Abstract
Introduction
Choledocholithiasis is most often managed in a two-procedure pathway including endoscopic retrograde cholangiopancreatography (ERCP) followed by laparoscopic cholecystectomy (LC). In contrast, a single-stage, surgery-first approach consisting of LC, cholangiogram, and laparoscopic common bile duct exploration (LCBDE) is associated with reduced hospital stays and equivalent morbidity. Despite this, nationwide referral patterns heavily favor ERCP, obscuring those undergoing ERCP with obstructions amenable to simple intraoperative interventions. We hypothesized that most patients had endoscopic findings consistent with simple sludge or small-to-medium stones, which could have been cleared by basic LCBDE maneuvers.
Methods
We retrospectively reviewed 294 patients > 18 years old who underwent preoperative ERCP for the management of suspected choledocholithiasis. Exclusion criteria included: failed ERCP, cholangitis, prior cholecystectomy, patient refusal of surgery, or medical conditions precluding surgical candidacy. Stone size was categorized as small (0–4 mm), medium (5–7 mm), and large (≥ 8 mm).
Results
At the time of ERCP, 37 (20.1%) patients had sludge only, 96 (52.2%) had stones only, 42 (22.8%) had sludge and stones, and 9 (4.8%) had no stones. Of the 138 patients with any stones, 37 (26.8%) had small stones, 41 (29.7%) medium, 43 (31.2%) large, and 17 (12.3%) had uncharacterizable stones. Overall, 74.3% of patients had findings of sludge, stones (0–7 mm), or negative ERCP.
Conclusion
The majority of patients who underwent preoperative ERCP for suspected choledocholithiasis had findings that are amenable to simple intraoperative interventions. In fact, over a quarter of the patients had a negative ERCP, sludge, or small stones which would likely be cleared by flushing/glucagon precluding any further instrumentation. While large stones may require more advanced techniques, this represents a small percentage of patients. Surgery-first management for suspected choledocholithiasis can offer an efficient alternative for the majority of patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Gallstone disease is one of the most prevalent surgically treatable disorders in adults, and up to 19% of patients undergoing cholecystectomy in the acute setting have choledocholithiasis [1]. The treatment pathway for choledocholithiasis often includes an initial endoscopic retrograde cholangiopancreatography (ERCP) followed by a laparoscopic cholecystectomy (LC) [2]. An alternative is a single intervention consisting of LC with intraoperative cholangiogram (IOC) and a laparoscopic common bile duct exploration (LCBDE) [2,3,4,5]. Despite several randomized control trials demonstrating the safety and success of LCBDE since its introduction in the 1990s, it has not been widely adopted as the standard of care and many centers still favor the two-stage pathway [3]. This treatment preference not only obscures the number of patients who may benefit from a surgery-first approach, but also results in longer hospital stays, higher costs, and increased patient exposure to unnecessary interventions [6, 7].
While ERCP has well-established diagnostic and therapeutic benefits, it is associated with potential complications, including pancreatitis, post-sphincterotomy bleeding, infection, and perforation [8]. Moreover, depending on the indication guideline criteria, over 20% of ERCPs may result in CBD stone-negative cases [9, 10]. These non-therapeutic interventions likely arise from spontaneous stone migration prior to intervention or an incorrect preoperative diagnosis. This uncertainty raises concerns surrounding frequent utilization of ERCP including the risks associated with multiple anesthetic events. To minimize these risks, there is an increased reliance on advanced imaging techniques like MRCP prior to ERCP to ensure the correct diagnosis [11]. Furthermore, ERCP is not always effective. Studies have reported a post-ERCP choledocholethiasis incidence of up to 16.9% found on IOC during the subsequent LC [12]. For these reasons, proponents of LCBDE have suggested that IOC is equally effective as ERCP in identifying stones, further supporting a surgery-first approach [13, 14]. Yet, despite the additional interventions, imaging, and laboratory studies that prolong length of stay and increase resource utilization, ERCP remains the dominant paradigm for the management of choledocholithiasis in the absence of cholangitis.
