Abstract
Tongue base pressures have been thought to provide primary bolus clearance through the pharynx during swallowing. The relationship between bolus driving pressures and residue remaining in the valleculae after the swallow has not been defined. Thirty-seven dysphagic patients who were evaluated with both videofluoroscopy (VFSS) and high-resolution manometry (HRM) were identified within the University of Wisconsin Voice and Swallowing Outcomes database. Patients were categorized according to binary ratings of presence or absence of vallecular stasis as well as incomplete or complete tongue retraction on VFSS. Tongue base region pressures measured with HRM during saline swallows of 1 and 10 ml volumes were compared to ratings of vallecular stasis or tongue base retraction. No significant difference could be identified among mean peak HRM pressures when compared to presence or absence of vallecular stasis (1 ml saline: p = .1886; 10 ml saline: p = .7354). When categorized according to complete or incomplete tongue retraction, mean peak HRM pressures were significantly greater in the complete tongue retraction group as compared to incomplete tongue retraction (1 ml saline: p = .0223; 10 ml saline: p = .0100). Findings suggest there are multiple factors that lead to reduced vallecular clearance. In the absence of HRM measures, judging complete or incomplete tongue retraction on VFSS may be a more valid gauge of tongue base region pressures than vallecular clearance when planning dysphagia treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It has long been postulated that tongue base pressures account for clearance of bolus material through the oropharyngeal spaces during swallowing [1]. Pressures generated at the tongue base have been studied in normal human subjects, identifying fine modulation of swallowing pressures in response to varying bolus volumes and textures [2, 3]. Pharyngeal wall contributions to bolus clearance have also been defined, though it has been suggested they play a minor role in propulsive force [4, 5]. The significance of hyoid excursion to facilitate epiglottic inversion and subsequent vallecular clearance has also been shown [6]. In older adults without dysphagia, those with age-associated vallecular retention showed significantly reduced tongue base pressures against a uni-directional manometric sensor [7]. Given the proximity of the tongue base to the valleculae, it would seem feasible that tongue base pressures would account for clearance of bolus material through these spaces.
The propulsive force of the tongue base has been described as “pistonlike” in its rapid displacement of contrast from the oropharynx through the upper esophageal sphincter (UES) [8]. Reduced tongue base contact with the posterior pharyngeal wall has been associated with vallecular retention of bolus residue in both videofluoroscopic swallowing study (VFSS) and fiberoptic endoscopic evaluation of swallowing (FEES). VFSS examinations of head/neck cancer patients performed concurrent with manometry featuring two pressure sensors correlated increased duration and amplitude of tongue base pressures with reduced transit time and bolus residue [9]. However, little remains understood about the mechanism of vallecular clearance and the relationship to tongue base pressures in disordered swallowing.
Incomplete bolus clearance in the valleculae has been significantly associated with aspiration and is considered a predictor of aspiration risk [10, 11]. Standard swallowing assessments such as VFSS or FEES can detect presence of vallecular stasis when barium contrast administered in VFSS, or opaque food and liquid in FEES, remains within the vallecular spaces following swallows. Clinical interpretation of swallowing imaging has been plagued by poor reliability when graded ratings of vallecular residue, hyolaryngeal excursion, or tongue propulsion are applied [12–15]. Visual perceptual measurements in FEES or VFSS imaging cannot offer the objective measurement required to analyze the role of tongue base pressures in vallecular clearance.
With the advent of high-resolution manometry (HRM) offering refined pressure measurements for pharyngoesophageal swallow analysis, application of HRM as a diagnostic tool in complex dysphagia care has been initiated [16]. Investigation of pressures generated at the tongue base region in dysphagic patients may help define the relationship between tongue base pressures and vallecular clearance. If a relationship between tongue base movement and vallecular clearance exists, it becomes important to consider how standard diagnostic tools can objectively assess impairment as well as treatment outcomes. The purpose of this study was to investigate the relationship between tongue base region pressures and vallecular clearance. It was hypothesized that manometric measures at the tongue base region in patients with vallecular stasis after swallows on VFSS would differ significantly from tongue base region pressures in patients without vallecular stasis. A secondary hypothesis that manometric measures at the tongue base region in patients with incomplete tongue base retraction on VFSS would differ from those with complete retraction against the posterior pharyngeal wall was proposed.
