Abstract
Recurrent laryngeal nerve (RLN) damage in infants leads to increased dysphagia and aspiration pneumonia. Recent work has shown that intraoral transport and swallow kinematics change following RLN lesion, suggesting potential changes in bolus formation prior to the swallow. In this study, we used geometric morphometrics to understand the effect of bolus shape on penetration and aspiration in infants with and without RLN lesion. We hypothesized (1) that geometric bolus properties are related to airway protection outcomes and (2) that in infants with RLN lesion, the relationship between geometric bolus properties and dysphagia is changed. In five infant pigs, dysphagia in 188 swallows was assessed using the Infant Mammalian Penetration–Aspiration Scale (IMPAS). Using images from high-speed VFSS, bolus shape, bolus area, and tongue outline were quantified digitally. Bolus shape was analyzed using elliptical Fourier analysis, and tongue outline using polynomial curve fitting. Despite large inter-individual differences, significant within individual effects of bolus shape and bolus area on airway protection exist. The relationship between penetration–aspiration score and both bolus area and shape changed post lesion. Tongue shape differed between pre- and post-lesion swallows, and between swallows with different IMPAS scores. Bolus shape and area affect airway protection outcomes. RLN lesion changes that relationship, indicating that proper bolus formation and control by the tongue require intact laryngeal sensation. The impact of RLN lesion on dysphagia is pervasive.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Damage to the recurrent laryngeal nerve (RLN) is a frequent complication of surgery to correct patent ductus arteriosus in premature infants [1, 2]. Iatrogenic RLN lesion is associated with increased incidence of dysphagia [2–4], leading to increased aspiration, with potentially dangerous complications such as aspiration pneumonia. Severity and prognosis are variable and difficult to predict [5, 6].
The RLN provides motor innervation to the intrinsic laryngeal muscles, and sensory innervation to the laryngeal mucosa below the vocal folds. Neither these muscles, nor these sensory fields, are directly involved in a safe swallow. However, recent work has indicated that airway protection deficits following RLN lesion are associated with changes in the timing and extent of tongue movements during intraoral transport and the swallow [7]. In addition, both anesthesia [8] and stimulation [9] of oral sensory pathways change swallow parameters and airway protection outcomes, highlighting the importance of sensory modulation of the swallow by structures throughout the oral, pharyngeal, and laryngeal complex. This suggests that the biomechanics of transport of the liquid bolus from the valleculae to the pharynx may be modified in infants with a recurrent laryngeal nerve lesion.
These biomechanics of transport are responsible for the bolus formation prior to propulsion into the esophagus. Changes in size and shape of the bolus resulting from RLN lesion may reveal important information about how bolus properties, airway protection, and recurrent laryngeal nerve lesion are interrelated.
Geometric morphometrics is a toolbox of mathematical and statistical techniques that allow complex two- and three-dimensional shapes to be analyzed quantitatively in a way that can be directly related to underlying variation in anatomy [10]. As bolus shape, tongue shape, and bolus area are all potentially relevant anatomical variables in understanding the relationship between bolus formation in the valleculae and airway protection, in this study we propose to use geometric morphometrics to address this question. The complex and changing shape of the tongue and soft palate, which determine much of the two dimensional bolus outline, are functionally relevant variables not reducible to linear metrics, or single-point-tracking-based kinematic approaches. Thus, although such approaches yield important insights into timing of the relative movements of the structures involved in the swallow [7], they do not tell us about the deformation of these structures, and therefore the formation of the bolus itself.
The aim of this study is to establish whether bolus formation in the valleculae prior to the swallow is predictive of airway protection outcomes in intact infants and infants with unilateral recurrent laryngeal nerve lesion. We use our validated infant pig model [8, 11, 12] in order to do controlled nerve injuries and collect amounts of data impossible in vulnerable infant clinical populations. Infant pigs are a good model for infant humans through similar size [13], similar anatomy (a fleshy, muscular tongue, muscular cheeks, and an intranarial larynx), and a similar mode of drinking (tongue-based suction rather than lapping) [14]. Furthermore, unlike rodent models, aspiration and penetration are characteristic features of dysphagia in infant pigs as they are in humans, so infant pigs make a good model of this particular pathophysiology. Interspecies comparisons with non-human primates suggest that many features of infant feeding are shared among mammals [15]. In so far as it is known, the peripheral innervation of the larynx is anatomically broadly similar in pigs and humans [13]. Thus, detailed, controlled, experimental study of pathophysiology of feeding in infant pigs can inform and guide clinical hypothesis development where such invasive experimental work is impossible. We tested two hypothesis:
-
1).