In contrast, LCBDE maneuvers are effective in clearing the majority of obstructions in choledocholithiasis, with success rates ranging from 80 to 99% [3, 4, 15, 16]. Therefore, our intention was to identify the scope of missed opportunities for a surgery-first intervention in a tertiary care center. We sought to determine whether patients undergoing the ERCP-first pathway had endoscopic findings amenable to a surgery-first, single-stage approach. We hypothesized that the majority of patients undergoing preoperative ERCP for choledocholithiasis in the absence of cholangitis had findings that could have been cleared by basic LCBDE maneuvers, specifically, those with sludge, CBD stone-negative ERCPs, and small-to-medium stones. While large stones may require more advanced LCBDE techniques and equipment such as lithotripsy, we predicted this would be a small percentage of patients presenting with choledocholithiasis.
Methods
This study was approved by the Institutional Review Board (IRB). A retrospective chart review was performed and included all adult patients (age ≥ 18 years) who underwent preoperative ERCP from 2018 to 2022. Inclusion criteria included: age greater than 18 years old, a diagnosis of choledocholithiasis, and performance of a preoperative ERCP for suspected choledocholithiasis in patients who later underwent cholecystectomy. The diagnosis was made by a combination of imaging findings consistent with biliary obstruction (dilated ducts or evidence of stone), biochemical results, and clinical presentation. Exclusion criteria were ultimately a failed ERCP or instances in which ERCP would be a first-line therapy, such as: a diagnosis of cholangitis, prior cholecystectomy, patient declining of surgery, or medical conditions precluding surgical candidacy [17].
We retrospectively reviewed patients’ medical records for baseline characteristics, hospital course, clinical data, and ERCP findings. Study data were collected and managed using REDCap electronic data capture tools hosted at our institution [18]. Stone size was categorized as small (0–4 mm), medium (5–7 mm), and large (≥ 8 mm) based on institutional criteria as well as available definitions in the biliary literature [19,20,21,22]. Whenever multiple stones were encountered, the size of the largest stone was used for classification. All ERCP were performed by experienced endoscopists who routinely quantify stone sizes.
Results
A total of 535 patients who were diagnosed with obstructive biliary disease and underwent LC with either preoperative or postoperative ERPC from 2018 to 2022 were screened. After excluding those who were under the age of 18 and those with postoperative ERCPs, 294 patients of interest were identified. Of these patients, those with a diagnosis of cholangitis (n = 97), refused surgery (n = 3), unfit surgical candidates (n = 4), prior cholecystectomy (n = 2), and patients with a failed ERCP (n = 4) were excluded. A total of 184 patients who received preoperative ERCP prior to laparoscopic cholecystectomy were included. Baseline characteristics included 104 females and 80 males with a median (IQR) age of 61.2 years (42.5–73.3), body mass index (BMI) of 29.5 kg/m2 (25.6–35.7). The median (IQR) length of stay was 88.6 h (68.7–118.8), and time from admission to ERCP intervention was 21.5 h (13.1–39.7). See Fig. 1 for a breakdown of included and excluded patients.
Ninety-four (51.1%) patients had a diagnosis involving choledocholithiasis without acute cholecystitis, making it the most common diagnosis. This was followed by choledocholithiasis with cholecystitis in 56 (30.4%) patients, and gallstone pancreatitis in 34 patients (18.5%). The majority of patients (57.1%) underwent multiple imaging modalities to characterize their pathology. This included ultrasound (US) in 128 (69.6%) patients, computed tomography (CT) scan in 117 (63.5%) patients, and magnetic resonance cholangiopancreatography (MRCP) in 63 (34.2%) patients. Stone identification rates for US, CT, and MRCP were 79.7%, 75.2%, 88.9%, respectively. Of the patients where pre-ERCP imaging identified or suggested stones, the ERCP-stone confirmation rate for US, CT, and MRCP were 67.7%, 76.1%, and 78.6%, respectively.
