Abstract
Background
There is debate about whether intraoperative cholangiography (IOC) should be performed routinely or selectively during laparoscopic cholecystectomy (LC) in patients with suspected choledocholithiasis. The timing of endoscopic retrograde cholangiopancreatography (ERCP) in these patients also is an issue. We reviewed the experience in our center, where a management algorithm limiting ERCP in relation to LC was adopted.
Methods
We retrospectively reviewed every LC performed by one surgeon during 6 years and the related ERCPs.
Results
A total of 264 LCs were performed. In 30 patients, stones were cleared or excluded by preoperative ERCP. In the remaining 234 LCs, 31 of 34 IOCs were successfully performed. Two of 31 IOCs were positive for bile duct stones; stone removal was successful in each patient at subsequent ERCP. Only 10 of 201 patients who did not have IOC required postsurgical ERCP within 10 weeks of LC, 3 of whom had common bile duct stones at ERCP.
Conclusions
For patients who underwent LC, we performed selective IOC with postoperative ERCP for positive studies. Review of our experience using this algorithm showed it to be a powerful tool in limiting unnecessary ERCPs. Our data suggest that routine preoperative ERCP cannot be justified. Selective IOC during LC misses relatively few cases of biliary stones; these can be managed quickly by experienced endoscopists.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
There is ongoing debate about whether intraoperative cholangiography (IOC) should be performed routinely [1–4] or selectively [5–7] during laparoscopic cholecystectomy (LC), and regarding the timing of preoperative or postoperative endoscopic retrograde cholangiopancreatography (ERCP) [8–14] in patients who are suspected of having choledocholithiasis. Laparoscopic common bile duct (CBD) exploration has emerged recently as a treatment option for ductal stones; however, ERCP before or after LC is still the most common approach [15–17]. Several studies in the laparoscopic age have investigated the use of preoperative criteria, such as liver function tests (LFTs), ultrasound findings, and features and severity of pancreatitis and cholangitis, to predict likelihood of common bile duct stones. The results vary somewhat between studies but overall have been fairly disappointing [8–13, 18]. The use of these and other criteria to “drive” the use of preoperative ERCP has resulted in a high percentage of negative studies. Whether IOC should be performed routinely or selectively also is controversial. Common bile duct stones (CBDS) in patients undergoing elective LC may occur in up to 11% of cases [3, 4, 19, 20]. Some have suggested that routine IOC should be the “gold standard” because its use reduces the probability of retained CBDS and reduces the risk of CBD damage during laparoscopic surgery. However, many laparoscopic surgeons feel that selective use of IOC is preferable. We reviewed a 6-year experience in our major referral center, where a management algorithm limiting ERCP in relation to LC was agreed on between the endoscopists and one senior biliary surgeon.
Patients and methods
We retrospectively reviewed a database of every LC performed between August 1993 and February 1999 by one experienced surgeon (TNP) at our tertiary referral center. Further patient details were obtained from hospital records. Permission to perform these record searches was granted by the Duke University Medical Center Institutional Review Board (IRB). Details of patient demographics were recorded. Indications for LC were detailed, as were the use and findings of IOC. The outcome of all patients who had IOC performed was studied. The incidence of postoperative ERCP within 10 weeks of surgery in patients who did not have IOC was determined. ERCPs relating to these procedures were reviewed in two computerized endoscopy databases. All ERCPs were performed by senior endoscopists skilled in ERCP (JB, MSB, PSJ).
Surgical technique for LC and IOC
A standardized, four-cannula technique was used for laparoscopic cholecystectomy. Intraoperative cholangiography (IOC) was performed if there was a concern about possible CBDS based on preoperative indicators (see below) or there was a need to define the biliary anatomy. IOC was performed in a standard manner: the cystic duct was identified and a clip placed close to the gallbladder neck; a pair of straight scissors was used to open the duct, and a flexible cholangiography catheter was introduced to perform cholangiography.
