [43] and are expected to be fully resorbed within approximately 240 days [11].
Discussion
A number of clinical studies have evaluated the adhesion characteristics associated with intraperitoneal placement of mesh prostheses and the impact of absorbable and permanent barrier layers on reducing adhesions [44–49]. In one study, adhesions to polyester mesh materials were evaluated via ultrasound examination of visceral slide in patients with Parietex™ Composite mesh compared with uncoated polyester mesh. The results demonstrated that the protective barrier layer of the Parietex™ Composite significantly reduced the incidence of adhesions from 77% for uncoated polyester to 18% for Parietex™ Composite [44]. In another study, infection and recurrence rates associated with the use of Bard™ Composix™ mesh materials were assessed in 95 cases of previous open incisional hernia repair with intraperitoneal mesh placement. In this particular series, Bard™ Composix™ mesh materials had an 8% infection rate and overall 10% recurrence rate [45], but this study lacked a comparison to bare polypropylene or to a prosthesis with an alternative barrier.
Clinical studies were identified that evaluated the adhesions observed at the time of a subsequent abdominal surgery. In the first study, 65 subjects (n = 65) with DUALMESH® Biomaterial implanted in the intraperitoneal position during a previous laparoscopic ventral hernia repair were evaluated at the time of reoperation. The majority (91%) exhibited zero or filmy adhesions, and only a few (9%) exhibited dense adhesions to the omentum or to the tacking devices utilized to attach the mesh to the anterior abdominal wall [46]. In a similar study, 72 subjects (n = 72) with DUALMESH® Biomaterial implanted during a previous laparoscopic ventral or incisional hernia repair were evaluated at the time of a subsequent operation. The majority (83%) exhibited adhesions with 65% involving omentum and 18% involving bowel. However, the adhesiolysis was easily performed and inadvertent enterotomies were avoided [50]. In a third study, 85 subjects (n = 85) with Parietex™ Composite implanted during a previous laparoscopic incisional or ventral hernia repair were evaluated at the time of reoperation. The majority exhibited zero (47%) or loose adhesions to the omentum (42%), whereas the rest (11%) exhibited mild serosal adhesions [49]. However, these studies lacked quantification of the characteristics of the adhesions, such as area covered by adhesions, adhesion tenacity, or measurement of adhesiolysis time.
Only one clinical study provided a comprehensive comparison of the majority of the barrier mesh prostheses available for hernia repair applications [48]. In this particular study, Jenkins et al. compared the adhesion characteristics and adhesiolysis-related complications associated with uncoated polypropylene mesh, permanent barrier composite prostheses (Bard™ Composix™), permanent barrier noncomposite prostheses (DUALMESH® Biomaterial), absorbable barrier prostheses (C-QUR™ Mesh, Parietex™ Composite, PROCEED™ Surgical Mesh, and Bard™ Sepramesh™ IP Composite), and biological tissue-derived prostheses (AlloDerm®, Surgisis®, FlexHD®, CollaMend™, AlloMax™, and Permacol™) at the time of laparoscopic reexploration of a previous ventral hernia repair. The only barrier mesh prosthesis not included in this study was PHYSIOMESH™, which was not commercially available at the time that this study was conducted.
Sixty-nine patients were enrolled in this study, with 12 uncoated polypropylene mesh, 17 permanent barrier composite prostheses, 14 permanent barrier noncomposite prostheses, 18 absorbable barrier prostheses, and 8 biological tissue-derived materials. The results revealed that DUALMESH® Biomaterial performed well overall with significantly less tenacious adhesions (score of 2.4 ± 0.6 indicative of dense adhesions requiring blunt dissection) compared with all other types of meshes, which generally scored approximately 3.0–3.5, indicating the presence of dense adhesions requiring sharp dissection or the inability to separate the adhesions from the mesh in some cases. Statistically significant differences were not detected between the other mesh types: uncoated mesh, permanent barrier composite prostheses, absorbable barrier prostheses, and biological tissue-derived prostheses.
