Abstract
Background: Two-port laparoscopic cholecystectomy has been reported to be safe and feasible. However, whether it offers any additional advantages remains controversial. This study reports a randomized trial that compared the clinical outcomes of two-port laparoscopic cholecystectomy versus conventional four-port laparoscopic cholecystectomy. Methods: One hundred and twenty consecutive patients who underwent elective laparoscopic cholecystectomy were randomized to receive either the two-port or the four-port technique. All patients were blinded to the type of operation they underwent. Four surgical tapes were applied to standard four-port sites in both groups at the end of the operation. All dressings were kept intact until the first follow-up 1 week after surgery. Postoperative pain at the four sites was assessed on the first day after surgery using a 10-cm unscaled visual analog scale (VAS). Other outcome measures included analgesia requirements, length and difficulty of the operation, postoperative stay, and patient satisfaction score on surgery and scars. Results: Demographic data were comparable for both groups. Patients in the two-port group had shorter mean operative time (54.6 ± 24.7 min vs 66.9 ± 33.1 min for the four-post group; p = 0.03) and less pain at individual subcostal port sites [mean score using 10-cm unscaled VAS: 1.5 vs 2.8 (p = 0.01) at the midsubcostal port site and 1.3 vs 2.3 (p = 0.02) at the lateral subcostal port site]. Overall pain score, analgesia requirements, hospital stay, and patient satisfaction score on surgery and scars were similar between the two groups. Conclusion: Two-port laparoscopic cholecystectomy resulted in less individual port-site pain and similar clinical outcomes but fewer surgical scars compared to four-port laparoscopic cholecystectomy. Thus, it can be recommended as a routine procedure in elective laparoscopic cholecystectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic cholecystectomy (LC) has replaced open cholecystectomy as the standard procedure for gallbladder removal whenever possible. Recent developments regarding LC have been directed toward reducing the size or number of ports to achieve the goal of minimal invasive surgery [1, 2, 4, 5, 6, 7, 8]. The utilization of laparoscopes with operating channels made two-port LC technically feasible [5, 7]. Although several case series have reported the advantages of two-port LC in terms of better patient satisfaction and less postoperative pain, none have compared two-port LC with the conventional four-port LC in a randomized manner [5, 6, 8]. Whether two-port LC is superior to conventional LC has not been determined in the literature. We report a prospective randomized controlled trial that compared the clinical outcomes of two-port laparoscopic cholecystectomy versus conventional laparoscopic cholecystectomy.
Materials and methods
We prospectively recruited consecutive patients aged 18–75 who were indicated for elective LC into this study. Exclusion criteria included patients with bleeding tendency (International normalized ratio [INR] > 1.5 or platelet count < 100 × 109) or American Society of Anesthesiologist class III or higher. All procedures were performed or closely supervised by experienced specialist laparoscopic surgeons who had performed more than 100 conventional LCs and at least 20 two-port LCs prior to the study. All patients signed informed consent for the randomization and procedure.
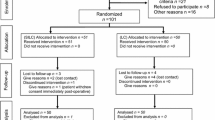
Patients were randomized to receive either two-port (two-port group) or conventional LC (four-port group) after satisfactory general anesthesia. An 11-mm supraumbilical port, a 5-mm subxyphoid port, and two 5-mm subcostal ports were used in four-port LC. We adopted the single surgeon technique in the four-port LC using zero-degree operating telescopes. In two-port LC, an 11-mm supraumbilical port and 5-mm subxyphoid port were used. Our technique for two-port LC has been reported elsewhere [5, 7]. Briefly, we used a modified operating telescope (Karl Storz 26036A zero degree; Fig. 1) that was inserted into the supraumbilical port. Retraction of gallbladder was done by the long grasping forceps through the operating telescope, whereas dissection was accomplished through the 5-mm subxyphoid port. Additional 5-mm subcostal ports or percutaneous sling-through sutures could be added when necessary. The cystic duct and cystic artery were clipped by a 5-mm multiple clip applicator in both groups (Allport ML326, Ethicon). The gallbladder was retrieved through the umbilical port without changing the position of the operating telescope. Non-transparent surgical adhesive tape was applied to the standard four-port sites at the end of the operation in both groups (Fig. 2). All wound dressings were kept intact until the first follow-up 1 week after surgery. Thus, all patients were blinded to the type of operation they underwent. Intramuscular pethidine (1 mg/kg) was given every 4 h as requested for postoperative pain control. Our primary outcome measure was pain score and analgesia requirements after surgery. An independent doctor assessed the pain score by using a 10-cm unscaled visual analog scale (VAS) for each dressing site and the overall pain on the first day after the operation. Several other outcome measures were used. First was length of operation and operative difficulty: the operative time was recorded from the beginning of the first incision until closure of the final wound. Operative surgeons also graded the difficulty of the operation using a 10-cm unscaled VAS (0, easy; 10, difficult). Second was patient satisfaction score on surgery: an independent assessor determined the satisfaction score using a 10-cm unscaled VAS on the day of discharge. Third was post-operative stay: patients were discharged if they had satisfactory pain control and were able to tolerate their usual diet. The assessment was made by an independent specialist surgeon who did not know the type of surgery that the patient underwent. Fourth was patient satisfaction score on scars: all patients were reviewed 1 week after surgery by an independent doctor to assess the satisfaction score on the scar using a 10-cm unscaled VAS (0, unsatisfied; 10, very satisfied).
