Abstract
Background
In patients in whom attempted endoscopic stenting of malignant biliary obstruction fails, combined percutaneous–endoscopic stenting and percutaneous stenting using expandable metallic endoprostheses offer alternative approaches to biliary drainage. Despite the popularity of the percutaneous route, there is no available evidence to support its superiority over combined stenting in this patient group. The objective of this study was to present the short- and long-term results of a large series of combined percutaneous–endoscopic stenting procedures and identify factors associated with adverse outcome.
Methods
Data were retrospectively collected on patients undergoing combined percutaneous–endoscopic biliary stenting for malignant biliary obstruction between January 2002 and December 2006. Short- and long-term outcomes were recorded, and pre-procedure variables correlated with adverse outcome.
Results
Combined biliary stenting was technically successful in 102 (96.2%) of 106 patients. Procedure-associated mortality rate was 0%. In-hospital morbidity and mortality rates were 24.5% and 16.7%, respectively, with the majority of deaths resulting from biliary sepsis. Median survival was 100 days, with a 13.7% stent occlusion rate. On multivariable analysis, baseline American Society of Anaesthesiologists (ASA) grade, decreasing serum albumin and increasing leucocyte count were independently associated with in-hospital mortality following combined stenting.
Conclusion
Combined biliary stenting is associated with short- and long-term outcomes equal to those reported in recent series of percutaneous transhepatic stenting. Randomised control trials, including cost-effectiveness analyses, are required to further compare these techniques. Outcomes following combined stenting may be further improved by early recognition and treatment of sepsis and scrupulous management of co-morbid disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In patients with malignant biliary obstruction, biliary drainage may be achieved by three principal methods: endoscopic stenting, percutaneous transhepatic stenting and surgical bypass. Recent meta-analyses have suggested that endoscopic stenting provides superior results to both open surgical bypass [1, 2] and the transhepatic placement of non-expandable metallic stents [3]. Whilst the advent of expandable endoprostheses, which can be placed over a transhepatic track of narrower diameter, has led to increasing use of the transhepatic route [4–11], the endoscopic approach remains the first-line stenting technique in most centres.
A proportion of patients fail attempted endoscopic stenting, mainly due to anatomical distortion as a consequence of tumour size and/or dissemination. In this subgroup, stenting may be attempted either by the percutaneous transhepatic method or by a repeat endoscopic procedure with assistance provided to the endoscopist by the passage of a narrow-diameter percutaneous transhepatic guidewire across the stricture, over which a stent may then be placed (a combined or rendezvous procedure) [12]. This latter technique enables the passage of either plastic or metallic stents, using a smaller transhepatic puncture site than that required for percutaneous stenting, but requires an additional endoscopic procedure.
There is currently no evidence to demonstrate superiority of either combined stenting or percutaneous transhepatic stenting in patients with malignant biliary obstruction in whom initial endoscopic stenting fails. Available evidence is provided by individual non-comparative series, with no randomised control trial evidence available. Data for combined procedures are limited, with studies including small numbers of patients and assessing limited outcomes [12–17]. Recent studies have reported short-term outcomes comparable to those of percutaneous stenting, with 30-day mortality rates of 12–14.8% [13, 17], with few data available regarding long-term outcomes such as stent occlusion and survival. The primary aim of this study was to report the short- and long-term outcomes of combined biliary stenting, using the experience of a high-volume tertiary referral hepatobiliary centre.
Endoscopic, percutaneous and combined biliary stenting in patients with malignant disease are all associated with significant rates of in-hospital morbidity and mortality. Factors associated with adverse outcome have been explored in patients with malignant biliary obstruction undergoing surgical bypass [18–22], endoscopic stenting [19, 23] and percutaneous stenting [8, 24]. However, save for the performance of preceding biliary drainage [17], they have not been examined in the context of combined stenting. The secondary aim of this paper was, therefore, to perform a comprehensive analysis to identify pre-procedure variables associated with adverse outcome following combined percutaneous–endoscopic stenting, in an effort to improve procedure-associated risk.