Variation in bolus shape, tongue shape, and bolus area is related to airway protection outcomes.
-
2).
Recurrent laryngeal nerve lesion leads to changes in bolus shape, tongue shape, and bolus area, and changes to their relationship to airway protection.
Materials and Methods
Animals
Five pigs aged between 3 and 14 days of age were trained to drink pig formula (Solustart Pig Milk Replacement, Land o’ Lakes, Arden Mills, MN) mixed with barium sulfate (E-Z Paque Barium sulfate, EZ EM Inc., NY) from a bottle in front of a fluoroscope (GE9400 C-Arm, 80 kV, 4MA) connected to a high-speed, adjustable frame rate digital camera (used at 100 frames per second, XC 1 M digital video camera, Xcitex, Cambridge, MA). The camera resolution was 1260 by 1080. The liquid formula used was 250 ml of milk powder mixed with 250 ml of barium sulfate and 1 l of water, which the pigs drank without difficulty. Radio opaque markers were implanted in the tongue. Seven days after arrival, unilateral recurrent laryngeal nerve lesion was performed surgically. Under isoflurane anesthesia (2–5%) using aseptic techniques, the right recurrent laryngeal nerve was identified anatomically from its entry into the larynx at the level of the cricothyroid muscle. The nerve was then ligated with suture in two places, crushed with microvascular hemoclips, and sectioned, with a 1–2 mm section of nerve removed. The ends were displaced to prevent re-innervation of the larynx. Lesion was confirmed by post-mortem dissection in all individuals. Individuals were recorded feeding on milk pre- and post-lesion, so that each individual could act as its own control. All protocols and procedures were approved by the NEOMED institutional animal care and use committee (IACUC protocol 13-011).
Swallows
Animals were filmed in lateral view drinking barium milk unrestrained in front of a fluoroscope recording at 100 fps. Swallows were assessed for airway safety using the Infant Mammalian Penetration–Aspiration Scale [16] (Table 1). A random sample of pre- and post-lesion swallows with IMPAS scores of 1, 2, and 7 was selected for this analysis, as previous work indicates that lesion–IMPAS interactions can be expected as one outcome of these experiments [7]. Not all IMPAS scores are present in all individuals owing to natural variation in the severity of response to lesion; in particular, one individual did not aspirate post lesion. Furthermore, silent aspiration is considerably rarer in unlesioned pigs than in lesioned pigs, although it does occur [12]. As a result, the design could not be perfectly balanced. A total of 188 swallows were used in this analysis.
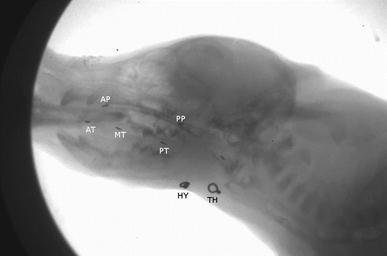
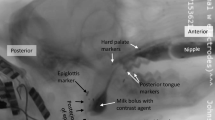
Bolus Outline
For each swallow selected for the analysis, the frame before the beginning of posterior movement of the epiglottis was selected for measurement of bolus properties. Boluses were outlined in ImageJ [17] using the free select tool on a touch screen tablet with a stylus (Surface Pro 2, Microsoft Corporation, Redwood, WA). A measuring scale was set using a ball with a 12.7-mm diameter attached to the pig. Milk in the pyriform recesses was excluded from the outlines, as the volume contained within the recesses is quite small relative to the valleculae, given their anatomical relationship to the laryngeal opening. The area outlined was then measured in mm2 (Fig. 1a). Although we could not automate this process, a blinded repeated measures trial of manual outline traces indicated that error due to outline tracing was less than variation between different boluses. This method of quantifying bolus shape has limitations due to movement of the pig’s head out of parasagittal position, unavoidable as the animals in this study fed unrestricted. Some caution is needed to avoid making overly specific interpretations of the results. However, techniques, such as 4D CT scans [18] to image boluses in 3D, which would avoid this problem, are only 10 fps, and do not yet have the temporal resolution of our system.