The sample size was calculated based on the assumption that there would be a 30% reduction in overall pain score in the two-port LC group. With a p value of 0.05 and a power of 80%, it was calculated that it was necessary to include at least 55 patients in each group. Parametric summary statistics were presented as means with standard deviations (±SD), whereas nonparametric summary statistics were presented as medians with interquartile range. Categorical data were analyzed using Pearson’s chi-square test or Fisher’s exact test as appropriate. The two-sample t-test was used to test the hypothesis of equality of means, and the Mann–Whitney U-test was used to test the hypothesis of equality of medians. A p value < 0.05 was considered statistically significant. Statistical Package for Social Science (SPSS) Version 9.0 for Windows (SPSS, Cary, NC, USA) was used for statistical analysis.
Results
From November 2000 to July 2001, 120 consecutive patients were recruited for this study. Five patients were excluded after randomization. One patient in the two-port group was found to have carcinoma of the gallbladder during laparoscopy. Another 4 patients (1 in the two-port group and 3 in the four-port group) violated the protocol due to use of ports that were the wrong size. The final analysis included 115 patients. The demographic data and indications for cholecystectomy were comparable in both groups (Table 1). The mean scores for the difficulty of the operation (3.2 ± 3.0 for the two-port group vs 3.6 ± 3.0 for the four-post group; p = 0.53) were similar (Table 2). Five of 58 patients (8.6%) in the two-port group required an additional 5-mm subcostal port or a percutaneous sling to aid dissection. There was no difference in open conversion rate among the two groups [3/58 (5.2%) in the two-port group vs 2/58 (3.4%) in the four-port group; p = 1.00]. The two-port group had a significantly shorter mean operative time than the four-port group (54.6 ±24.7 min vs 66.0 ± 32.6 min; p = 0.04). The majority of procedures were performed by senior surgical residents under supervision (Table 2). For the postoperative pain assessment, the two-port group had significantly less pain at individual subcostal port sites [mid subcostal port site C, 1.5 ± 2.2 vs 2.8 ± 2.7 (p = 0.01); lateral subcostal port site D; 1.3 ± 2.0 vs 2.3 ± 2.4 (p = 0.02), Table 3]. However, the mean overall pain score was similar in the two groups (4.5 ± 2.3 for the two-port group vs 4.6 ± 2.5 for the four-port group; p = 0.72). Also, there was no difference in terms of analgesia requirement among the two groups. The median hospital stay was 2 days in both groups (Table 3). The four-port group had higher overall complication rate than the two-port group (8 vs 3, respectively), but this did not reach the level of significance. One patient in the two-port group was complicated by intratabdominal collection and was managed conservatively. Three patients in the four-port group had common bile duct stone(s) after surgery. These patients had normal liver function tests before surgery. All the stones were successfully removed by endoscopic retrograde cholangiopancretiography (ERCP) subsequently. One patient in the four-port group developed severe abdominal pain on the first day after surgery. An emergency laparoscopy was performed that showed no abnormality and the patient made an uneventful recovery. The mean patient satisfaction score on surgery was not different among the two groups 8.7 ± 1.6 for the two-port group vs 8.3 ± 2.0 for the four-port group; p = 0.28). Similarly, there was no significant difference among the two groups regarding the mean patient satisfaction score on the scar on day 7 (8.7 ± 1.7 for the two-port group vs 8.3 ± 1.7 for the four-port group; p = 0.24).