Patients and methods
The study included all patients undergoing attempted combined biliary stenting at our institution over a 5-year period (January 2002 to December 2006). Patients who had an obstructed biliary system on ultrasonography and the biochemical features of biliary obstruction (elevated bilirubin and alkaline phosphatase) were selected for combined biliary stenting if endoscopic retrograde cholangiopancreatography (ERCP) had failed to relieve the obstruction despite the second part of the duodenum being accessible. At initial ERCP, techniques including needle-knife papillotomy, tapered-tip catheters and polymer-coated guidewires had been utilised without success.
Patients transferred to our institution following failed endoscopic stenting at another hospital routinely underwent a further attempt at endoscopic drainage following transfer, prior to undergoing a combined procedure. Similarly, the majority of patients who failed initial ERCP at our institution underwent a repeat attempt several days later by a different operator, unless technical factors at the time of initial endoscopy had suggested little hope of subsequent success or expedient percutaneous drainage was required to treat biliary sepsis.
Prior to the procedure, a single dose of prophylactic antibiotics and sedation with morphine and benzodiazepines were administered as routine. The transhepatic stage of the procedure was performed by a consultant radiologist. Local anaesthetic was used at the percutaneous puncture site, following which a standard technique [25] was used to place the guidewire across the site of biliary obstruction. The size of the transhepatic track was kept to a minimum and was usually 6-French. The endoscopic stage of the procedure was performed by a consultant surgeon or gastroenterologist using a video duodenoscope. Following endoscopic identification of the percutaneous guidewire, a 10-French polytetrafluoroethylene (PTFE) biliary stent was placed across the obstruction and the position checked on screening. Patient recovery took place on a surgical ward, with discharge home dependent on the appropriate support being in place.
Pre-procedure data and information regarding post-procedure outcomes were extracted from patient case notes and computerised records. The following pre-procedure parameters were recorded: age, gender, route of admission, baseline ASA grade, underlying pathology, site of stricture, biliary drainage (external or internal–external) prior to combined stenting, interval between index ERCP and biliary drainage (external or internal), interval between index ERCP and stent placement, presence of sepsis pre-procedure, pre-procedure serum biochemical parameters (urea, creatinine, bilirubin, alkaline phosphatase, albumin) and pre-procedure haematological parameters (haemoglobin, leucocyte count, platelet count).
ASA grade was taken as the patient’s baseline physiological status prior to the development of obstructive jaundice. Site of stricture was classified as upper, middle or lower third of the biliary tree dependent upon radiological findings. The value recorded for each biochemical and haematological variable was the most abnormal value within the 48-h period prior to combined stenting. Pre-procedure sepsis was considered to be present if infection was suspected or proven and two or more systemic inflammatory response syndrome (SIRS) criteria were met (heart rate >90 beats per minute, body temperature <36°C or >38°C, respiratory rate >20 breaths per minute, leucocyte count >12 × 109 cells/L or <4 × 109 cells/L or greater than 10% band forms) [26].
As previously, technical success was defined as the successful deployment of the stent in the appropriate position resulting in drainage of the stented bile ducts, and clinical success was defined as a decrease in serum bilirubin level of more than 20% relative to the pre-procedure level within 1 week of stent insertion [5, 27]. Short-term outcome measures were in-hospital morbidity, 30-day mortality and in-hospital mortality.
Long-term outcome measures assessed were stent occlusion and overall survival rates. Patients who developed recurrent jaundice and/or symptoms of sepsis following discharge were readmitted. Cholangitis was treated aggressively with intravenous antibiotics and, when dilatation of the biliary tree was confirmed, patients underwent restenting. Date of death was determined from case notes, computerised records and death certificates.
Statistics
Chi-squared and Fisher’s exact tests were used to analyse for significant associations and differences between subgroups within the cohort. Where variables did not follow a normal distribution, the Mann–Whitney U test was applied. Categorical pre-procedure variables were correlated with in-hospital morbidity and mortality using the chi-square test or Fisher’s exact test as appropriate. Continuous variables were compared with outcome using binary logistic regression analysis. Multivariable analysis was performed using a stepwise binary logistic regression model, including all variables with P < 0.10 on univariate analysis. Pre-procedure variables were correlated with long-term survival by entry into a Kaplan–Meier model and application of the log-rank test. Continuous variables were dichotomised using the median for this analysis. Statistical significance was defined as P < 0.05. Statistical analyses were performed using the Statistical Package for the Social Sciences 14.0® (SPSS, Chicago, IL).
