Abstract
Purpose
The number of elderly patients with colorectal cancer (CRC) treated with surgery has gradually increased. The aim of this study was to evaluate the short-term outcomes in patients ≥80 years of age who underwent laparoscopic or open surgery for CRC using a propensity score-matched analysis to make uniform the patient background characteristics affecting the postoperative morbidity and mortality.
Methods
We compared the short-term outcomes of open vs. laparoscopic surgery in patients with CRC ≥80 years of age between 2010 and 2015. Fifty-two patients undergoing laparoscopic colectomy for CRC were matched to 52 patients undergoing open colectomy with respect to gender, age, body mass index, performance status, prognostic nutritional index, Charlson Comorbidity Index score, tumor-node-metastasis stage, and tumor location. The operative time, blood loss, length of hospital stay, and postoperative complications were investigated.
Results
Blood loss was less during laparoscopic surgery than during open surgery (40 vs. 140 ml, p < 0.001). In the laparoscopic surgery group, the hospital stay was shorter (11 vs. 14 days, p < 0.001) and the morbidity rate lower (21.2 vs. 40.4%) than in the open surgery group. The mortality for both groups was similar (0 vs. 1.9% for laparoscopic surgery vs. open surgery).
Conclusion
Laparoscopic surgery in octogenarians with CRC is a safe, low-invasive alternative to open surgery with less blood loss and a shorter hospital stay.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An increase in the number of elderly people has been observed in Japan, the US, and Europe [1]. According to 2016 statistics, the proportion of the population ≥80 years of age (very elderly) is approximately 8.2%. Life expectancy is increasing, along with the number of elderly patients with surgically correctable diseases. Recent reports suggest that age per se in the absence of significant disease should not be considered a prognostic factor in gastrointestinal surgery [2].
Colorectal cancer (CRC) is one of the most common malignancies worldwide, and in recent years, its incidence rates in Japanese males have exceeded the peak incidence observed in the US, Canada, and New Zealand [3]. CRC is also the third-most common cause of cancer-related death in Japan, following lung cancer and gastric cancers. This results in an increasing proportion of elderly patients suffering from CRC becoming prospective candidates for surgery. As compared with open surgery, laparoscopic surgery has been proven to reduce hospitalization time, postoperative pain, and cardiopulmonary stress; to better preserve immune and metabolic responses; and to allow for an earlier return to routine activities [4,5,6]. The advantages of laparoscopic surgery may be more beneficial for elderly patients with comorbid conditions than open surgery [7]. Several studies have demonstrated that laparoscopic colorectal surgery (LCS) has superiority over traditional surgery in terms of the short-term outcomes and a substantial equality with regard to the functional and oncological results [8,9,10,11,12]. However, the number of randomized controlled trials is limited, and the literature lacks adequate information on the outcomes for elderly and/or high-risk patients who have undergone laparoscopic surgery. The diffusion of LCS for CRC in elderly patients is still limited, and published data lack sufficient supporting evidence. In the current situation, treatment decisions in aged patients with CRC depend on the policies of each institution and physician because no standard guidelines are available in Japan, Europe, or the US.
Therefore, the aim of this study was to evaluate the surgical outcomes of laparoscopic surgery as compared with those of open surgery for elderly patients ≥80 years of age with CRC in a single institution using a propensity score-matched analysis while considering patients’ background characteristics, such as their nutritional state, and their effects on postoperative morbidity and mortality.
Methods
Patients and methods
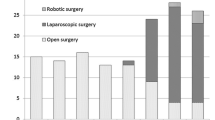
From 2010 to 2015, 158 consecutive colorectal cancer patients ≥80 years of age who underwent curative resection in Hiroshima City Asa Citizens Hospital were studied retrospectively. The exclusion criteria were synchronous CRC or distant metastasis; a medical history of other primary malignancy; combined operations for other disease; emergency operation; and/or the reception of preoperative chemotherapy, radiotherapy, or chemoradiotherapy. Of the 158 patients included in this study, 102 underwent laparoscopic surgery, and 56 underwent open surgery. Among the 158 patients, 104 were matched using propensity scoring. Data were collected in a prospectively maintained database that was supplemented by a retrospective chart review. This study was conducted with the approval of the ethics committee of Hiroshima City Asa Citizens Hospital (approval number: 29-2-9).