Scores for adhesion surface area were assigned based on 10% intervals of surface area covered by adhesions. DUALMESH® Biomaterial exhibited significantly less surface area covered by adhesions compared with Bard™ Composix™ and uncoated polypropylene mesh. Statistically significant differences were not detected between the other mesh types: absorbable barrier prostheses biological tissue-derived prostheses.
A ratio of adhesiolysis time to adhesion area (min/cm2) was utilized as a surrogate for operative complexity, and the results indicated that DUALMESH® Biomaterial exhibited a significantly lower ratio of adhesiolysis time to adhesion area compared with uncoated polypropylene mesh, Bard™ Composix™, and biologic mesh. However, no differences were detected with the absorbable barrier prostheses. Adhesiolysis-related complications were documented in two cases—one cystotomy and one enterotomy; both were associated with the use of uncoated polypropylene mesh.
A few trends were documented between the absorbable barrier prosthesis, although statistical significance was not achieved due to low numbers of patients in each group (PROCEED™ Surgical Mesh n = 8, C-QUR™ Mesh n = 5, Bard™ Sepramesh™ IP Composite n = 4, and Parietex™ Composite n = 1). For instance, C-QUR™ Mesh consistently exhibited the lowest adhesion tenacity, least area covered by adhesions, and lowest ratio of adhesiolysis time to adhesion area compared with the other three absorbable barrier prostheses. PROCEED™ Surgical Mesh consistently exhibited the highest values across all of these categories. However, due to the pilot nature of the project, this study was underpowered to detect significant differences within each subcategory of mesh. For this reason, a multi-institutional clinical trial is currently underway to expand this pilot project with the goal of elucidating the effectiveness of barrier-coated versus non-barrier-coated mesh in reducing adhesions and adhesiolysis-related complications after intraperitoneal placement during ventral hernia repair applications (clinicaltrials.gov protocol number: NCT01355939).
Numerous preclinical animal models have attempted to determine the adhesion characteristics and effectiveness of barrier mesh prostheses available for ventral hernia repair applications. Porcine [51–53], rat [13, 54–56], and rabbit models [10, 57–60] have all been described evaluating a variety of mesh types in a number of combinations. Of 12 studies cited, bare polypropylene was evaluated in 10 studies [10, 13, 52–56, 58–60], Parietex™ Composite [10, 13, 51–56] and DUALMESH® Biomaterial in 8 studies [10, 52, 54–59], Bard™ Composix™ in 7 studies [10, 51, 54, 55, 57, 59, 60], Bard™ Sepramesh™ IP Composite in 6 studies [10, 54–57, 60], PROCEED™ Surgical Mesh in 4 studies [10, 13, 53, 59], C-QUR™ Mesh in 2 studies [10, 13], and PHYSIOMESH™ in 0 studies. It is difficult to make any definitive statements about the adhesion characteristics and effectiveness of these materials, because all meshes were not included in all studies and likewise not compared under identical conditions. However, some basic trends do emerge. Overall, Parietex™ Composite and DUALMESH® Biomaterial were cited most frequently for improvement of adhesion characteristics, followed closely by Bard™ Sepramesh™ IP Composite and C-QUR™ Mesh. Bard™ Composix™, PROCEED™ Surgical Mesh, and uncoated polypropylene were cited most frequently as having the most tenacious and extensive adhesions.
Of these 12 studies, only one compared 6 barrier mesh prostheses to each other and to an uncoated polypropylene control, making it the best available comparison of these materials [10]. In this particular study, Pierce et al. evaluated the amount and tenacity of adhesions, mesh contracture, and overall tissue response to bare polypropylene mesh (ProLite™ Ultra™) compared with permanent barrier prostheses (Bard™ Composix™ M and DUALMESH® Biomaterial) and absorbable barrier prostheses (C-QUR™ Mesh, Parietex™ Composite, PROCEED™ Surgical Mesh, and Bard™ Sepramesh™ IP Composite) in a rabbit model during a period of 120 days. The meshes were placed on an intact peritoneum without any intentional bowel abrasion, essentially evaluating only the intraperitoneal response. The only mesh not included in this study was PHYSIOMESH™, which was not commercially available at the time that this study was conducted.