Methods
Participants
This retrospective review of a prospective disease-specific outcomes database was conducted using the University of Wisconsin Madison Voice and Swallow Outcomes Database. Establishment and subsequent use of the database has been approved by the University of Wisconsin Madison School of Medicine and Public Health Institutional Review Board. Information in the database is obtained with patient consent for those who visit the Otolaryngology Head and Neck Clinic for a complaint related to voice and swallow and includes patient health information for over 4000 persons. This study sample consisted of patients over the age of 18 during the period of November 2012 to May 2014.
Patients were identified in the database by diagnosis of dysphagia. Additionally, completion of both VFSS and HRM evaluation was required with a maximum of 45 days interval and no documented functional change or medical/surgical procedures between exams. Patients with an interval exceeding 45 days between exams or who underwent procedures that may have changed their swallowing function were excluded. Demographic variables (age, sex), dysphagia severity rating, date and type of visit (VFSS vs. HRM) for selected subjects were also retrieved from the database (Table 1).
Procedures
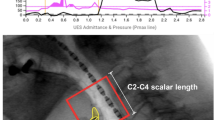
VFSS and HRM studies were performed by trained speech pathologists at University of Wisconsin (UW) Voice and Swallow Clinics in accordance with institution policies for peer-reviewed competence. VFSS ratings of presence or absence of vallecular stasis, complete or incomplete tongue base retraction, and penetration/aspiration scale (PAS) scores [17] were obtained from the database. Clinician judgments of dysphagia severity were also extracted, characterized by a 7-point ordinal scale representing normal function to severe impairment. Severity levels were subjectively assigned by the clinician based on functional estimates of dependence on swallowing maneuvers or strategies for safe oral intake, degree of diet modification advised, and use of alternative means for achieving nutritional intake. PAS ratings extracted included 5 ml Varibar Thin barium contrast via cup, 10–30 ml Varibar Thin via cup, 5 ml Varibar Pudding via spoon, and ½ Wanda’s Barium Cookie. The highest rating on the 8-point PAS, representing the poorest performance on a given bolus trial, was selected from the extracted data to represent each texture/volume grouping. Single ratings were recorded by clinicians to represent presence or absence of vallecular stasis and complete or incomplete tongue retraction for each VFSS and were not volume or texture specific. HRM data for the tongue base region were extracted, including peak pressure measures averaged across three trials for 1 and 10 ml volumes of saline. Patients were divided into groups according to presence or absence of stasis for testing against the primary hypothesis. Patients were then divided into complete and incomplete retraction groups to address the secondary hypothesis for comparison.
Statistical Analysis
Statistical analysis was performed using SAS statistical software (version 9.2, SAS Institute Inc., Cary, NC). All groups were analyzed for differences in sex, dysphagia severity rating and tongue retraction by testing with Fisher’s exact test. Age was tested both as a continuous variable with a two-tailed, two-sample Satterthwaite method t test, as well as a categorical variable with Fisher’s exact test to determine any differences in representation of older adults ≥70 years of age. Two-tailed, two-sample Satterthwaite method t tests were calculated for PAS scores for 5 ml thin liquid, semisolid and solid bolus types due to unequal variances. Examination interval, PAS scores for thin liquid by cup, and manometric measures of 1 and 10 ml volumes of saline were analyzed using two-tailed, two-sample pooled t tests given relatively equal variances among groups. Analysis for the retraction groups mirrored the same testing for sex, dysphagia severity, categorical age, PAS scores, and HRM measures. Age as a continuous variable was analyzed using two-tailed, two-sample pooled t tests as age variances between retraction groups were relatively equal. Conversely, examination interval was analyzed using two-tailed, two-sample Satterthwaite method t tests due to unequal variances between the tongue retraction groups.