Results
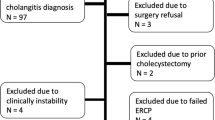
LC was performed in 264 patients (87 male, 177 female) during the study period (Fig. 1). In 30 patients, CBDS were cleared or excluded by preoperative ERCP. The main indications for preoperative ERCP were gallstone pancreatitis (n = 7), cholangitis (n = 4), jaundice/abnormal LFTs (n = 12), dilated CBD on ultrasound (n = 6), and chronic abdominal pain (n = 1). For the purposes of this study, the 30 patients who had preoperative ERCP were excluded from further analysis.
Indications for laparoscopic cholecystectomy
In the remaining 234 patients, indications for LC included cholelithiasis (n = 154), acute (n = 31) and chronic (n = 19) cholecystitis, gallstone pancreatitis (n = 10), biliary colic (n = 5), and “other” (e.g., suspected gallbladder dyskinesia; n = 15) (Table 1).
Intraoperative cholangiography
During the 234 LCs, 31 of 34 (91%) IOC attempts were successful. A policy of selective IOC was used by the surgeon in this study; the decision to perform this imaging was based on a variety of preoperative indicators, including a history of gallstone pancreatitis, mild dilatation of the biliary tree on transabdominal ultrasound, and abnormal LFTs (Table 2). Only 2 of 31 (6.5%) IOCs were positive for bile duct stones. These two patients had ERCP with successful stone removal within 24 hours of LC. Five IOCs showed mildly dilated CBDs with no evidence of CBDS, possibly reflecting recent stone passage. The other 24 IOCs were within normal limits.
Postoperative ERCP in patients who did not undergo IOC or had failed IOC
Two of three patients with failed IOCs had early postoperative ERCP: one for abdominal pain and ultrasound findings suggesting a stone, and the other for persistently abnormal LFTs. The first patient had a CBD stone, which was removed, and the second had a normal biliary tree. Another eight patients who did not have IOC during LC underwent ERCP within 10 weeks of LC: for acute pancreatitis, abdominal pain, abnormal LFTs, and unexplained fever. ERCP was normal in six of eight patients; two of eight had CBDS successfully removed. Thus, only 10 of 201 patients (5%) who did not have IOC (i.e., not performed or failed) had postsurgical ERCP within 10 weeks of LC (Table 3). If we include the 2 patients with positive IOCs, only 12 of 234 patients (5.1%) required postoperative ERCP. There were no diagnostic or therapeutic ERCP failures.
Discussion
Whether intraoperative cholangiography (IOC) should be performed routinely or selectively at the time of laparoscopic cholecystectomy (LC) is still a subject of much debate. Advocates of routine IOC argue that preoperative prediction of choledocholithiasis is inaccurate and that IOC is the only way to guarantee a stone-free bile duct, thereby minimizing subsequent problems related to CBDS [1–4]. CBDS are reported in 2–11% of cases in LC series during which IOC is performed routinely [3, 4, 19, 20]. IOC has been made easier, faster, and more accurate by the advent of intraoperative fluoroscopy. Those who support routine IOC stress the importance of delineation of biliary anatomy to avoid or lessen bile duct injury during laparoscopic surgery [2, 21–23]. A recent, prospective study reported an abnormal IOC in 287 (27.2%) of 1,056 IOCs that had been performed routinely during LC [24]. Although routine IOC may not decrease the overall incidence of operative injuries to the bile duct, there is evidence that its routine use may minimize the extent of the injury so that it can be repaired easily without significant consequences for the patient [2, 25, 26]. In addition, there is evidence to suggest that routine IOC during LC is a cost-effective means of preventing the costs of delayed recognition of bile duct injuries [27]. However, other studies have shown that IOC could be selectively performed and had few postoperative CBD stone complications [5, 7, 28–30]. One group proposed that it is unreasonable to perform routine IOC during laparoscopic cholecystectomy because it is negative in >90% of cases [31]. In addition, IOC often involves more dissection, more time, more cost, and more radiation exposure to the patient and operating staff. Many surgeons in favor of selective use of IOC during LC argue that IOC is not necessary in patients with normal LFTs and CBD diameter, and no history of gallstone pancreatitis or jaundice. In a prospective study of 155 patients to evaluate whether IOC could be safely omitted during LC in patients who meet these criteria, there were only four postoperative complications and one CBD injury, and no patients were found to have retained CBDS during follow-up [28]. In another study of more than 2,000 patients, results of routine IOC were compared with selective IOC in patients who underwent LC. The authors concluded from their findings that the increased morbidity and cost of routine IOC to avoid symptomatic residual CBDS is not justified, and that selective IOC is an effective method of verifying suspected CBDS [32].