Perioperative factors were compared, including the operative time, blood loss, type of operation, conversion rate, postoperative morbidity, mortality, postoperative hospital stay, and readmission within 30 days. Conversion to open operation was defined as an abdominal incision larger than necessary for specimen retrieval. The results of a pathological examination were classified according to the tumor-node-metastasis (TNM) classification of the International Union Against Cancer (UICC). The patient characteristics assessed were the age, gender, body mass index (BMI), Eastern Cooperative Oncology Group (ECOG) performance status (PS), prognostic nutritional index (PNI), Charlson Comorbidity Index score, pathological TNM stage, and tumor location. The PNI was calculated based on the serum albumin concentration (Alb) and total lymphocyte count of the peripheral blood (TLC), which was calculated using the following formula: 10 × Alb + 0.005 × TLC.
Postoperative management was the same for both surgery groups. Patients were discharged when they had sufficient oral intake, no complications or well-controlled complications, and no excessive anxiety about discharge from the hospital. Short-term morbidity and mortality were defined as 30-day or in-hospital morbidity and mortality. Tumor stage was based on the final pathologic assessment. Tumor location was divided into three areas: right colon, left colon, and rectum. The right colon was defined as the cecum, ascending colon, hepatic flexure colon, and transverse colon; the left colon was defined as the splenic flexure colon, descending colon, and sigmoid colon. Complications designated as more severe than grade I according to the Clavien–Dindo classification system were categorized as wound infection, ileus, delirium, anastomotic leakage, pneumonia, intra-abdominal bleeding, heart failure, urinary tract infection, voiding difficulty, or cholecystitis [13].
Statistical analyses
For categorical variables, data were presented as frequencies and percentages, and the Fisher’s exact probability test or Chi-square test was applied to evaluate the significance of differences in proportions. Continuous variables were presented as mean ± standard deviation (SD) or medians (from minimum value to maximum value) and were estimated using the Mann–Whitney U test or a t test. Associations were considered significant when p < 0.05. The survival time was measured from the surgery for CRC to the date of last follow-up or death. The Kaplan–Meier method was used to construct survival curves.
A propensity score matching analysis was performed using logistic regression analysis to create a propensity score for the laparoscopic and open operation groups with a logistic regression model. The following variables were entered into the propensity model: gender, age, BMI, ECOG PS, PNI, Charlson Comorbidity Index score, TNM stage, and tumor location. Subsequently, a one-to-one match between the two groups was obtained using nearest neighbor matching with a caliper method. All statistical analyses were performed using the JMP 13 software program (SAS Institute Inc., Cary, NC, USA).
Results
Baseline characteristics
Of the 158 patients included in this study, 35.4% (56/158) underwent open resection, and 64.6% (102/158) underwent laparoscopic resection. The median age of the patients was 85 years, and there were 71 males and 87 females. More than two-thirds of patients had some kind of comorbidity. The midterm outcomes (the 3-year overall survival and relapse-free survival) are shown by tumor stage in Figs. 1 and 2. After performing propensity score matching for the entire study population, 52 matched pairs of patients were selected. The baseline characteristics of the pre- and post-matching groups are outlined in Table 1. Before matching, there were differences between the two groups. The patients tended to be older in the open (OP) group than in the laparoscopic (LP) group (p = 0.06). The BMI tended to be higher in the LP group than in the OP group (p = 0.09). The ECOG PS and PNI tended to be lower in the OP group than in the LP group (p = 0.08, 0.07). Tumor stage was higher in the OP group than in the LP group (p = 0.01). After matching, the two groups were well balanced in terms of gender, age, BMI, ECOG PS, PNI, Charlson Comorbidity Index score, tumor location, and stage of the tumor.
Short-term outcomes
Operative outcomes in the matched cohorts are presented in Table 2. The type of operation did not statistically differ between the two groups. The operative time was longer in the LP group than in the OP group (222 vs. 168 min, p = 0.002). Blood loss was greater in the OP group than in the LP group (140 vs. 40 ml, p < 0.001). Blood transfusion was performed more frequently in the OP group than in LP group. Conversion to open surgery was necessary in 3 (5.8%) LP patients; adhesion after appendectomy, right accessary colic vein injury, and superior mesenteric vein injury occurred in 1 patient each. With regard to oncological outcomes, the extent of lymph node dissection, number of retrieved lymph nodes, length of resected bowel, proximal resection margin, distal resection margin, and radial margin were not statistically different between the two groups.