Tongue Outline
The tongue was outlined following a standard protocol. The base of the tongue (where the tongue meets the epiglottis) was identified on the image. A radio opaque marker had been placed in the middle of the tongue, at a histological location marked in pigs by the presence of a V-shaped keratinous pad. The surface of the tongue between these two points was digitized with the stylus and tablet in ImageJ, and exported as a series of X–Y coordinates (Fig. 1b).
Elliptical Fourier Analysis
Bolus outlines were analyzed using elliptical Fourier analysis [19], a type of geometric morphometrics designed for shape analysis of closed outlines. Elliptical Fourier analysis allows the quantification of complex shapes, and the exploration of how these shapes differ in a manner that can be related to differences in the configuration of muscular structures (Fig. 2). Closed outlines are represented as unique combinations of coefficients weighing different harmonic functions derived from a Fourier transformation of the curves. Outlines of boluses were extracted from digitized boluses using ChainCoder [20]. Fourier decomposition of the outlines were calculated using the Momocs package for R [21]. Once Fourier coefficients were calculated for each outline, a principal components analysis was performed on the coefficients, and the principal components scores were used for subsequent multivariate statistics [22]. Often, a very high number of Fourier coefficients (in this case, 32) are needed to represent each shape. Such large numbers of variables to represent each case become statistically redundant. Principle components analysis is a data reduction technique that uses the correlation between these coefficients to construct axes that capture the covarying changes in outline shape in the sample, in progressively smaller proportions. Thus, often, most of the variation in the sample can be analyzed using a small number of principal components, instead of the original high variable count representation of each sample [23].
Graphical representation of elliptical Fourier analysis. Any closed outline (a) can be approximated by the sum of a hierarchy of elliptical orbits of progressively higher rotation frequency (b). The fundamental orbit (the best fit ellipse to the original outline) sets the basic period of rotation, with the higher orbits rotating at a harmonic frequency of the original period. The more harmonic orbits are added (c) the better the fit to the original outline. The coefficients which define the ellipse drawn by each harmonic orbit uniquely represent each outline in a set of outlines
Polynomial Curve Fitting
Tongue outline traces were analyzed using polynomial curve fitting with a least squares goodness of fit criterion. Using a polynomial fit, curvature in a scatter of points, like that which represents tongue outline, can be modeled. Polynomial approximation was used in preference to geometric morphometrics as the muscular, deformable nature of the tongue makes it difficult to be certain that the anatomical regions outlined in each animal are clearly homologous. Thus, polynomials were used as quantitative estimates of the shape of the trace, without the strong inferences about the underlying morphology a geometric morphometric analysis would have. Various polynomial models were assessed by examination of residual plots of tongue outlines to polynomial curves for heteroscedasticity. A third order polynomial with a sine factor was selected based on equally distributed goodness of fit along the entire digitized tongue surface. Polynomial coefficients from the least squares best fit polynomial to each tongue outline were retained for further analysis. Polynomial curves were fitted in Systat 13 (Systat Software, Inc., San Jose, CA). The polynomial function had the following general form:
Relationship Between Nerve Lesion, Airway Protection, and Bolus Shape
We tested the relationship between nerve lesion, airway protection, and bolus shape using multivariate ANOVA. We used a complete model approach, with three fixed factors (individual, IMPAS score, treatment) and all four interaction terms. Inter-individual variation was very high, which is why individual was also included as fixed factor in the model. The dependent variables were the principal component scores of the first five principle components deriving from the analysis of bolus outline Fourier coefficients, which account for 97% of the variance in the sample. No single principal component after PC 5 accounted for more than 1% of the total variance in the sample. All statistical tests were conducted in R [24].