The debate about the use of selective or routine IOC during LC is intimately linked to the practice of preoperative and postoperative ERCP. Most authorities agree that routine preoperative ERCP cannot be justified. This practice exposes patients to unnecessary morbidity and added cost. Although preoperative studies, such as LFTs and ultrasound findings, and clinical data, such as recent pancreatitis, cholangitis, or obstructive jaundice, are not particularly reliable, several studies have supported the practice of selective preoperative ERCP based on the above factors followed by laparoscopic cholecystectomy [8–13, 33]. It has been suggested by some, in an attempt to limit the number of negative ERCPs before laparoscopy, that preoperative ERCP should be reserved for patients who have documented choledocholithiasis, acute cholangitis, or severe biliary pancreatitis [3, 14, 18, 33]. When IOC demonstrates choledocholithiasis, the choices include: (1) proceed to postoperative ERCP, (2) single-stage laparoscopic procedure with cholecystectomy and laparoscopic bile duct exploration [15, 16], or, occasionally, (3) open bile duct exploration. However, few surgeons have the necessary training or an interest in performing laparoscopic bile duct stone extraction. Because this latter procedure is likely to be a practice adopted in only a limited number of centers of excellence, many recommend routine IOC during laparoscopic cholecystectomy and postoperative ERCP as necessary. In experienced hands, postoperative ERCP to clear CBDS has a high success rate: 97–100% in several series [34–36]. An option that has received much less attention is that of combined intraoperative LC and ERCP, a combined procedure that includes a one-stage treatment of cholelithiasis and choledocholithiasis [37]. This policy has been shown to be effective but is not a common practice.
However, there is little information on the outcome of a practice of selective use of both IOC and preoperative ERCP. One study from Germany supported the practice of selective preoperative, intraoperative, and postoperative bile duct diagnosis for patients; results showed low morbidity and high efficiency in avoiding CBDS with such a practice [38]. Many who support selective preoperative ERCP suggest routine IOC during laparoscopic cholecystectomy in those patients who did not have preoperative ERCP. Our large study supports the practice of selective preoperative ERCP, selective IOC during laparoscopic cholecystectomy and early postoperative ERCP for positive studies. Retrospective review of 6 years experience of one surgeon adhering to this algorithm shows that it is a powerful tool to limit unnecessary (low-yield) ERCPs. Our reported low incidence (6.5%) of CBD stones at IOC may suggest that, although the incidence of CBD stones at IOC is approximately 10% as shown in some studies, the incidence of symptomatic CBD stones is lower. We conclude that routine preoperative ERCP cannot be justified and that selective IOC during laparoscopic cholecystectomy misses relatively few cases of retained CBDS, which can be dealt with quickly by experienced endoscopists.