Of those included, 37 (20.1%) patients had sludge only, 42 (22.8%) patients had sludge and stones, 96 (52.2%) had stones only, and 9 (4.9%) patients had CBD stone-negative ERCPs, defined as nothing returned or removed during balloon sweeps (see Table 1). Of the 138 patients with stone involvement (either stones only or sludge and stones), 37 (26.8%) had small stones, 41 (29.7%) had medium-sized stones, 43 (31.2%) patients had large stones, and 17 (12.3%) had uncharacterized stones (see Table 2, Fig. 2). Sphincterotomy was performed in 175 (95%) patients, with 14 (8%) patients experiencing post-sphincterotomy bleeding. The median (IQR) CBD diameter was 10 mm (7–12). Stent placement was performed in 85 (45.9%) patients, in which 74 (40.2%) patients had biliary stents and 11 (5.9%) of patients had pancreatic stents placed. Of those who underwent preoperative ERCP (n = 184), 17 patients did not have complete reports specifying endoscopic findings. Among those with characterizable findings (n = 167), 124 (74.3%) patients had findings of sludge, sludge and stones, small or medium stones, or negative returns.
Discussion
Our study indicates that the majority of patients, 74.3%, who undergo preoperative ERCP for suspected choledocholithiasis without cholangitis have findings that are potentially amenable to clearance with simple intraoperative interventions. We defined findings amenable to simple LCBDE maneuvers as endoscopic findings of sludge, small or medium stones, or stone-negative ERCPs. While large stones may require more advanced LCBDE techniques and equipment such as transcystic or transductal choledocoscopy and lithotripsy, this represents a small percentage of patients presenting with choledocholithiasis.
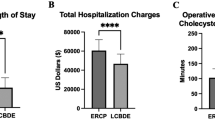
The optimal management of choledocholithiasis remains controversial. Despite the advancement of laparoscopy and decades of LCBDE experience, the traditional two-stage pathway involving preoperative ERCP followed by LC remains the preferred treatment modality at many institutions. While several studies have compared both approaches and demonstrated equivalent stone clearance rates and similar mortality and morbidity, LCBDE as a single-stage procedure offers the advantage of an individual anesthetic event resulting in shorter hospital stays and lower costs [3, 15, 23,24,25]. In fact, some studies suggest LCBDE can reduce the length of stay by 2 days, with a mean hospital stay between 40 and 50 h compared to over 80 h for ERCPs [24, 25]. Consistent with previous ERCP + LC literature, the median length of stay of our current study was 88.6 h. The longer hospital stay associated with the two-stage pathway can likely be attributed to the acquisition of additional imaging, time interval between anesthetic events, and trending biochemical markers; while the single-stage approach simultaneously confirms and treats choledocholithiasis in one intervention.
The implementation and efficacy of LCBDE are predicated on the surgeon’s comfort with LCBDE techniques and training, equipment availability, costs, as well as staff and institutional support. Moreover, the chosen approach, either transcystic or transductal, can also play a role. For instance, a study of 500 patients achieved a 99% stone clearance rate using both transcystic and transductal LCBDE, with a median stone size of 6–7 mm [4]. The authors reported that 14% of cases had findings of sludge at the time of LCBDE, which is consistent with our findings of 20% at the time of ERCP. However, while several studies report high success rates utilizing transcystic approaches, few define the success of a transcystic approach in relation to stone sizes, leaving room for uncertainty. For example, Martin et al., advocate that a transcystic approach should be attempted in all LCBDEs, yet report a success rate of only 67.3% [26]. Meanwhile, a systematic review and meta-analysis evaluating transcystic and transductal LCBDE report a 91% clearance versus 94%, respectively [27]. Tokumura et al. did comment on stone sizes, suggesting that stones less than 9 mm can be removed via a transcystic approach with a success rate of 87.5% [28]. Similarly, a prospective series of 505 patients reports a 72.5% ductal clearance success rate via transcystic approach for stones that were smaller than 7 mm, which is consistent with our hypothesis that most non-large stones can be cleared via simple LCBDE maneuvers [29]. Therefore, defining stone size is important to determine the effectiveness of LCBDE and characterize patients who will likely have successful clearance via the single-stage pathway.