Relationship Between Nerve Lesion, Airway Protection, and Bolus Area
We tested the relationship between nerve lesion, airway protection, and bolus area using a univariate ANOVA. As above, we used a complete model with three fixed factors (individual, IMPAS score, treatment) and all four interaction terms. The dependent variable was bolus area measured in mm2.
Relationship Between Nerve Lesion, Airway Protection, and Tongue Shape
We tested the relationship between nerve lesion, airway protection, and tongue shape with univariate, multifactorial ANOVAs, with three fixed factors and interaction terms. We analyzed each coefficient of the polynomial (first order, second order, third order, constant, sine term) separately.
Correlation of Variables
We predict that tongue shape, bolus shape, and bolus area to be correlated as biological variables. In order to separate the effects of these correlations, we performed two multivariate regressions. The first was a multivariate multiple regression of the principal component scores of bolus shape on the first, second, and third order factors of the polynomials fit to the tongue outlines. The second was a multivariate regression of the principal components of bolus shape on bolus area. For each regression, we analyzed the residuals of bolus shape principal component scored using the multifactorial MANOVA with three fixed factors and four interactions. This method of analysis is a mathematical way of analyzing size independent, and tongue shape independent, bolus shape variation.
Results
Variation in Bolus Shape is Correlated with RLN Lesion, Airway Protection, and Individual Variation
Across all swallows in a feeding sequence, swallow safety decreased pre- to post-lesion in all animals (Table 2). Significant differences in bolus shape are found between individuals, nerve lesion treatment groups, and swallows with different airway protection outcomes (Table 3). Furthermore, the statistical interactions between these terms are significant, indicating that the relationship between bolus shape and airway protection outcome is different between control and lesion, and in different individuals. Thus, graphically, when plotting PC1, PC2, and PC3 (92.43% of the total variation in the sample), patterns of bolus shape differences are inconsistent among individuals (Fig. 3). Calculated average shapes of the bolus pre- and post-lesion in each individual show within individual differences in the tongue profile which are overshadowed by overall inter-individual differences (Fig. 4).
The Relationship Between Bolus Area and Airway Protection Changes Pre- and Post-RLN Lesion
Across all animals, bolus area is significantly smaller post-lesion that pre-lesion, and graphically this reduction in bolus area is most clearly visible in safe swallows (Fig. 5). Statistically, between-individual variation is highly significant, and thus the effect of treatment on the relationship between bolus area and aspiration is only statistically significant within individuals (Table 4). This is due in part to the variation in the distribution of IMPAS score among individuals. For example, one individual never showed any aspiration pre- or post-lesion, and this individual also consistently had small area boluses.
Boxplot of log of bolus area in control and lesion swallows with different IMPAS values. Boxes are median and interquartile range, whiskers are 95th percentiles, dots are outliers. See Table 4 for statistical significance
Differences Following RLN Lesion in Tongue Shape Reflect Both Airway Protection Outcomes and the Effect of RLN Lesion
In the analysis of tongue shape, one of the five individuals had to be removed owing to much higher variation and poor polynomial fit than the other four. There were significant differences in the tongue outlines between individuals, pre- and post-lesion, and between IMPAS scores, although the interaction of treatment and IMPAS was not significant in this case (Table 5). Both first and third order polynomial coefficients were lower in RLN lesion than in control pigs, with intercept, second order, and sine term coefficients being higher (Fig. 6).
Boxplot of the five parameters of the best fit polynomials to tongue outlines in control and lesion swallows with different IMPAS values. Boxes are median and interquartile range, whiskers are 95th percentiles, dots are outliers. See Table 5 for statistical significance
Bolus Area and Tongue Shape do not Account for all of the Relationship between Bolus shape, RLN Lesion, and Airway Protection
The effects of individual, IMPAS score, and RLN lesion on the residuals from the multivariate multiple regression of bolus shape principle component scores against tongue shape coefficients are all significant, as well as all the interactions (Table 6). This indicates that aspects of bolus shape distinct from the tongue curvature (which describes part of the bolus as traced in this study) are related to airway protection outcomes, and affected by RLN lesion.