Results
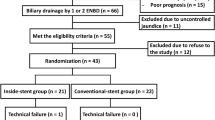
Over the study period, 2,201 patients required biliary stenting for all indications. This was performed successfully at ERCP in 2,058 cases (93.5%), with 143 patients failing endoscopic stenting, of whom 118 proceeded to attempted combined stenting. One hundred and six of these patients had malignancy and 12 had benign disease. Of patients undergoing combined stenting for malignant disease, the initial endoscopic procedure failed due to inability to cannulate the common bile duct in 50 cases and inability to cross the stricture in 56 cases. Twenty-five patients were unsuitable for a combined procedure due to inability to intubate the duodenum and underwent attempted percutaneous stenting.
Combined biliary stenting was technically successful in 102 of the 106 patients (96.2%) with malignancy. Pre-procedure demographic and clinicopathological variables for these patients are shown in Table 1. The aetiology of low biliary strictures was carcinoma of the pancreas (n = 34), cholangiocarcinoma (n = 3) and ampullary carcinoma (n = 2). The aetiology of mid biliary strictures was carcinoma of the pancreas (n = 15), cholangiocarcinoma (n = 4) and metastases (n = 6). The aetiology of high/hilar biliary strictures was cholangiocarcinoma (n = 23), metastases (n = 14) and gallbladder cancer (n = 1).
Combined stenting was technically successful at the first attempt in 98 cases, with a repeat attempt necessary to achieve stent placement in 4 cases. In 39 patients, biliary drainage (external or external–internal) was performed prior to combined stenting (median 7 days before, range 1–53 days). Indications included injection of contrast above the stricture at ERCP (n = 10), profound hyperbilirubinaemia and/or sepsis (n = 25) and as part of a failed combined procedure (n = 4).
Combined biliary stenting could not be achieved in four patients (3.8%). In all cases this related to failure of the percutaneous part of the procedure and was due to inability to specifically cannulate the ducts (n = 1) or inability to traverse the stricture with the guidewire (n = 3). Failure was unrelated to stricture type or location. Of these patients, one was left with an external biliary drain and three underwent a surgical bypass procedure. In-hospital morbidity and mortality of this group was not significantly different from that of patients who underwent successful combined stenting.
Including technically unsuccessful procedures, combined stenting was clinically successful, leading to a decrease in serum bilirubin level of more than 20%, in 94.3% of cases (n = 100). Early stent occlusion and stent migration each occurred in one case (diagnosed at 6 and 8 days post-procedure, respectively). Both episodes were associated with the development of sepsis and were treated by endoscopic restenting.
In-hospital mortality and morbidity
In-hospital morbidity occurred in 24.5% of cases (n = 25) and was deemed to be definitely or probably procedure related in five cases (4.9%) (Table 2). All patients who developed biliary sepsis following combined stenting had evidence of sepsis or an elevated leucocyte count prior to the combined procedure. Similarly, all patients who developed renal failure had deranged renal function prior to stenting. These complications were not, therefore, deemed to be procedure related.
Of patients undergoing successful combined biliary stenting, 16.7% (n = 17) died within 30 days of the procedure (Table 3). No in-hospital death occurred later than 30 days, and in-hospital mortality was, therefore, also 16.7%. The principal causes of death were biliary sepsis (n = 8) and renal failure (n = 3), with no death deemed to be procedure related. The aetiology of biliary strictures in patients dying in hospital following combined stenting for malignant disease was as follows: carcinoma of the pancreas (n = 7), cholangiocarcinoma (n = 8) and metastatic disease (n = 2). In-hospital mortality and morbidity rates for patients with benign disease were 0% and 16.6%, respectively.