Results
Demographics
Data were extracted from the database for the thirty-seven patients meeting inclusion and exclusion criteria and included a total of 23 males and 14 females. Mean age of participants across groups was 65 years (SD = 14 years). Mean duration of interval between examinations for the sample was 9 days (SD = 14 days). The largest proportion of patients, 38 %, was rated to have mild-moderate severity of dysphagia and represented the mode of the sample. The remainder of the sample’s dysphagia severity ratings were distributed as follows: functional 8 %, minimal 8 %, mild 19 %, moderate 16 %, moderate-severe 8 %, and severe 3 %.
Data were divided according to stasis ratings on VFSS, resulting in a “stasis” group (n = 29) and a “no stasis” group (n = 8). Sex, age, and dysphagia severity proportions of the sample are described in Table 1. Sex appeared to be associated with presence of stasis, p = .0345, with 91 % of the sample’s males falling into the stasis group. Mean age for the stasis group was 65.4 years (SD = 11.6 years) and 63.5 years (SD = 22.4 years) for the no stasis group. Age was not found to be significantly associated with presence of stasis for either continuous age analysis or when categorized as under/over 70 years of age (p = .8184 and p = 1.0, respectively). Mean evaluation interval for patients with vallecular stasis was 10.8 days (SD = 14.74 days), and for those without vallecular stasis, 2.63 days (SD = 7.42 days); there was no significant difference for time interval between stasis groups (p = .1415). Dysphagia severity at the time of VFSS as rated on a 7-point scale was not significantly different between vallecular stasis groups (p = .3388).
The sample was secondarily divided into groups according to tongue retraction ratings on VFSS. Due to a missing rating for tongue retraction in one sample unit, the total sample for analysis was 36 patients. Sex, age, and exam interval data for the tongue base retraction rating groups are represented in Table 2. A larger proportion of males (n = 15) comprised the incomplete retraction group, but males and females were equally represented in the complete retraction group (n = 8 for each sex). Sex differences were not shown to be significant, p = .1691. Mean age for the incomplete retraction group was 66.8 years (SD = 11.9) and 62.2 (SD = 17 years) for the complete retraction group. Age was not shown to be significantly different between tongue base retraction groups for continuous or categorical age analysis, p = .3398 and p = .7182, respectively. Examination intervals were also compared, showing a significant difference (p = .0104) in the number of days from VFSS to manometric measurement between the complete tongue retraction (mean = 3.1 days; SD = 7.2 days) and incomplete tongue retraction (mean = 14.2 days; SD = 16.1 days) groups. Dysphagia severity distribution mode for the full sample was the “mild-moderate” rating; however, the incomplete retraction group data is shifted toward “severe” while the complete retraction group is distributed near “functional”. The association between severity and retraction ratings was tested to be significant at p = .0325.
Vallecular Stasis
Mean peak manometry measures and PAS scores for each stasis group are shown in Table 3. For patients with vallecular stasis, mean peak manometric measurements for 1 ml saline (mean = 133.4 mmHg; SD = 47.5 mmHg) and 10 ml saline (mean = 142.9 mmHg; SD = 58.5 mmHg) showed no significant difference (p = .1886 and p = .7354, respectively) from those without stasis for both 1 ml saline (mean = 166.2 mmHg; SD = 81.4 mmHg) and 10 ml saline (mean = 151 mmHg; SD = 44.4 mmHg). PAS scores for thin liquids administered in 5 ml and cup volumes were significantly associated with clinician stasis ratings, p = .0012 and p = .0127, respectively. PAS scores for pudding and solid were not significantly related (p = .1341 and p = .1426).