Postoperative recovery, morbidity, and mortality data are presented in Table 3. Overall postoperative complications occurred in 40.4 and 21.2% of the OP and LP groups, respectively (p = 0.03). The LAP group had a significantly lower rate of grade I wound infection than the OP group (3.9 vs. 17.3%, p = 0.02). Grade II or higher complications occurred in 25 and 17.3% of the OP and LP groups, respectively (p = 0.34). In the OP group, the most common morbidity was wound infection in 12 patients (23.1%), followed by postoperative ileus in 6 patients (11.5%), and delirium in 4 patients (7.7%). In the LP group, the most common morbidity was wound infection in 6 patients (11.5%), followed by postoperative ileus in 4 patients (7.7%) and delirium in 2 patients (3.9%). There was one 30-day postoperative mortality in the OP group because of heart failure. The length of postoperative hospital stay was also shorter in the LP group than in the OP group (9.0 vs. 10.0 days, p < 0.001). One (1.9%) and 2 patients (3.9%) required hospital readmission within 30 days in the OP and LAP group, respectively; ileus occurred in 2 patients, and enterocutaneous fistula occurred in 1 patient.
Discussion
This single-institutional, propensity score-matched study compared the short-term outcomes for elderly patients who underwent either laparoscopic or open resection for CRC. Our results suggested that LCS in octogenarian patients achieved better short-term outcomes than open surgery.
LCS has been shown to lead to better short-term outcomes than open surgery in general, and a long-term analysis after LCS has highlighted that its oncological outcomes are substantially comparable to those following open surgery, definitively validating the minimally invasive treatment of cancers of the colon and, more recently, of the rectum [14–17]. In Japan, the Japan Clinical Oncology Group (JCOG) conducted a randomized trial to compare the oncological outcomes between patients who underwent LCS and open surgery for stage II/III CRC [18, 19]. A total of 1050 patients were registered, and the short-term outcomes were the same between the LCS and open surgery groups, while the long-term results were similar. Despite these outcomes, LCS is still much less widespread in the elderly than in younger patients because elderly patients tend to be excluded from randomized controlled trials.
Several retrospective studies comparing the outcomes of LCS to those of open surgery for elderly patients found that LCS may be of benefit to elderly patients, as it results in shorter admission duration, earlier recovery, less pain, and, ultimately, lower mortality and morbidity rates than open surgery, with the presupposition that these procedures are performed by surgeons experienced in the technique [12, 20,21,22,23,24,25]. Furthermore, the long-term results of a few prospective randomized trials comparing LCS and open surgery for CRC have been published in recent years [11, 26]. LCS for CRC in elderly patients has short-term benefits in terms of an earlier recovery of the bowel function and a shorter length of hospital stay than open surgery. However, reports on very elderly patients (≥80 years of age) with CRC are rare.
A case-matched retrospective study compared the outcomes for 71 patients >80 years of age after LCS with those for the same number of patients undergoing open surgery and reported a faster recovery of bowel function (3.0 vs. 4.0 days, p < 0.001), a shorter hospital stay (9.0 vs. 10.0 days, p = 0.037), a lower rate of postoperative complications (22.5 vs. 40.8%, p = 0.019) and an equivalent long-term prognosis in the LCS group than in the open surgery group [20]. A multicenter-matched case–control study in Japan reported that the complication rates of LCS were lower than those of open surgery (24.9 vs. 36.3%, p < 0.001) in CRC patients >80 years of age [27]. A randomized control study that compared the outcomes for elderly patients ≥75 years of age after LCS with those of patients undergoing open surgery showed that LCS resulted in a shorter hospital stay (10.0 vs. 13.0 days, p = 0.026) and a lower rate of postoperative complications (22.5 vs. 39.4%, p = 0.029) than open surgery [26].