The multivariate regression of bolus shape principle components on bolus area is highly significant (p < 0.001, F(5172) = 215.43). However, the effects of individual, RLN lesion, and IMPAS score on the variation in the residuals of bolus shape principle components from this regression are still significant (Table 7). Only the individual: treatment and individual: IMPAS score interactions are still significant though, indicating that the effect of treatment on IMPAS score may be primarily driven by bolus area and bolus area correlated shape difference.
Discussion
Variation in Bolus size and Shape is Correlated with Dysphagia and Failure of Airway Protection
For both lesioned and non-lesioned infants, boluses in the valleculae differ between normal and dysphagic swallows both in area and in shape. Thus, swallows in which aspiration occurs already have different properties from safe swallows before the swallow reflex proper has been triggered. As aspiration is much rarer in animals without lesion, the effect is less strong ([12]; Table 2). Although the bolus area measured here is a two-dimensional proxy for volume, previous work [25] has shown that the correlation between bolus area and bolus volume is strong. The relationship between bolus area and failure of airway protection is consistent with literature indicating that swallow volume is a key determinant in preventing aspiration and is often an indicator of mistimed triggering of the swallow [26, 27].
The clear effect of recurrent laryngeal nerve lesion on bolus area, bolus shape, and their relationship to airway protection outcomes adds to the body of knowledge indicating that RLN lesion affects the swallow in a more fundamental way than simply by preventing vocal fold closure [12]. The apparent reduction in the area of boluses associated with safe swallow outcomes in infants with lesion is particularly intriguing in this regard, as it suggests that RLN lesion may impact on the oro-pharyngeal system’s ability to handle large boluses safely. This suggests that controlled volume of milk delivery may potentially be a therapeutic avenue worth investigating for infants with RLN damage. Mechanically, controlling both rate and volume of milk delivery changes both frequency and volume of boluses in intact infants [11]. Future work on how these parameters also affects swallow safety outcomes in intact infants, and infants with RLN lesion, are warranted.
Physical properties of the bolus, specifically the rheology of the fluid, may be part of the explanation for the pattern observed here. Although there is no change in the rheology of the milk fed to animals pre- and post-lesion, fluid properties are well known to affect swallowing safety, and form the primary basis for treatment intervention [28]. Thus, some of these outcomes might vary with the rheological properties of the liquids being ingested.
The pressure dynamics within the oropharynx will also be important in determining the shape and movement of the bolus. These observed changes may relate to changes in the pressure differentials in the pharynx and oral cavity. Importantly, these changes in shape occur before the bolus enters the pharynx proper suggesting that changes in pharyngeal pressure are unlikely to be driving these differences. However, changes in the negative pressure gradient that drive the oral suction pump [29] may be important in bolus formation and control.
RLN Lesion may Impact the Relationship Between Tongue Movements and Timing of the Swallow
Tongue shape differs markedly between control and lesion boluses. The data collected in our analysis represented a snapshot from a kinematic process. Furthermore, this snapshot was timed to the swallow, as indicated by the movement of the epiglottis. Thus, the differences found may reflect absolute difference in tongue geometry between lesion and control animals, or they may reflect changes in timing between tongue movements and the pharyngeal swallow. It may be that, from the perspective of tongue kinematics, we were comparing different frames of the same film sequence between control and lesion swallows. In the future, we will carry out a more complete dynamic analysis to address this question.
Sensory Signals and Swallowing
This work adds to the understanding of the role of the bolus in the sensory motor control of infant swallowing. Various bolus properties modify swallow outcomes. The viscosity of the bolus affects kinematics of swallow, changing the duration of the various phases of the swallow and modifying airway protection outcomes [30]. Conversely, varying various parameters (such as rate of milk delivery [9]) has measurable effects on bolus volume at swallow initiation. Most relevant, lesion of the superior laryngeal nerve (SLN), which is also associated with a significant increase in aspiration [31], also results in changes in the volume of liquid in the valleculae at the point at which the swallow is initiated [26].