Tongue Retraction
Mean peak manometric measures for the incomplete and complete retraction groups are listed in Table 4. Manometric measures of the tongue base region in the incomplete retraction group (1 ml: mean = 121.5 mmHg, SD = 45.3 mmHg; 10 ml: mean = 124.6 mmHg, SD = 45.3 mmHg) were significantly different from the complete retraction group (1 ml: mean = 164.5 mmHg, SD = 59 mmHg; 10 ml: mean = 173.9 mmHg, SD = 56.2 mmHg), with p = .0223 and p = .01 for respective saline volumes presented during manometry. PAS scores for 5 ml and cup drinking with thin liquids both demonstrated significant relationships to clinician ratings of tongue retraction on VFSS, p < .001 for both PAS groups. PAS scores for pudding and solid were not significant, p = .1351 and p = .1441, respectively. Clinician ratings of incomplete tongue retraction to the posterior pharyngeal wall on VFSS imaging showed a strong relationship with presence of vallecular stasis, p = .0014.
Discussion
This study of tongue base region manometric pressures as compared to presence of vallecular stasis suggests that there is not an explicit relationship between tongue base region pressure generation and bolus clearance. No significant differences in manometric pressure measures were evident between individuals rated with vallecular stasis when compared to those without stasis, supporting that there must be multiple physiologic contributions to vallecular stasis in oropharyngeal dysphagia.
A significant relationship was identified between clinician ratings of tongue retraction and vallecular stasis as judged on VFSS. Closer examination of the data reveals that all 20 participants with ratings of incomplete tongue base retraction also exhibited vallecular stasis, while the 16 individuals with complete tongue base retraction were divided between ratings of no stasis and stasis. It would be important to further investigate this relationship with a prospective design that may assure independence between the stasis and retraction ratings through controlled training and rating processes. Trained clinician ratings comparing tongue base retraction during real-time videofluoroscopy of non-swallow tasks demonstrated high agreement with actual measures [18]. However, binary ratings of tongue base retraction during swallows by experienced clinicians without training or definition have shown low inter-rater reliability [19]. The role of standardization in videofluoroscopic judgments is indisputable.
Tongue base retraction ratings on VFSS were significantly correlated to peak manometric measures at the tongue base region. This finding makes the division of stasis presence or absence among individuals with complete tongue retraction more compelling, suggesting that factors other than impaired pressure generation at the tongue base region can account for vallecular stasis. Such factors have been implied in the literature, including fibrosis of the epiglottis or xerostomia [6]. When HRM is not clinically available for pressure measurements, clinician judgments of tongue retraction to the posterior pharyngeal wall may offer a representation of tongue base region pressure generation for bolus clearance. No prior studies have systematically investigated the validity of interpreting tongue base retraction on VFSS as a representation of tongue base pressure. The binary tongue retraction ratings used in this study do not provide detailed assessment for treatment planning or post-treatment comparison. Manometric measurement promises finer resolution for comparing patient performance against functional thresholds at the tongue base region to support patient-reported outcomes following dysphagia treatment.
The use of an outcomes database for this study warrants consideration in interpreting these results. The intervals between VFSS and manometric examinations varied from 0 to 45 days. While 68 % of exams were completed within 7 days, the testing interval could not be controlled to assure equivalent performance at both examinations. The significant difference in examination intervals analyzed between the retraction groups may be a function of the clinical model for manometry, where more severely dysphagic patients may coordinate a manometric evaluation with an appointment for ENT consultation weeks following their imaging study. It is also important to acknowledge that manometric measures in the present study were collected during liquid swallows, while judgments of vallecular stasis and tongue retraction on VFSS were not associated with any defined texture. While all patients included in this study had manometric data for analysis, missing data points within the manometry data are presumed to relate to individualized protocol adjustments based upon patient aspiration risk. Furthermore, the study sample represented a range of age and dysphagia severity, though males comprised more of the vallecular stasis group. Future study should endeavor to control exam intervals, testing protocols, and age and sex representation within groups to account for potential differences.
Retention of bolus residue presents implications for patient health that underscores the importance of understanding causes for stasis. Depth of penetration or aspiration was significantly related to the presence of vallecular stasis in this study, which is consistent with prior studies demonstrating the relationship [10, 11]. However, critical tongue base pressure thresholds that may relate to pharyngeal dysphagia are not yet defined. Establishing functional pressure thresholds will be vital in differentiating tongue base region contributions from other mechanical effects on vallecular clearance when designing exercise protocols for treating complex dysphagia. In the absence of objective measurement with HRM, best practice in gauging pressure generation at the tongue base may depend upon careful consideration of tongue base retraction to the posterior pharyngeal wall during imaging studies.