Factors associated with in-hospital morbidity
The results of univariate analyses of pre-procedure variables for their influence on morbidity are shown in Table 4. Factors associated with morbidity were increasing age, decreasing serum albumin, increasing serum urea, increasing serum creatinine, decreasing serum haemoglobin, increasing leucocyte count and presence of sepsis pre-procedure. Increasing baseline ASA grade also showed a borderline significant association with morbidity.
On multivariable analysis, the presence of sepsis pre-procedure and increasing leucocyte count were the only variables independently associated with morbidity following combined stenting (Table 5).
Factors associated with in-hospital mortality
The results of univariate analyses of pre-procedure variables for their influence on in-hospital mortality are shown in Table 4. Factors associated with mortality were increasing age, increasing baseline ASA grade, increasing serum bilirubin, decreasing serum albumin, increasing serum urea, increasing serum creatinine, decreasing serum haemoglobin, increasing leucocyte count and presence of pre-procedure sepsis.
On multivariable analysis, baseline ASA grade, decreasing serum albumin and increasing leucocyte count were independently associated with in-hospital mortality (Table 5).
Long-term outcomes
Stent occlusion developed in 13.7% of cases (n = 14), leading to readmission in all cases. Occlusion occurred at a median of 100 days following stent placement (range 6–200 days). Twelve patients underwent endoscopic restenting, one patient required use of the combined technique and one patient refused further treatment. No clinicopathological factor, including stricture site or type, predicted stent occlusion.
Median survival following combined stenting for malignancy was 100 days (range 2–800 days). Five patients subsequently underwent tumour resection and at 2 years post-resection, two of these patients remained disease free, two were alive with inoperable recurrence and one had died. Median survival in patients not proceeding to surgery (n = 97) was 98 days (range 2–240 days). Twenty of these patients were alive at 6 months following combined stenting. None of the pre-procedure variables assessed predicted long-term survival in patients with malignant disease who survived the initial hospital episode.
Discussion
The current study confirms that the combined technique is associated with rates of technical (96.2%) and clinical (94.3%) success equal to or exceeding results reported for percutaneous stenting of malignant biliary obstruction [4–11]. Whilst endoscopic placement of stents is generally accepted to be more difficult with proximal obstruction, efficacy of the combined technique, in agreement with a previous study [14], was unrelated to stricture location or type. The rates of procedure-associated mortality (0%) and morbidity (4.9%) are the lowest reported for this technique [12–17] and are equal to reported results of percutaneous stenting [4–11].
The in-hospital morbidity (24.5%) and mortality (16.7%) rates reported in this study are in line with other reports of this technique [12–17]. Deaths arose primarily from biliary sepsis and renal failure, with evidence of these derangements preceding stent placement in all cases. Whilst these mortality and morbidity rates are significant, they must be taken in the context of the patient group undergoing the procedure and results reported for other methods of biliary stenting in this group. A recent meta-analysis reported a 9.8% 30-day mortality rate amongst patients with malignant biliary obstruction successfully stented with endoscopy alone [1]. Patients undergoing combined stenting represent a distinct subgroup of patients with malignant biliary obstruction, however, tending to have more advanced disease and having undergone one or more failed attempts at endoscopic stenting prior to the definitive drainage procedure.
Objective comparison of the current data with series of percutaneous metallic stenting is confounded by the use of the latter technique as the index procedure, rather than as a second-line therapy following failed endoscopic stenting, in many series [5, 6, 9, 11]. Recent series of percutaneous stenting as first-line therapy have reported in-hospital mortality and morbidity rates of 9–13.2% and 28%, respectively [5, 6]. While these results are comparable with those of the current study, a more relevant comparison is provided by the recent UK series of Indar et al. [7]. This study of percutaneous Wallstent® placement used a patient population similar to that examined in the current study, 87% of whom had previously failed attempted endoscopic stenting, and reported 30-day mortality and morbidity rates of 20% and 30%, respectively. Performance of prior endoscopic intervention must be considered, therefore, when comparing results of percutaneous series with those using the combined technique.