The characterization of common bile duct stone sizes varies across studies, with various groups defining small, medium and large stones differently. Attasaranya et al., describe large stones as up to 25 mm in size [20], while others have defined large stones with ranges between ≥ 5 mm to ≥ 15 mm [22, 30]. Given the wide range of large stone size diameters reported in the literature, we defined large stones as ≥ 8 mm, as these stones may require advanced endoscopic or laparoscopic techniques for clearance [17, 24, 30, 31]. The majority of patients in our study had stones smaller than 8 mm, findings that have been reported to be amenable to clearance with simple transcystic LCBDE techniques [28, 32].
Small stones < 4 mm have a higher likelihood of spontaneous passage, and as such, may be amenable to simple power flushing and glucagon administration during LC and IOC [33, 34]. In fact, if we were to consider this in this patient cohort, of the 167 patients with characterizable complete endoscopic findings, 50% off all our study patients had findings that would likely resolve solely with power flushing or glucagon administration. This represents 67% of the patients identified as being amenable to LCBDE maneuvers. Moreover, some authors have suggested that patients who are found to have stones smaller than 5 mm after surgery do not require subsequent ERCP interventions as these are likely to pass on their own. This furthers the assertion that a surgery-first approach for these patients can eliminate unnecessary additional interventions as simple flushing may be the solution [19]. These concepts support a single-intervention approach as being a reasonable first-line treatment.
Despite being a relatively safe procedure, ERCP is associated with a risk of pancreatitis, bleeding, and perforation [35]. ERCP with sphincterotomy may also disrupt the sphincter of Oddi’s integrity, leading to duodenal-biliary reflux, a major cause of stone recurrence and chronic cholangitis [35, 36]. Although over 20% of ERCP interventions have no return of stones (i.e., negative ERCP), false positive rates of IOC during LCBDE are lower at 7% [14, 37]. This high rate of negative results from ERCP further supports the notion of a surgery-first approach. Since surgical intervention in the form of LC is necessary in both approaches, a surgery-first approach can help avoid unnecessary procedures and multiple anesthetic events while providing a treatment alternative that is associated with shorter inpatient stays [2, 3, 6].
The limitations of this study include its retrospective nature and a relatively limited number of patients included. Moreover, it is possible that this study’s main finding that 74.3% of ERCP cases will be amenable to LCBDE maneuvers is an overestimation. Other factors may contribute to the difficulty of performing LCBDE successfully, and looking at stone size alone may be an oversimplification. For example, cystic duct tortuosity and diameter, CBD size, location of obstruction, multiplicity of stones, and severity of gallbladder inflammation may affect LCBDE outcomes. While stone size is just one consideration, it is helpful to have the general awareness that clinical concern for choledocholithiasis often translates to small stones or sludge. A surgery-first approach allows for minimization of negative ERCPs and can facilitate clearance of the duct in agreeable operative settings. Follow-up studies will include a multi-center analysis of patients undergoing a two-stage approach and their endoscopic findings to further characterize those who would benefit from a single-stage approach. An additional desired future direction of our work is to implement a clear clinical pathway directed by stone size for providers at our institution in order to ensure the maximal number of patients are able to benefit from a surgery-first approach. Ultimately, adopting a surgery-first approach has the potential to improve patient care and reduce healthcare resource utilization.
Conclusion
Our findings suggest that the majority of patients who underwent preoperative ERCP for suspected choledocholithiasis had endoscopic findings that are amenable to simple operative interventions, including transcystic LCBDE techniques. Implementing surgery-first management for suspected choledocholithiasis can offer a safe and efficient alternative to the more traditional two-stage pathway and minimize patient exposure to unnecessary interventions.