Discussion
In the era of laparoscopic surgery, less postoperative pain and early recovery are major goals in order to achieve better patient care and cost-effectiveness. Several studies demonstrated that less postoperative pain was associated with reduction in either size or number of ports [1, 4, 6, 8]. In the current study, we failed to demonstrate any difference in terms of overall pain score or analgesia requirements among the two groups. However, it is conceivable that less pain is associated with the site at which no incision was made, and this was proven in our double-blind study. The median hospital stay was 2 days for both groups. Although our primary aim was not to perform these laparoscopic cholecystectomies as outpatient procedures, we believe that with defined protocols, both techniques can be safely performed as day case procedures. The majority of procedures in this study were performed by senior surgical residents supervised by specialists. The scoring on difficulty of operation was not different among the two groups of surgeons. It was also interesting that the mean operative time was shorter for the two-port LC group. One explanation for the shorter operative time is that less time was spent on the establishment and subsequent closure of subcostal ports. These results suggest that the technique of two-port LC was not difficult to master and could be safely performed by trained personnel. Although needlescopic cholecystectomy is technically demanding [1], two-port LC may be a viable alternative in the field of minimal invasive laparoscopic cholecystectomy.
Most of the complications in this series were related to wound infections. It was noteworthy that three patients in the four-port LC group presented with impairment of liver function tests after surgery and were later found to have common bile duct stones. Although all cases were adequately managed with ERCP stone removal, this raised the question of the value of routine intraoperative cholangiography during laparoscopic cholecystectomy [3, 9]. We performed intraoperative cholangiogram using a two-port technique on selected cases, and we found that the technique was not more difficult to perform than the conventional one. Nonetheless, we are awaiting final results of this new technique before we make any conclusions.
Most of our patients reported high satisfaction for the surgery and the surgical scars in both groups. Although there was a higher observed satisfaction score for the two-port LC group, this did not reach statistical significance.
To conclude, we demonstrated in this study that two-port LC is safe and has similar clinical outcomes compared to the conventional four-port LC in selective cases. Since two-port LC has less surgical scars, it can be recommended as a routine technique.
References
T Bisgaard B Klarskov R Trap H Kehlet J Rosenberg (2000) ArticleTitlePain after microlaparoscopic cholecystectomy. A randomized double blind controlled study. Surg Endosc 14 340–344
WK Cheah JE Lenzi JB So CK Kum PM Goh (2001) ArticleTitleRandomized trial of needlescopic versus laparoscopic cholecystectomy. Br J Surg 88 45–47 Occurrence Handle10.1046/j.1365-2168.2001.01636.x Occurrence Handle1:STN:280:DC%2BD3M7isFGnsA%3D%3D Occurrence Handle11136308
A Cuschieri S Shimi S Banting LK Nathanson A Pietrabissa (1994) ArticleTitleIntraoperative cholangiography during laparoscopic cholecystectomy. Routine vs selective policy. Surg Endosc 8 302–305
PL Leggett R Churchman-Winn R Miller (2000) ArticleTitleMinimizing ports to improve laparoscopic cholecystectomy. Surg Endosc 14 32–36
KF Leung KW Lee TY Cheung LC Leung KW Lau (1996) ArticleTitleLaparoscopic cholecystectomy: two-port technique. Endoscopy 6 505–507
D Lomanto L De Angelis V Ceci G Dalsasso J So FM Frattaroli R Muthiah V Speranza (2001) ArticleTitleTwo-trocar laparoscopic cholecystectomy: a reproducible technique. Surg Laparosc Endosc Percutan Tech 11 248–251 Occurrence Handle1:STN:280:DC%2BD3Mvot1CisQ%3D%3D Occurrence Handle11525369
CM Poon KW Chan CW Ko KC Chan DW Lee HY Cheung KW Lee (2002) ArticleTitleTwo-port laparoscopic cholecystectomy: initial results of a modified technique. J Laparoendosc Adv Surg Tech A 12 259–262 Occurrence Handle10.1089/109264202760268032 Occurrence Handle12269493
CS Ramachandran V Arora (1998) ArticleTitleTwo-port laparoscopic cholecystectomy: an innovative new method for gallbladder removal. J Laparoendosc Adv Surg Tech A 8 303–308 Occurrence Handle1:STN:280:DyaK1M%2Fjs1Kjuw%3D%3D Occurrence Handle9820723
NJ Soper DL Dunnegan (1992) ArticleTitleRoutine versus selective intra-operative cholangiography during laparoscopic cholecystectomy. World J Surg 16 1133–1140 Occurrence Handle1:STN:280:ByyD1cfot1E%3D Occurrence Handle1455885
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Poon, C., Chan, K., Lee, D. et al. Two-port versus four-port laparoscopic cholecystectomy . Surg Endosc 17, 1624–1627 (2003). https://doi.org/10.1007/s00464-002-8718-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-002-8718-9