A recent meta-analysis of trials examining patients stented endoscopically for predominantly mid and lower malignant biliary obstruction reported median survival of 99–175 days [1]. Recent series of percutaneous stenting reported median survival of 97–134 days [4–7], with a median of 105 days in patients who had failed attempted endoscopic stenting prior to the percutaneous procedure [7]. The median survival of 100 days in the current study is in line with these results. The short survival of patients failing initial endoscopic stenting results from a combination of a high in-hospital mortality rate coupled with advanced disease stage, and occurred despite the aggressive treatment of recurrent obstruction and/or sepsis.
The 13.7% occlusion rate observed in this study is within the 12–18% range reported in recent series of percutaneous metallic stenting [5–7], in the context of similar median survival times. Whilst studies of endoscopic stenting found metallic stents to have long-term patency superior to plastic stents, this benefit was not apparent until at least 3 months following insertion [1]. Available data for both the combined and percutaneous stenting techniques suggest that the majority of patients die before the reported patency benefits of metallic stents can become clinically apparent.
In summary, therefore, the short- and long-term results of combined biliary stenting reported here are equivalent to those reported following percutaneous, transhepatic placement of metallic stents. In addition to providing equivalent palliation, the combined technique offers several potential benefits over the percutaneous route. Whilst both techniques allow the placement of expandable metallic stents, the combined technique also allows the placement of large-bore plastic (e.g. PTFE) endoprostheses. These stents are significantly easier to replace following stent occlusion and are easier to remove in patients who later proceed to surgical intervention. Plastic stents also cost approximately 15–40 times less than expandable metallic stents and may, therefore, be a more rationale choice in patients with limited life expectancy due to terminal malignancy.
Previous cost-effectiveness analyses of endoscopic stenting favoured metallic stents only in patients who survived in excess of 6 months, with no difference in cost if survival was less than 6 months and a higher cost per patient for metallic stents when patients survived less than 3 months [23, 28, 29]. The poor long-term survival reported in series of both combined and percutaneous stenting suggests that plastic stents may also offer a cost benefit in patients undergoing combined stenting. Comparison of cost between percutaneous and combined techniques must, however, also take into account the cost of the endoscopic procedure required for the latter technique. These cost-effectiveness issues would be best assessed within the context of a prospective randomised control trial.
Reduction of in-hospital mortality is a key goal in improving outcomes of patients undergoing stenting for malignant biliary obstruction. Factors associated with adverse outcome have been explored in patients with malignant biliary obstruction undergoing surgical, endoscopic and percutaneous decompression [8, 18–24]. However, save for the performance of preceding biliary drainage [17], they have not been examined in the context of combined stenting. The secondary aim of this study was, therefore, to identify factors that correlate with adverse outcome following combined biliary stenting.
Baseline ASA grade, representative of pre-existing co-morbidity, independently predicted death following combined stenting. This finding agrees with a previous study of jaundiced patients undergoing biliary surgery, which concluded that postoperative deaths and serious complications were principally the result of associated disease [21]. A number of potentially reversible physiological parameters were also associated with adverse outcome in this study. Decreasing haemoglobin and decreasing serum albumin were both significantly associated with morbidity and mortality on univariate analysis, with albumin independently associated with in-hospital mortality. Depression of these variables is central to the nutritional deficiency and cachexia that typifies terminal hepatopancreaticobiliary malignancy, and both have previously been shown to correlate with poor outcome following both surgical [18, 22] and percutaneous decompression of jaundice [24].
In agreement with other series of biliary stenting, biliary sepsis was responsible for the majority of morbidity and mortality in this study. As expected, therefore, the presence of sepsis pre-procedure was independently associated with the development of morbidity following combined stenting. For mortality, the presence of sepsis pre-procedure, whilst a significant predictor on univariate analysis, did not maintain independent prognostic significance. However, increasing leucocyte count, a marker of sepsis, was independently associated with both morbidity and mortality following combined biliary stenting.