References
Blohm M, Sandblom G, Enochsson L, Hedberg M, Andersson MF, Österberg J (2023) Relationship between surgical volume and outcomes in elective and acute cholecystectomy: nationwide, observational study. Br J Surg 110:353–361. https://doi.org/10.1093/bjs/znac415
Rogers SJ, Cello JP, Horn JK, Siperstein AE, Schecter WP, Campbell AR, Mackersie RC, Rodas A, Kreuwel HTC, Harris HW (2010) Prospective randomized trial of LC+LCBDE vs ERCP/S+LC for common bile duct stone disease. Arch Surg 145:28–33. https://doi.org/10.1001/archsurg.2009.226
Wandling MW, Hungness ES, Pavey ES, Stulberg JJ, Schwab B, Yang AD, Shapiro MB, Bilimoria KY, Ko CY, Nathens AB (2016) Nationwide assessment of trends in choledocholithiasis management in the United States from 1998 to 2013. JAMA Surg 151:1125–1130. https://doi.org/10.1001/jamasurg.2016.2059
Hua J, Meng H, Yao L, Gong J, Xu B, Yang T, Sun W, Wang Y, Mao Y, Zhang T, Zhou B, Song Z (2017) Five hundred consecutive laparoscopic common bile duct explorations: 5-year experience at a single institution. Surg Endosc 31:3581–3589. https://doi.org/10.1007/s00464-016-5388-6
Bosley ME, Zamora IJ, Neff LP (2021) Choledocholithiasis—a new clinical pathway. Transl Gastroenterol Hepatol 6:35–35. https://doi.org/10.21037/tgh-20-172
Bansal VK, Misra MC, Rajan K, Kilambi R, Kumar S, Krishna A, Kumar A, Pandav CS, Subramaniam R, Arora MK, Garg PK (2014) Single-stage laparoscopic common bile duct exploration and cholecystectomy versus two-stage endoscopic stone extraction followed by laparoscopic cholecystectomy for patients with concomitant gallbladder stones and common bile duct stones: a randomized controlled trial. Surg Endosc 28:875–885. https://doi.org/10.1007/s00464-013-3237-4
Bosley ME, Nunn AM, Westcott CJ, Neff LP (2022) Antegrade balloon sphincteroplasty as an adjunct to laparoscopic common bile duct exploration for the acute care surgeon. J Trauma Acute Care Surg 92:e47–e51. https://doi.org/10.1097/TA.0000000000003478
Chandrasekhara V, Khashab MA, Muthusamy VR, Acosta RD, Agrawal D, Bruining DH, Eloubeidi MA, Fanelli RD, Faulx AL, Gurudu SR, Kothari S, Lightdale JR, Qumseya BJ, Shaukat A, Wang A, Wani SB, Yang J, DeWitt JM (2017) Adverse events associated with ERCP. Gastrointest Endosc 85:32–47. https://doi.org/10.1016/j.gie.2016.06.051
Sperna Weiland CJ, Verschoor EC, Poen AC, Smeets XJMN, Venneman NG, Bhalla A, Witteman BJM, Timmerhuis HC, Umans DS, van Hooft JE, Bruno MJ, Fockens P, Verdonk RC, Drenth JPH, van Geenen EJM, for the Dutch Pancreatitis Study Group (2023) Suspected common bile duct stones: reduction of unnecessary ERCP by pre-procedural imaging and timing of ERCP. Surg Endosc 37:1194–1202. https://doi.org/10.1007/s00464-022-09615-x
Jacob JS, Lee ME, Chew EY, Thrift AP, Sealock RJ (2021) Evaluating the revised American Society for Gastrointestinal Endoscopy guidelines for common bile duct stone diagnosis. Clin Endosc 54:269–274. https://doi.org/10.5946/ce.2020.100
Makmun D, Fauzi A, Shatri H (2017) Sensitivity and specificity of magnetic resonance cholangiopancreatography versus endoscopic ultrasonography against endoscopic retrograde cholangiopancreatography in diagnosing choledocholithiasis: the Indonesian experience. Clin Endosc 50:486–490. https://doi.org/10.5946/ce.2016.159
Pierce RA, Jonnalagadda S, Spitler JA, Tessier DJ, Liaw JM, Lall SC, Melman LM, Frisella MM, Todt LM, Brunt LM, Halpin VJ, Eagon JC, Edmundowicz SA, Matthews BD (2008) Incidence of residual choledocholithiasis detected by intraoperative cholangiography at the time of laparoscopic cholecystectomy in patients having undergone preoperative ERCP. Surg Endosc 22:2365–2372. https://doi.org/10.1007/s00464-008-9785-3