After 120 days, DUALMESH® Biomaterial and Bard™ Sepramesh™ IP Composite exhibited significantly fewer adhesions with significantly lower tenacity compared with PROCEED™ Surgical Mesh, which exhibited the greatest amount and tenacity of adhesions out of all of the meshes evaluated. No significant differences in adhesion amount or tenacity were detected between the other meshes evaluated. However, it should be noted that many of the meshes scored less than 1.5 for adhesion tenacity, which corresponds to a mixture of mostly zero adhesions with a few filmy adhesions. With regard to overall mesh contracture, C-QUR™ Mesh exhibited the least contracture overall and significantly less contracture than PROCEED™ Surgical Mesh and DUALMESH® Biomaterial, which exhibited the greatest contracture overall. No significant differences in mesh contracture were detected between the other meshes evaluated. Detailed histological analyses revealed similar results for all of the meshes in terms of abdominal wall incorporation, vascularity, necrosis, and mesothelialization. Overall, the meshes exhibited an established neointima, moderate vascularization, a lack of surrounding necrosis, and development of a neoperitoneum.
Pierce et al. concluded that the differences observed between the various barrier prostheses were likely attributable to the chemical makeup of the barrier or the conditions required for resorption and metabolism of the barrier components. It is likely that the components of these barriers incite a wide range of inflammatory responses, resulting in the range of adhesion coverage and tenacity observed. In fact, Schreinemacher et al. have observed this phenomenon in a 30-day rat study [13]. After 7 days, C-QUR™ Mesh exhibited less inflammation than PROCEED™ Surgical Mesh and Parietex™ Composite. Moderate to abundant macrophages and giant cells were observed phagocytosing the barrier layers of PROCEED™ Surgical Mesh and Parietex™ Composite, but only a few of these cells were observed in the C-QUR™ Mesh specimens 7 days postoperatively. By 30 days, the collagen layer of the Parietex™ Composite was completely resorbed. Thus, macrophages were not observed in these specimens, but giant cells remained. However, moderate to abundant macrophages and giant cells were still observed in the PROCEED™ Surgical Mesh specimens 30 days postoperatively, and these cells continued to degrade the ORC barrier layer. Only a few macrophages and giant cells were observed in the C-QUR™ Mesh specimens, and the coating layer remained intact 30 days postoperatively. This study also demonstrated increased adhesion formation for all of the barrier mesh prostheses between 7 and 30 days, which the authors attributed to increased inflammation related to the degradation and resorption of the barrier layer components, which were ongoing between 7 and 30 days. This effect was most pronounced in PROCEED™ Surgical Mesh materials, which again highlights the influence that the chemistry of the particular barrier components may have over the inflammatory response and subsequent adhesion formation. In particular, the anti-inflammatory properties of omega-3 fatty acids [29, 30] may contribute to the low-grade inflammatory response and minimal adhesions observed for the C-QUR™ Mesh materials in this study.
Conclusions
Numerous clinical studies and preclinical animal models have attempted to determine the adhesion characteristics and effectiveness of barrier mesh prostheses available for ventral hernia repair applications. However, it is difficult to make any definitive statements about the adhesion characteristics and effectiveness of these materials, because all meshes were not included in all studies and likewise not compared under identical conditions. Thus, clinical trials are needed to more appropriately define the clinical effectiveness of these barriers. For this reason, we have initiated a multi-institutional clinical trial to assess the effectiveness of barrier-coated versus non-barrier-coated mesh in reducing adhesions and adhesiolysis-related complications after intraperitoneal placement during ventral hernia repair applications (clinicaltrials.gov protocol number: NCT01355939).