The influence of the timing of the two stages of the combined procedure on outcome was previously examined by Wayman et al. [17]. In that study, 41 patients, primarily based on the availability of radiological expertise, were allocated to undergo either combined stenting on the same day as failed index ERCP or percutaneous drainage several days after failed ERCP, with definitive combined stenting several days later. The study reported significantly increased morbidity, particularly septic complications, in patients undergoing prior biliary drainage, though no analysis for confounding factors was performed. On the basis of these findings, those authors recommended that combined stenting should be performed only when the two stages of the procedure can be performed simultaneously. Of note, however, following the initial unsuccessful attempt at endoscopic stenting, patients undergoing two-stage procedures were left with undrained biliary systems for up to 7 days prior to percutaneous drain placement, a policy that would clearly have increased their potential for the development of septic complications over that of patients undergoing immediate combined drainage.
In agreement with Wayman et al. [17], the current study also found morbidity and mortality to be higher in patients undergoing biliary drainage prior to combined stenting, though these differences were not significant. In the current study, however, biliary drainage was carried out for specific indications, generally to achieve expedient drainage of an infected, obstructed biliary system, or to prevent the development of biliary sepsis in patients in whom contrast had been introduced above a stricture at index ERCP. The poorer results of patients undergoing biliary drainage prior to stenting are, therefore, almost certainly a consequence of physiological derangement preceding drain placement. Whilst we do not advocate routine percutaneous biliary drainage prior to combined stenting, it remains necessary in cases where urgent decompression of the biliary tree is required.
In conclusion, combined biliary stenting is associated with short- and long-term outcomes comparable to those reported for percutaneous stenting, but at a potentially lower cost per procedure. Randomised control studies are required to further compare the percutaneous and combined stenting techniques in patients who cannot be stented by endoscopy alone and should include cost-effectiveness analyses. This patient group typically have end-stage disease and significant numbers die in hospital following biliary stenting. Early recognition and treatment of sepsis and scrupulous management of co-morbid disease may, however, improve patient outcomes.
References
Moss AC, Morris E, Leyden J, MacMathuna P (2007) Malignant distal biliary obstruction: a systematic review and meta-analysis of endoscopic and surgical bypass results. Cancer Treat Rev 33:213–221
Moss AC, Morris E, Mac Mathuna P (2006) Palliative biliary stents for obstructing pancreatic carcinoma. Cochrane Database Syst Rev CD004200
Speer AG, Cotton PB, Russell RC, Mason RR, Hatfield AR, Leung JW et al (1987) Randomised trial of endoscopic versus percutaneous stent insertion in malignant obstructive jaundice. Lancet 2:57–62
Alfke H, Alfke B, Froelich JJ, Klose KJ, Wagner HJ (2003) Treatment of malignant biliary occlusion by means of transhepatic percutaneous biliary drainage with insertion of metal stents—results of an 8-year follow-up and analysis of the prognostic parameters. Rofo 175:1125–1129
Brountzos EN, Ptochis N, Panagiotou I, Malagari K, Tzavara C, Kelekis D (2007) A survival analysis of patients with malignant biliary strictures treated by percutaneous metallic stenting. Cardiovasc Intervent Radiol 30:66–73
Inal M, Akgul E, Aksungur E, Demiryurek H, Yagmur O (2003) Percutaneous self-expandable uncovered metallic stents in malignant biliary obstruction. Complications, follow-up and reintervention in 154 patients. Acta Radiol 44:139–146
Indar AA, Lobo DN, Gilliam AD, Gregson R, Davidson I, Whittaker S et al (2003) Percutaneous biliary metal wall stenting in malignant obstructive jaundice. Eur J Gastroenterol Hepatol 15:915–919
Lammer J, Hausegger KA, Fluckiger F, Winkelbauer FW, Wildling R, Klein GE et al (1996) Common bile duct obstruction due to malignancy: treatment with plastic versus metal stents. Radiology 201:167–172