References
McConnell FMS, Cerenko D, Jackson RT, Guffin TN. Timing of major events of pharyngeal swallowing. Arch Otolaryngol Head Neck Surg. 1988;114:1413–8.
Pouderoux P, Kahrilas PJ. Deglutitive tongue force modulation by volition, volume and viscosity in humans. Gastroenterology. 1995;108:1418–26.
Hoffman MR, Ciucci MR, Mielens JD, et al. Pharyngeal swallow adaptations to bolus volume measured with high-resolution manometry. Laryngoscope. 2010;120:2367–734.
Palmer JB, Tanaka E, Siebens A. Motions of the posterior pharyngeal wall in swallowing. Laryngoscope. 1988;98:414–7.
Kahrilas PJ, Logemann JA, Lin S, Ergun GA. Pharyngeal clearance during swallowing: a combined manometric and videofluoroscopic study. Gastroenterology. 1992;103:128–36.
Perlman AL, Grayhack JP, Booth BM. The relationship of vallecular residue to oral involvement, reduced hyoid elevation, and epiglottic function. J Speech Hear Res. 1992;35:734–41.
Dejaeger E, Pelemans W, Ponette E, Joosten E. Mechanisms involved in postdeglutition retention in the elderly. Dysphagia. 1997;12:63–7.
Dodds WJ, Stewart ET, Logemann JA. Physiology and radiology of the normal oral and pharyngeal phases of swallowing. Am J Roentgenol. 1990;154:953–63.
Pauloski BR, Rademaker AW, Lazarus C, Boeckxstaens G, Kahrilas PJ, Logemann JA. Relationship between manometric and videofluoroscopic measures of swallow function in healthly adults and patients treated for head and neck cancer with various modalities. Dysphagia. 2009;24:196–203.
Perlman AL, Booth BM, Grayhack JP. Videofluoroscopic predictors of aspiration in patients with oropharyngeal dysphagia. Dysphagia. 1994;9:90–5.
Molfenter SM, Steele CM. The relationship between residue and aspiration on the subsequent swallow: an application of the normalized residue ratio scale. Dysphagia. 2013;28:494–500.
Kuhlemeier KV, Yates P, Palmer JB. Intra- and interrater variation in the evaluation of videofluorographic swallowing studies. Dysphagia. 1998;13:142–7.
Scott AS, Perry A, Bench J. A study of interrater reliability when using videofluoroscopy as an assessment of swallowing. Dysphagia. 1998;13:223–7.
McCullough GH, Wertz RT, Rosenbeck JC, Mills RH, Webb WG, Ross KB. Inter- and intrajudge reliability for videofluoroscopic swallowing evaluation measures. Dysphagia. 2001;16:110–8.
Bryant KN, Finnegan E. VFS interjudge reliability using a free and directed search. Dysphagia. 2011;27:53–63.
Knigge MA, Thibeault S, McCulloch TM. Implementation of high-resolution manometry in the clinical practice of speech language pathology. Dysphagia. 2014;29:2–16.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11:93–8.
Veis S, Logemann JA, Colangelo L. Effects of three techniques on maximum posterior movement of the tongue base. Dysphagia. 2000;15:142–5.
Stoeckli SJ, Huisman TAGM, Seifert B, Martin-Harris BJW. Interrater reliability of videofluoroscopic swallow evaluation. Dysphagia. 2003;18:53–7.
Acknowledgments
The authors would like to thank Glen Leverson, PhD for his statistical assistance
Funding
This work was funded by the Diane M. Bless Endowed Chair.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Knigge, M.A., Thibeault, S. Relationship Between Tongue Base Region Pressures and Vallecular Clearance. Dysphagia 31, 391–397 (2016). https://doi.org/10.1007/s00455-015-9688-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-015-9688-0