References
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–583
Heniford BT, Park A, Ramshaw BJ, Voeller G (2003) Laparoscopic repair of ventral hernias: nine years’ experience with 850 consecutive hernias. Ann Surg 238:391–399
Pierce RA, Spitler JA, Frisella MM, Matthews BD, Brunt LM (2007) Pooled data analysis of laparoscopic vs. open ventral hernia repair: 14 years of patient data accrual. Surg Endosc 21:378–386
Ray NF, Denton WG, Thamer M, Henderson SC, Perry S (1998) Abdominal adhesiolysis: inpatient care and expenditures in the United States in 1994. J Am Coll Surg 186:1–9
Gray SH, Vick CC, Graham LA, Finan KR, Neumayer LA, Hawn MT (2008) Risk of complications from enterotomy or unplanned bowel resection during elective hernia repair. Arch Surg 143:582–586
Halm JA, de Wall LL, Steyerberg EW, Jeekel J, Lange JF (2007) Intraperitoneal polypropylene mesh hernia repair complicates subsequent abdominal surgery. World J Surg 31:423–429
Usher FC, Ochsner J, Tuttle LJ (1958) Use of Marlex mesh in the repair of incisional hernias. Am Surg 24:969–974
(2007) PROCEED Surgical mesh instructions for use
(2005) Sepramesh IP composite instructions for use
Pierce RA, Perrone J, Nimeri A, Sexton J, Walcutt J, Frisella M, Matthews B (2009) 120-day comparative analysis of adhesion grade and quantity, mesh contraction, and tissue response to a novel omega-3 fatty acid bioabsorbable barrier macroporous mesh after intraperitoneal placement. Surg Innov 16:46–54
(2011) PHYSIOMESH instructions for use. Ethicon, Inc
Tingstedt B, Isaksson K, Andersson E, Andersson R (2007) Prevention of abdominal adhesions—present state and what’s beyond the horizon? Eur Surg Res 39:259–268
Schreinemacher MH, Emans PJ, Gijbels MJ, Greve JW, Beets GL, Bouvy ND (2009) Degradation of mesh coatings and intraperitoneal adhesion formation in an experimental model. Br J Surg 96:305–313
(2005) Bard* Composix E/X mesh instructions for use
(2006) Composix L/P instructions for use. CR Bard
Deeken CR, Abdo MS, Frisella MM, Matthews BD (2011) Physicomechanical evaluation of absorbable and nonabsorbable barrier composite meshes for laparoscopic ventral hernia repair. Surg Endosc 25:1541–1552
(2007) DualMesh biomaterial instructions for use
(2008) Gore DUALMESH PLUS biomaterial instructions for use
Fox C et al (1991) Infection-resistant compositions, medical devices and surfaces and methods for preparing the same. U.S. Patent #5019096
Ratner BD, Hoffman AS, Schoen FJ, Lemons JE (2004) Biomaterials science. Academic Press, San Diego
Laurent TC (1987) Biochemistry of hyaluronan. Acta Otolaryngol Suppl 442:7–24
Turaev A (1995) Dependence of the biodegradability of carboxymethylcellulose on its supermolecular structure and molecular parameters. Chem Nat Compds 31:254–259
Yamaoka T, Tabata Y, Ikada Y (1995) Fate of water-soluble polymers administered via different routes. J Pharm Sci 84:349–354
Earle DB, Mark LA (2008) Prosthetic material in inguinal hernia repair: how do I choose? Surg Clin North Am 88:179–201
(2009) C-QUR mesh instructions for use
(2007) What is atrium’s omega-3–coated mesh and what happens following implantation? Atrium Medical Corp Technical Data Report No 010. http://www.atriummed.com/EN/Biosurgery/cqur-data.asp
Kabara J, Swieczkowski D, Conley AJ, Truant J (1972) Fatty acids and derivatives as antimicrobial agents. Antimicrob Agents Chemother 2:23–28
Thormar H, Isaacs CE, Brown HR, Barshatzky MR, Pessolano T (1987) Inactivation of enveloped viruses and killing of cells by fatty acids and monoglycerides. Antimicrob Agents Chemother 31:27–31