de Sousa S, Tobler O, Iranmanesh P, Frossard J-L, Morel P, Toso C (2017) Management of suspected common bile duct stones on cholangiogram during same-stay cholecystectomy for acute gallstone-related disease. BMC Surg 17:39. https://doi.org/10.1186/s12893-017-0232-z
Gurusamy KS, Giljaca V, Takwoingi Y, Higgie D, Poropat G, Štimac D, Davidson BR (2015) Endoscopic retrograde cholangiopancreatography versus intraoperative cholangiography for diagnosis of common bile duct stones. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD010339.pub2
Cennamo V, Fuccio L, Zagari RM, Eusebi LH, Ceroni L, Laterza L, Fabbri C, Bazzoli F (2010) Can early precut implementation reduce endoscopic retrograde cholangiopancreatography-related complication risk? Meta-analysis of randomized controlled trials. Endoscopy 42:381–388. https://doi.org/10.1055/s-0029-1243992
Topal B, Aerts R, Penninckx F (2007) Laparoscopic common bile duct stone clearance with flexible choledochoscopy. Surg Endosc 21:2317–2321. https://doi.org/10.1007/s00464-007-9577-1
Williams EJ, Green J, Beckingham I, Parks R, Martin D, Lombard M (2008) Guidelines on the management of common bile duct stones (CBDS). Gut 57:1004–1021. https://doi.org/10.1136/gut.2007.121657
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Ammori BJ, Birbas K, Davides D, Vezakis A, Larvin M, McMahon MJ (2000) Routine vs “on demand” postoperative ERCP for small bile duct calculi detected at intraoperative cholangiography. Clinical evaluation and cost analysis. Surg Endosc 14:1123–1126. https://doi.org/10.1007/s004640000146
Attasaranya S, Cheon YK, Vittal H, Howell DA, Wakelin DE, Cunningham JT, Ajmere N, Ste Marie RW, Bhattacharya K, Gupta K, Freeman ML, Sherman S, McHenry L, Watkins JL, Fogel EL, Schmidt S, Lehman GA (2008) Large-diameter biliary orifice balloon dilation to aid in endoscopic bile duct stone removal: a multicenter series. Gastrointest Endosc 67:1046–1052. https://doi.org/10.1016/j.gie.2007.08.047
Kim H, Shin SP, Hwang JW, Lee JW (2020) Outcomes of laparoscopic common bile duct exploration (LCBDE) after failed endoscopic retrograde cholangiopancreatography versus primary LCBDE for managing cholecystocholedocholithiasis. J Int Med Res 48:0300060520957560. https://doi.org/10.1177/0300060520957560
Ghazala S, Pokhrel B, Shrestha MP, Junna S, Cunningham J, Gavini H (2017) Common bile duct stone size is an independent predictor of stone detection by magnetic resonance imaging: 85. Am J Gastroenterol 112:S38
Topal B, Vromman K, Aerts R, Verslype C, Van Steenbergen W, Penninckx F (2010) Hospital cost categories of one-stage versus two-stage management of common bile duct stones. Surg Endosc 24:413–416. https://doi.org/10.1007/s00464-009-0594-0
Mattila A, Mrena J, Kellokumpu I (2017) Cost-analysis and effectiveness of one-stage laparoscopic versus two-stage endolaparoscopic management of cholecystocholedocholithiasis: a retrospective cohort study. BMC Surg 17:79. https://doi.org/10.1186/s12893-017-0274-2
Morton A, Cralley A, Brooke-Sanchez M, Pieracci FM (2022) Laparoscopic common bile duct exploration by acute care surgeons saves time and money compared to ERCP. Am J Surg 224:116–119. https://doi.org/10.1016/j.amjsurg.2022.03.026