References
Sackier JM, Berci G, Phillips E, Carroll B, Shapiro S, Paz-Partlow M (1991) The role of cholangiography in laparoscopic cholecystectomy. Arch Surg 126:1021–1025
Stuart SA, Simpson TI, Alvord LA, Williams MD (1998) Routine intraoperative laparoscopic cholangiography. Am J Surg 176:632–637
Duensing RA, Williams RA, Collins JC, Wilson SE (1995) Managing choledocholithiasis in the laparoscopic era. Am J Surg 170:619–623
Ammori BJ, Birbas K, Davides D, Vezakis A, Larvin M, McMahon MJ (2000) Routine vs “on demand” postoperative ERCP for small bile duct calculi detected at intraoperative cholangiography. Clinical evaluation and cost analysis. Surg Endosc 14:1123–1126
Clair DG, Carr-Locke DL, Becker JM, Brooks DC (1993) Routine cholangiography is not warranted during laparoscopic cholecystectomy. Arch Surg 128:551–555
Voyles CR, Sanders DL, Hogan R (1994) Common bile duct evaluation in the era of laparoscopic cholecystectomy. 1050 cases later. Ann Surg 219:744–752
Pietra N, Sarli L, Maccarini PU, Sabadini G, Costi R, Gobbi S (2000) Five-year prospective audit of routine intravenous cholangiography and selective endoscopic retrograde cholangiography with or without intraoperative cholangiography in patients undergoing laparoscopic cholecystectomy. World J Surg 24:345–352
Koo KP, Traverso LW (1996) Do preoperative indicators predict the presence of common bile duct stones during laparoscopic cholecystectomy? Am J Surg 171:495–499
Hauer-Jensen M, Karesen R, Nygaard K, Solheim K, Amlie E, Havig O et al (1985) Predictive ability of choledocholithiasis indicators. A prospective evaluation. Ann Surg 202:64–68
Lacaine F, Corlette MB, Bismuth H (1980) Preoperative evaluation of the risk of common bile duct stones. Arch Surg 115:1114–1116
Prat F, Meduri B, Ducot B, Chiche R, Salimbeni-Bartolini R, Pelletier G (1999) Prediction of common bile duct stones by noninvasive tests. Ann Surg 229:362–368
Abboud PA, Malet PF, Berlin JA, Staroscik R, Cabana MD, Clarke JR et al (1996) Predictors of common bile duct stones prior to cholecystectomy: a meta-analysis. Gastrointest Endosc 44:450–455
Trondsen E, Edwin B, Reiertsen O, Faerden AE, Fagertun H, Rosseland AR (1998) Prediction of common bile duct stones prior to cholecystectomy: a prospective validation of a discriminant analysis function. Arch Surg 133:162–166
Ng T, Amaral JF (1999) Timing of endoscopic retrograde cholangiopancreatography and laparoscopic cholecystectomy in the treatment of choledocholithiasis. J Laparoendosc Adv Surg Tech A 9:31–37
Phillips EH (1998) Laparoscopic transcystic duct common bile duct exploration. Surg Endosc 12:365–366
Paganini AM, Lezoche E (1998) Follow-up of 161 unselected consecutive patients treated laparoscopically for common bile duct stones. Surg Endosc 12:23–29
Urbach DR, Khajanchee YS, Jobe BA, Standage BA, Hansen PD, Swanstrom LL (2001) Cost-effective management of common bile duct stones: a decision analysis of the use of endoscopic retrograde cholangiopancreatography (ERCP), intraoperative cholangiography, and laparoscopic bile duct exploration. Surg Endosc 15:4–13
Cotton PB (1993) Endoscopic retrograde cholangiopancreatography and laparoscopic cholecystectomy. Am J Surg 165:474–478
Lezoche E, Paganini A, Guerrieri M, Carlei F, Lomanto D, Sottili M et al (1994) Technique and results of routine dynamic cholangiography during 528 consecutive laparoscopic cholecystectomies. Surg Endosc 8:1443–1447
Hainsworth PJ, Rhodes M, Gompertz RH, Armstrong CP, Lennard TW (1994) Imaging of the common bile duct in patients undergoing laparoscopic cholecystectomy. Gut 35:991–995
Gigot J, Etienne J, Aerts R, Wibin E, Dallemagne B, Deweer F et al (1997) The dramatic reality of biliary tract injury during laparoscopic cholecystectomy. An anonymous multicenter Belgian survey of 65 patients. Surg Endosc 11:1171–1178
Ludwig K, Bernhardt J, Lorenz D (2002) Value and consequences of routine intraoperative cholangiography during cholecystectomy. Surg Laparosc Endosc Percutan Tech 12:154–159