Ferrucci L, Cherubini A, Bandinelli S, Bartali B, Corsi A, Lauretani F, Martin A, Andres-Lacueva C, Senin U, Guralnik JM (2006) Relationship of plasma polyunsaturated fatty acids to circulating inflammatory markers. J Clin Endocrinol Metab 91:439–446
Arita M, Yoshida M, Hong S, Tjonahen E, Glickman JN, Petasis NA, Blumberg RS, Serhan CN (2005) Resolvin E1, an endogenous lipid mediator derived from omega-3 eicosapentaenoic acid, protects against 2,4,6-trinitrobenzene sulfonic acid-induced colitis. Proc Natl Acad Sci USA 102:7671–7676
(2010) Parietex composite instructions for use
Ory F et al (2002) Composite prosthesis for preventing post-surgical adhesions and method for obtaining same. U.S. Patent #09463313
Tayot J et al (2002) Collagenic material useful in particular for preventing post-operative adhesions. U.S. Patent #6391939
van Amerongen MJ, Harmsen MC, Petersen AH, Kors G, van Luyn MJ (2006) The enzymatic degradation of scaffolds and their replacement by vascularized extracellular matrix in the murine myocardium. Biomaterials 27:2247–2257
Campbell M (1995) Biochemistry. Saunders, New York
Boland ED, Coleman BD, Barnes CP, Simpson DG, Wnek GE, Bowlin GL (2005) Electrospinning polydioxanone for biomedical applications. Acta Biomater 1:115–123
Pillai CK, Sharma CP (2010) Review paper: absorbable polymeric surgical sutures: chemistry, production, properties, biodegradability, and performance. J Biomater Appl 25:291–366
Ashton W et al (1968) Oxidized cellulose product and method for preparing the same. U.S. Patent #3364200
Boardman F et al (1993) Cellulose oxidation by a perfluoronated hydrocarbon solution of nitrogen dioxide. U.S. Patent #5180398
Wiseman D et al (2003) Bioabsorbable medical devices from oxidized polysaccharides. U.S. Patent #20030073663
Dimitrijevich SD, Tatarko M, Gracy RW, Linsky CB, Olsen C (1990) Biodegradation of oxidized regenerated cellulose. Carbohydr Res 195:247–256
Dimitrijevich SD, Tatarko M, Gracy RW, Wise GE, Oakford LX, Linsky CB, Kamp L (1990) In vivo degradation of oxidized, regenerated cellulose. Carbohydr Res 198:331–341
Nary FH, Matsumoto MA, Batista AC, Lopes LC, de Goes FC, Consolaro A (2002) Comparative study of tissue response to polyglecaprone 25, polyglactin 910 and polytetrafluoroethylene suture materials in rats. Braz Dent J 13:86–91
Arnaud JP, Hennekinne-Mucci S, Pessaux P, Tuech JJ, Aube C (2003) Ultrasound detection of visceral adhesion after intraperitoneal ventral hernia treatment: a comparative study of protected versus unprotected meshes. Hernia 7:85–88
Cobb WS, Harris JB, Lokey JS, McGill ES, Klove KL (2003) Incisional herniorrhaphy with intraperitoneal composite mesh: a report of 95 cases. Am Surg 69:784–787
Koehler RH, Begos D, Berger D, Carey S, LeBlanc K, Park A, Ramshaw B, Smoot R, Voeller G (2003) Minimal adhesions to ePTFE mesh after laparoscopic ventral incisional hernia repair: reoperative findings in 65 cases. JSLS 7:335–340
Leber GE, Garb JL, Alexander AI, Reed WP (1998) Long-term complications associated with prosthetic repair of incisional hernias. Arch Surg 133:378–382
Jenkins ED, Yom V, Melman L, Brunt LM, Eagon JC, Frisella MM, Matthews BD (2010) Prospective evaluation of adhesion characteristics to intraperitoneal mesh and adhesiolysis-related complications during laparoscopic re-exploration after prior ventral hernia repair. Surg Endosc 24:3002–3007