In contrast, however, several studies have reported similar rates of postoperative complications between LCS and open surgery in elderly patients [23, 28]. A propensity score matching analysis comparing the short-term outcomes after LCS between elderly and younger patients reported that the rate of postoperative complications and length of hospital stay did not differ markedly between the two age groups [29]. A systematic review targeting CRC elderly patients identified 15 studies that discussed 1436 LCS and 1810 open surgery procedures. Among the short-term outcomes, blood loss was greater and morbidity, incisional surgical site infection, bowel obstruction, and cardiovascular complications more frequent in patients who underwent open surgery than in those who underwent LCS, although the operation time was shorter in the open surgery group. There were no significant differences in the long-term outcomes. The review concluded that LCS is an effective procedure for elderly patients with CRC [30].
Consistent with most previous reports, our study showed a lower frequency of morbidity and a shorter length of hospital stay for the LCS group than for the open surgery group. There were no significant differences in rates of complications, probably due to the relatively small number of subjects in our study. However, wound infection tended to more frequently occur in the OP group than in the LP group. Reports on the incidence of wound infection have varied in previous studies. Studies in elderly CRC patients reported that the incidence of wound infection was 6.7–8.1% in the LCS group and 10.2–16.1% in the OCS group [7, 20, 23]. In the present study, 102 CRC patients ≥80 years of age underwent laparoscopic surgery, with conversion to open surgery required in only 4 cases (3.9%) due to extensive adhesion and vessel injury. The conversion rate in our study was comparable to that of other trials [14, 17] and studies including elderly patients [12, 20, 31].
Beyond all of the factors that affect the postoperative morbidity and mortality, the nutritional state of a patient is the most important [32]. The predictive value of the PNI for postoperative complications is widely accepted in various solid organ cancers, including gastrointestinal cancer [33,34,35]. In patients with CRC who are undergoing primary tumor resection, it has been shown that a weight loss of greater than 10% prior to surgery [36] and undernutrition [37] are mortality risk factors, and that a low preoperative PNI predicts severe complications, recurrence, and a poor prognosis [38, 39]. Therefore, it is important that a patient’s nutritional status be evaluated prior to surgery, especially in elderly patients. However, there are no propensity score-matched analyses that have compared the short-term outcomes of LCS and open surgery considering nutritional status as a matching factor. In all cases of the present study, the PNI of patients who underwent open surgery tended to be lower than that of patients who underwent LCS, which may result in bias in baseline characteristics. Therefore, we conducted a propensity score-matched analysis comparing LCS and open surgery in elderly patients, including the PNI as matching factor.
Several limitations associated with the present study warrant mention. First, this study was conducted at a single institute. The impact of this study is thus lower than that of a large-scale multicenter trial. Second, the data on patient recovery during the early postoperative period were not evaluated in the present study except for the length of postoperative hospital stay, because we performed postoperative management according to clinical pathways in that the intake of liquids and dietary was started on the same postoperative day in patients who underwent both LCS and open surgery. Therefore, we believe that the data on patient recovery during the early postoperative period do not reflect early bowel recovery. Third, this study was an analysis of early results; the long-term results remain unknown. Oncological long-term outcomes are most important in clarifying the true feasibility of laparoscopic surgery. We will report long-term results when the observation period is sufficiently long.
Conclusion
Compared with open surgery, LCS resulted in benefits for octogenarians with CRC in terms of the short-term results. LCS might result in a reduction in postoperative complications and a shortening of the postoperative hospital stay.
References
Kordatou Z, Kountourakis P, Papamichael D. Treatment of older patients with colorectal cancer: a perspective review. Ther Adv Med Oncol. 2014;6:128–40.
Weber DM. Laparoscopic surgery: an excellent approach in elderly patients. Arch Surg. 2003;138:1083–8.
Kashino I, Mizoue T, Tanaka K, Tsuji I, Tamakoshi A, Matsuo K, et al. Vegetable consumption and colorectal cancer risk: an evaluation based on a systematic review and meta-analysis among the Japanese population. Jpn J Clin Oncol. 2015;45:973–9.
Gupta A, Watson DI. Effect of laparoscopy on immune function. Br J Surg. 2001;88:1296–306.