Lee BH, Choe DH, Lee JH, Kim KH, Chin SY (1997) Metallic stents in malignant biliary obstruction: prospective long-term clinical results. AJR Am J Roentgenol 168:741–745
Rieber A, Brambs HJ (1997) Metallic stents in malignant biliary obstruction. Cardiovasc Intervent Radiol 20:43–49
Tesdal IK, Adamus R, Poeckler C, Koepke J, Jaschke W, Georgi M (1997) Therapy for biliary stenoses and occlusions with use of three different metallic stents: single-center experience. J Vasc Interv Radiol 8:869–879
Tsang TK, Crampton AR, Bernstein JR, Ramos SR, Wieland JM (1987) Percutaneous-endoscopic biliary stent placement. A preliminary report. Ann Intern Med 106:389–392
Banerjee B, Harshfield DL, Thomas GA, Waits WJ, Teplick SK (1994) A modified combined percutaneous and endoscopic procedure for biliary stent placement. J Interven Radiol 9:153–159
Dowsett JF, Vaira D, Hatfield AR, Cairns SR, Polydorou A, Frost R et al (1989) Endoscopic biliary therapy using the combined percutaneous and endoscopic technique. Gastroenterology 96:1180–1186
Hunt JB, Sayer JM, Jacyna M, Crofton M, Summerfield JA (1993) Combined percutaneous transhepatic and endoscopic placement of biliary stents. Surg Oncol 2:293–298
Verstandig AG, Goldin E, Sasson T, Weinberger G, Wengrower D, Fich A et al (1993) Combined transhepatic and endoscopic procedures in the biliary system. Postgrad Med J 69:384–388
Wayman J, Mansfield JC, Matthewson K, Richardson DL, Griffin SM (2003) Combined percutaneous and endoscopic procedures for bile duct obstruction: simultaneous and delayed techniques compared. Hepatogastroenterology 50:915–918
Blamey SL, Fearon KC, Gilmour WH, Osborne DH, Carter DC (1983) Prediction of risk in biliary surgery. Br J Surg 70:535–538
Bonnel D, Ferrucci JT Jr, Mueller PR, Lacaine F, Peterson HF (1984) Surgical and radiological decompression in malignant biliary obstruction: a retrospective study using multivariate risk factor analysis. Radiology 152:347–351
Han XC, Li JL, Han G (2003) Surgical mortality in patients with malignant obstructive jaundice: a multivariate discriminant analysis. Hepatobiliary Pancreat Dis Int 2:435–440
Pellegrini CA, Allegra P, Bongard FS, Way LW (1987) Risk of biliary surgery in patients with hyperbilirubinemia. Am J Surg 154:111–117
Su CH, P’Eng FK, Lui WY (1992) Factors affecting morbidity and mortality in biliary tract surgery. World J Surg 16:536–540
Prat F, Chapat O, Ducot B, Ponchon T, Fritsch J, Choury AD et al (1998) Predictive factors for survival of patients with inoperable malignant distal biliary strictures: a practical management guideline. Gut 42:76–80
Rai R, Dick R, Doctor N, Dafnios N, Morris R, Davidson BR (2000) Predicting early mortality following percutaneous stent insertion for malignant biliary obstruction: a multivariate risk factor analysis. Eur J Gastroenterol Hepatol 12:1095–1100
Martin DF (1994) Combined percutaneous and endoscopic procedures for bile duct obstruction. Gut 35:1011–1012
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA et al (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101:1644–1655
Schmassmann A, von Gunten E, Knuchel J, Scheurer U, Fehr HF, Halter F (1996) Wallstents versus plastic stents in malignant biliary obstruction: effects of stent patency of the first and second stent on patient compliance and survival. Am J Gastroenterol 91:654–659
Arguedas MR, Heudebert GH, Stinnett AA, Wilcox CM (2002) Biliary stents in malignant obstructive jaundice due to pancreatic carcinoma: a cost-effectiveness analysis. Am J Gastroenterol 97:898–904
Yeoh KG, Zimmerman MJ, Cunningham JT, Cotton PB (1999) Comparative costs of metal versus plastic biliary stent strategies for malignant obstructive jaundice by decision analysis. Gastrointest Endosc 49:466–471
Acknowledgements
The authors would like to thank Dr. John Bankart (Department of Health Sciences, University of Leicester) for advice regarding statistical techniques.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Neal, C.P., Thomasset, S.C., Bools, D. et al. Combined percutaneous–endoscopic stenting of malignant biliary obstruction: results from 106 consecutive procedures and identification of factors associated with adverse outcome. Surg Endosc 24, 423–431 (2010). https://doi.org/10.1007/s00464-009-0586-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-009-0586-0