Chelala E, Debardemaeker Y, Elias B, Charara F, Dessily M, Alle JL (2010) Eighty-five redo surgeries after 733 laparoscopic treatments for ventral and incisional hernia: adhesion and recurrence analysis. Hernia 14:123–129
Wassenaar EB, Schoenmaeckers EJ, Raymakers JT, Rakic S (2010) Subsequent abdominal surgery after laparoscopic ventral and incisional hernia repair with an expanded polytetrafluoroethylene mesh: a single institution experience with 72 reoperations. Hernia 14:137–142
Duffy AJ, Hogle NJ, LaPerle KM, Fowler DL (2004) Comparison of two composite meshes using two fixation devices in a porcine laparoscopic ventral hernia repair model. Hernia 8:358–364
McGinty JJ, Hogle NJ, McCarthy H, Fowler DL (2005) A comparative study of adhesion formation and abdominal wall ingrowth after laparoscopic ventral hernia repair in a porcine model using multiple types of mesh. Surg Endosc 19:786–790
Jacob BP, Hogle NJ, Durak E, Kim T, Fowler DL (2007) Tissue ingrowth and bowel adhesion formation in an animal comparative study: polypropylene versus proceed versus parietex composite. Surg Endosc 21:629–633
Gonzalez R, Rodeheaver GT, Moody DL, Foresman PA, Ramshaw BJ (2004) Resistance to adhesion formation: a comparative study of treated and untreated mesh products placed in the abdominal cavity. Hernia 8:213–219
Gaertner WB, Bonsack ME, Delaney JP (2010) Visceral adhesions to hernia prostheses. Hernia 14:375–381
Kayaoglu HA, Ozkan N, Hazinedaroglu SM, Ersoy OF, Erkek AB, Koseoglu RD (2005) Comparison of adhesive properties of five different prosthetic materials used in hernioplasty. J Invest Surg 18:89–95
Matthews BD, Mostafa G, Carbonell AM, Joels CS, Kercher KW, Austin C, Norton HJ, Heniford BT (2005) Evaluation of adhesion formation and host tissue response to intra-abdominal polytetrafluoroethylene mesh and composite prosthetic mesh. J Surg Res 123:227–234
Matthews BD, Pratt BL, Pollinger HS, Backus CL, Kercher KW, Sing RF, Heniford BT (2003) Assessment of adhesion formation to intra-abdominal polypropylene mesh and polytetrafluoroethylene mesh. J Surg Res 114:126–132
Novitsky YW, Harrell AG, Cristiano JA, Paton BL, Norton HJ, Peindl RD, Kercher KW, Heniford BT (2007) Comparative evaluation of adhesion formation, strength of ingrowth, and textile properties of prosthetic meshes after long-term intra-abdominal implantation in a rabbit. J Surg Res 140:6–11
Greenawalt KE, Butler TJ, Rowe EA, Finneral AC, Garlick DS, Burns JW (2000) Evaluation of Sepramesh biosurgical composite in a rabbit hernia repair model. J Surg Res 94:92–98
Acknowledgments
The authors acknowledge the efforts of Hilda Kabiru and Jocelyn Prowse at Atrium Medical Corporation for technical expertise and assistance with the scanning electron micrographs.
Disclosures
Dr. Deeken is a consultant for Atrium Medical Corporation and Davol Incorporated. Dr. Faucher is an employee of Atrium Medical Corporation. Dr. Matthews is a consultant for Atrium Medical Corporation and Ethicon Incorporated. He also receives honoraria and research/equipment support from Atrium Medical Corporation, Ethicon EndoSurgery, Karl Storz Endoscopy, Stryker Endoscopy, and W.L. Gore & Associates, Incorporated.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Deeken, C.R., Faucher, K.M. & Matthews, B.D. A review of the composition, characteristics, and effectiveness of barrier mesh prostheses utilized for laparoscopic ventral hernia repair. Surg Endosc 26, 566–575 (2012). https://doi.org/10.1007/s00464-011-1899-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1899-3