Ciulla A, Agnello G, Tomasello G, Castronovo G, Maiorana AM, Genova G (2007) The intraoperative cholangiography during videolaparoscopic cholecystectomy. What is its role? Results of a non-randomized study. Annali Italiani di Chirurgia 78:85–89
Hamouda AH, Goh W, Mahmud S, Khan M, Nassar AH (2007) Intraoperative cholangiography facilitates simple transcystic clearance of ductal stones in units without expertise for laparoscopic bile duct surgery. Surg Endosc 21:955–959
Carroll BJ, Friedman RL, Liberman MA, Phillips EH (1996) Routine cholangiography reduces sequelae of common bile duct injuries. Surg Endosc 10:1194–1197
Vezakis A, Davides D, Ammori BJ, Martin IG, Larvin M, McMahon MJ (2000) Intraoperative cholangiography during laparoscopic cholecystectomy. Surg Endosc 14:1118–1122
Podnos YD, Gelfand DV, Dulkanchainun TS, Wilson SE, Cao S, Ji P et al (2001) Is intraoperative cholangiography during laparoscopic cholecystectomy cost effective? Am J Surg 182:663–669
Borjeson J, Liu SK, Jones S, Matolo NM (2000) Selective intraoperative cholangiography during laparoscopic cholecystectomy: how selective? Am Surg 66:616–618
Singh G, Gupta PC, Sridar G, Katariya RN (2000) Role of selective intraoperative cholangiography during cholecystectomy. Aust N Z J Surg 70:106–109
Coppola R, Riccioni ME, Ciletti S, Cosentino L, Ripetti V, Magistrelli P (2001) Selective use of endoscopic retrograde cholangiopancreatography to facilitate laparoscopic cholecystectomy without cholangiography. A review of 1139 consecutive cases. Surg Endosc 15:1213–1216
Sarli L, Roncoroni L, Costi R (2002) Risks of “on demand” postoperative endoscopic retrograde cholangiopancreatography (ERCP) for small bile duct calculi detected at intraoperative cholangiography (IOC). Surg Endosc 16:1016–1018
Snow LL, Weinstein LS, Hannon JK, Lane DR (2001) Evaluation of operative cholangiography in 2043 patients undergoing laparoscopic cholecystectomy: a case for the selective operative cholangiogram. Surg Endosc 15:14–20
Rijna H, Kemps WG, Eijsbouts Q, Meuwissen SG, Cuesta MA (2000) Preoperative ERCP approach to common bile duct stones: results of a selective policy. Dig Surg 17:229–233
Frazee RC, Roberts J, Symmonds R, Hendricks JC, Snyder S, Smith R et al (1993) Combined laparoscopic and endoscopic management of cholelithiasis and choledocholithiasis. Am J Surg 166:702–706
Graham SM, Flowers JL, Scott TR, Bailey RW, Scovill WA, Zucker KA et al (1993) Laparoscopic cholecystectomy and common bile duct stones. The utility of planned perioperative endoscopic retrograde cholangiography and sphincterotomy: experience with 63 patients. Ann Surg 218:61–67
Franceschi D, Brandt C, Margolin D, Szopa B, Ponsky J, Priebe P et al (1993) The management of common bile duct stones in patients undergoing laparoscopic cholecystectomy. Am Surg 59:525–532
Kalimi R, Cosgrove JM, Marini C, Stark B, Gecelter GR (2000) Combined intraoperative laparoscopic cholecystectomy and endoscopic retrograde cholangiopancreatography: lessons from 29 cases. Surg Endosc 14:232–234
Leibl BJ, Ulrich M, Scheuritzel U, Wellhausser U, Schmidt W, Marquardt B et al (2001) Selective pre- intra- and postoperative bile duct diagnosis: an efficient and low complication regimen within the scope of laparoscopic cholecystectomy. Early and late results of a prospective study. Chirurg 72:812–817
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Byrne, M.F., McLoughlin, M.T., Mitchell, R.M. et al. For patients with predicted low risk for choledocholithiasis undergoing laparoscopic cholecystectomy, selective intraoperative cholangiography and postoperative endoscopic retrograde cholangiopancreatography is an effective strategy to limit unnecessary procedures. Surg Endosc 23, 1933–1937 (2009). https://doi.org/10.1007/s00464-008-0250-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-008-0250-0