Milsom JW, Hammerhofer KA, Bohm B, Marcello P, Elson P, Fazio VW. Prospective, randomized trial comparing laparoscopic vs. conventional surgery for refractory ileocolic Crohn’s disease. Dis Colon Rectum. 2001;44:1–8 (discussion 9).
Zucker KA, Pitcher DE, Martin DT, Ford RS. Laparoscopic-assisted colon resection. Surg Endosc. 1994;8:12–7 (discussion 8).
Frasson M, Braga M, Vignali A, Zuliani W, Di Carlo V. Benefits of laparoscopic colorectal resection are more pronounced in elderly patients. Dis Colon Rectum. 2008;51:296–300.
Schwenk W, Haase O, Neudecker J, Muller JM. Short term benefits for laparoscopic colorectal resection. Cochrane Database Syst Rev. 2005;3:CD003145.
Kuhry E, Schwenk WF, Gaupset R, Romild U, Bonjer HJ. Long-term results of laparoscopic colorectal cancer resection. Cochrane Database Syst Rev. 2008;2:003432.
Breukink S, Pierie J, Wiggers T. Laparoscopic versus open total mesorectal excision for rectal cancer. Cochrane Database Syst Rev. 2006;4:CD005200.
Roscio F, Boni L, Clerici F, Frattini P, Cassinotti E, Scandroglio I. Is laparoscopic surgery really effective for the treatment of colon and rectal cancer in very elderly over 80 years old? A prospective multicentric case–control assessment. Surg Endosc. 2016;30:4372–82.
Nishikawa T, Ishihara S, Hata K, Murono K, Yasuda K, Otani K, et al. Short-term outcomes of open versus laparoscopic surgery in elderly patients with colorectal cancer. Surg Endosc. 2016;30:5550–7.
Katayama H, Kurokawa Y, Nakamura K, Ito H, Kanemitsu Y, Masuda N, et al. Extended Clavien–Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today. 2016;46:668–85.
Colon Cancer Laparoscopic or Open Resection Study G, Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, et al. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 2009;10:44–52.
Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ. Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg. 2010;97:1638–45.
Lacy AM, Delgado S, Castells A, Prins HA, Arroyo V, Ibarzabal A, et al. The long-term results of a randomized clinical trial of laparoscopy-assisted versus open surgery for colon cancer. Ann Surg. 2008;248:1–7.
Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB, et al. Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol. 2014;15:767–74.
Yamamoto S, Inomata M, Katayama H, Mizusawa J, Etoh T, Konishi F, et al. Short-term surgical outcomes from a randomized controlled trial to evaluate laparoscopic and open D3 dissection for stage II/III colon cancer: Japan Clinical Oncology Group Study JCOG 0404. Ann Surg. 2014;260:23–30.
Kitano S, Inomata M, Mizusawa J, Katayama H, Watanabe M, Yamamoto S, et al. Survival outcomes following laparoscopic versus open D3 dissection for stage II or III colon cancer (JCOG0404): a phase 3, randomised controlled trial. Lancet Gastroenterol Hepatol. 2017;2:261–8.
Moon SY, Kim S, Lee SY, Han EC, Kang SB, Jeong SY, et al. Laparoscopic surgery for patients with colorectal cancer produces better short-term outcomes with similar survival outcomes in elderly patients compared to open surgery. Cancer Med. 2016;5:1047–54.
She WH, Poon JT, Fan JK, Lo OS, Law WL. Outcome of laparoscopic colectomy for cancer in elderly patients. Surg Endosc. 2013;27:308–12.
Lian L, Kalady M, Geisler D, Kiran RP. Laparoscopic colectomy is safe and leads to a significantly shorter hospital stay for octogenarians. Surg Endosc. 2010;24:2039–43.
Vignali A, Di Palo S, Tamburini A, Radaelli G, Orsenigo E, Staudacher C. Laparoscopic vs. open colectomies in octogenarians: a case-matched control study. Dis Colon Rectum. 2005;48:2070–5.
Mukai T, Akiyoshi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, et al. Outcomes of laparoscopic surgery for colorectal cancer in oldest-old patients. Surg Laparosc Endosc Percutan Tech. 2014;24:366–9.