Martin IJ, Bailey IS, Rhodes M, O’Rourke N, Nathanson L, Fielding G (1998) Towards T-tube free laparoscopic bile duct exploration: a methodologic evolution during 300 consecutive procedures. Ann Surg 228:29–34. https://doi.org/10.1097/00000658-199807000-00005
Hajibandeh S, Hajibandeh S, Sarma DR, Balakrishnan S, Eltair M, Mankotia R, Budhoo M, Kumar Y (2019) Laparoscopic transcystic versus transductal common bile duct exploration: a systematic review and meta-analysis. World J Surg 43:1935–1948. https://doi.org/10.1007/s00268-019-05005-y
Tokumura H, Umezawa A, Cao H, Sakamoto N, Imaoka Y, Ouchi A, Yamamoto K (2002) Laparoscopic management of common bile duct stones: transcystic approach and choledochotomy. J Hepatobiliary Pancreat Surg 9:206–212. https://doi.org/10.1007/s005340200020
Berthou JCh, Dron B, Charbonneau Ph, Moussalier K, Pellissier L (2007) Evaluation of laparoscopic treatment of common bile duct stones in a prospective series of 505 patients: indications and results. Surg Endosc 21:1970–1974. https://doi.org/10.1007/s00464-007-9387-5
Kim TH, Oh HJ, Lee JY, Sohn YW (2011) Can a small endoscopic sphincterotomy plus a large-balloon dilation reduce the use of mechanical lithotripsy in patients with large bile duct stones? Surg Endosc 25:3330–3337. https://doi.org/10.1007/s00464-011-1720-3
Karsenti D (2013) Endoscopic management of bile duct stones: residual bile duct stones after surgery, cholangitis, and “difficult stones.” J Visc Surg 150:S39–S46. https://doi.org/10.1016/j.jviscsurg.2013.05.002
Zhang W, Xu G, Huang Q, Luo K, Dong Z, Li J, Wu G, Guan W (2015) Treatment of gallbladder stone with common bile duct stones in the laparoscopic era. BMC Surg 15:7. https://doi.org/10.1186/1471-2482-15-7
Kelly T, Parikh M, Pachter HL (2020) Laparoscopic common bile duct exploration. Laparosc Surg 4:16. https://doi.org/10.21037/ls.2019.12.06
the SAGES Guidelines Committee, Narula VK, Fung EC, Overby DW, Richardson W, Stefanidis D (2020) Clinical spotlight review for the management of choledocholithiasis. Surg Endosc 34:1482–1491. https://doi.org/10.1007/s00464-020-07462-2
Lyu Y, Cheng Y, Li T, Cheng B, Jin X (2019) Laparoscopic common bile duct exploration plus cholecystectomy versus endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for cholecystocholedocholithiasis: a meta-analysis. Surg Endosc 33:3275–3286. https://doi.org/10.1007/s00464-018-06613-w
Pan L, Chen M, Ji L, Zheng L, Yan P, Fang J, Zhang B, Cai X (2018) The safety and efficacy of laparoscopic common bile duct exploration combined with cholecystectomy for the management of cholecysto-choledocholithiasis: an up-to-date meta-analysis. Ann Surg 268:247–253. https://doi.org/10.1097/SLA.0000000000002731
Ng T, Amaral JF (1999) Timing of endoscopic retrograde cholangiopanereatography and laparoscopic cholecystectomy in the treatment of choledocholithiasis. J Laparoendosc Adv Surg Tech 9:31–37. https://doi.org/10.1089/lap.1999.9.31
Acknowledgements
Alison Perko for her assistance in data extraction.
Funding
No funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Gloria Sanin, Gabriel Cambronero, James Patterson, Maggie Bosley, Aravindh Ganapathy, Carl Wescott, and Lucas Neff have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Presented at SAGES 2023, Montreal, Canada.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sanin, G., Cambronero, G., Patterson, J. et al. ERCP findings provide further justification for a “surgery-first” mindset in choledocholithiasis. Surg Endosc 37, 8714–8719 (2023). https://doi.org/10.1007/s00464-023-10329-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10329-x