Tominaga T, Takeshita H, Arai J, Takagi K, Kunizaki M, To K, et al. Short-term outcomes of laparoscopic surgery for colorectal cancer in oldest-old patients. Dig Surg. 2015;32:32–8.
Fujii S, Ishibe A, Ota M, Yamagishi S, Watanabe K, Watanabe J, et al. Short-term results of a randomized study between laparoscopic and open surgery in elderly colorectal cancer patients. Surg Endosc. 2014;28:466–76.
Hinoi T, Kawaguchi Y, Hattori M, Okajima M, Ohdan H, Yamamoto S, et al. Laparoscopic versus open surgery for colorectal cancer in elderly patients: a multicenter matched case-control study. Ann Surg Oncol. 2015;22:2040–50.
Tan WS, Chew MH, Lim IA, Ng KH, Tang CL, Eu KW. Evaluation of laparoscopic versus open colorectal surgery in elderly patients more than 70 years old: an evaluation of 727 patients. Int J Colorectal Dis. 2012;27:773–80.
Shiga M, Maeda H, Oba K, Okamoto K, Namikawa T, Fujisawa K, et al. Safety of laparoscopic surgery for colorectal cancer in patients over 80 years old: a propensity score matching study. Surg Today. 2017;47:951–8.
Fujii S, Tsukamoto M, Fukushima Y, Shimada R, Okamoto K, Tsuchiya T, et al. Systematic review of laparoscopic vs open surgery for colorectal cancer in elderly patients. World J Gastrointest Oncol. 2016;8:573–82.
Inoue Y, Kawamoto A, Okugawa Y, Hiro J, Saigusa S, Toiyama Y, et al. Efficacy and safety of laparoscopic surgery in elderly patients with colorectal cancer. Mol Clin Oncol. 2015;3:897–901.
Blanc-Bisson C, Fonck M, Rainfray M, Soubeyran P, Bourdel-Marchasson I. Undernutrition in elderly patients with cancer: target for diagnosis and intervention. Crit Rev Oncol Hematol. 2008;67:243–54.
Nozoe T, Kimura Y, Ishida M, Saeki H, Korenaga D, Sugimachi K. Correlation of pre-operative nutritional condition with post-operative complications in surgical treatment for oesophageal carcinoma. Eur J Surg Oncol. 2002;28:396–400.
Kanda M, Fujii T, Kodera Y, Nagai S, Takeda S, Nakao A. Nutritional predictors of postoperative outcome in pancreatic cancer. Br J Surg. 2011;98:268–74.
Watanabe M, Iwatsuki M, Iwagami S, Ishimoto T, Baba Y, Baba H. Prognostic nutritional index predicts outcomes of gastrectomy in the elderly. World J Surg. 2012;36:1632–9.
Alves A, Panis Y, Mathieu P, Mantion G, Kwiatkowski F, Slim K, et al. Postoperative mortality and morbidity in French patients undergoing colorectal surgery: results of a prospective multicenter study. Arch Surg. 2005;140:278–83 (discussion 84).
Gupta D, Lammersfeld CA, Burrows JL, Dahlk SL, Vashi PG, Grutsch JF, et al. Bioelectrical impedance phase angle in clinical practice: implications for prognosis in advanced colorectal cancer. Am J Clin Nutr. 2004;80:1634–8.
Tokunaga R, Sakamoto Y, Nakagawa S, Miyamoto Y, Yoshida N, Oki E, et al. Prognostic nutritional index predicts severe complications, recurrence, and poor prognosis in patients with colorectal cancer undergoing primary tumor resection. Dis Colon Rectum. 2015;58:1048–57.
Mohri Y, Inoue Y, Tanaka K, Hiro J, Uchida K, Kusunoki M. Prognostic nutritional index predicts postoperative outcome in colorectal cancer. World J Surg. 2013;37:2688–92.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
There was no funding supporting this study.
Conflict of interest
The authors declare that they have no conflict of interests.
Rights and permissions
About this article
Cite this article
Miguchi, M., Yoshimitsu, M., Hakoda, K. et al. Short-term outcomes of laparoscopic surgery in octogenarians with colorectal cancer: a single-institution analysis. Surg Today 48, 292–299 (2018). https://doi.org/10.1007/s00595-017-1584-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-017-1584-9