These results are consistent with our previous work on tongue kinematics [7], and point strongly to existence of sensory motor connections between the afferent signals coming up the recurrent laryngeal nerve to the nucleus tractus solitarius, and the efferent signals emanating from the hypoglossal motor nucleus. Extensive sensory motor connections exist between the oral cavity and the swallow reflex [9, 32]. The results here indicate that sensory motor connections are ubiquitous throughout the oro-pharyngeal–laryngeal system, although their neurological basis is still poorly understood [33, 34]. Further investigation of tongue kinematics, as well as neurological investigation of connections between the brainstem and the cortex in the control of oro-pharyngeal movements is needed to clarify the neurological substrate of these results.
Clinically, the similarities between pigs and humans in laryngeal innervation on the one hand, and infant feeding behavior on the other, suggest that the results of this investigation are likely to translate to human feeding behavior. Thus, videofluoroscopic assessment of patient swallowing in infants with severe dysphagia may benefit from examination of bolus shape properties. Furthermore, unlike work involving tracking implanted radiopaque markers, this study’s approach is broadly non-invasive, and could be adapted to human patient studies with relatively minor modifications.
Between-Individual Variation is High and Pervasive
Between-individual differences consistently account for large proportions of the variation in these data, so much so that without explicitly incorporating it statistically, effects of lesion and airway protection are masked. And yet, within individual there are consistent patterns. For example, the one individual that never aspirated pre- or post-lesion consistently had the least variable, and smallest in area, boluses. This reinforces that the variation seen in severity and prognosis for infants with RLN lesion cannot be attributed solely to variation in degree of insult, but also to underlying physiological differences between the individuals. In this regard, it is important to remember that infants are neurologically plastic, and undergoing significant sensory and motor remodeling of the central nervous system. Infant pigs have quite compressed post-natal development, reaching weaning age within 25 days post birth [35]. Maturation in coordination of respiration and swallowing occurs over a couple of days post birth [36]. It is therefore likely that the between-individual variation observed in these animals could be due to maturational differences occurring over a span of a day or two. A better understanding of the interaction between neural maturation and variability in feeding behavior is important.
Limitations of the Study
Firstly, the use of two-dimensional images to quantify differences in complex three-dimensional shapes introduces measurement error due to the projection of these three-dimensional shapes into the plane [37]. This error complicates the interpretation of shape differences, and reduces the strength of the signal. This is compounded by the difficulty of maintaining an unrestrained, vigorously feeding animal in a completely parasagittal plane relative to the camera. As a result of this limitation, our power to detect effects is reduced (accounting for the low F values of many of our factors). Furthermore, our ability to make strong statements as to what part of bolus shape changes is reduced, as some of the apparent shape change in our sample is attributable to planar projection of volumes and head rotation in the animals. However, the reconstruction in three dimensions of bolus is only achievable currently using X-ray tomography, and is impossible at 100 fps, a speed which captures the detailed kinematics of infant swallowing. Going forward, the use of X-ray Reconstruction of Moving Morphology (XROMM) [38] may allow some of these artifacts to be reduced. Furthermore, many of these limitations also apply to studies of human infant swallowing. While adult human subjects can be told to hold position, it may be difficult to maintain a strict parasagittal orientation for children or infants. The level of detail we obtained in this study is impossible to achieve in human infants. In particular, the number of swallows recorded and the camera speed (which requires higher intensity of X-ray technique) would be ethically impermissible in human infants.
A further limitation of using these two-dimensional images is that our metrics are all proxies for actual bolus properties (volume, three-dimensional shape, tongue kinematics). Thus, our results, though indicative of changes in function following RLN lesion, are limited in their insights into the biomechanics of the bolus. The use of a mechanical milk delivery system, and of three-dimensional reconstruction of tongue kinematics, may allow more direct estimation of bolus volume and tongue kinematics.
Conclusion
The shape of the bolus in the valleculae prior to the swallow differs between swallows without penetration or aspiration, and swallows in which airway protection fails. Furthermore, RLN lesion changes both bolus properties and the relationship between these and airway protection. Thus, this study adds yet another neurological mechanism by which the coordination of the swallow is modulated by sensory inputs from the entire oro-pharyngeal and laryngeal complex. Clinically, this study highlights that the swallow varies between infants, and that variable responses to laryngeal nerve damage reflect underlying variation in infant physiology. More investigation of the neural mechanisms of tongue control and bolus dynamics is needed to better understand the pathophysiology of infant dysphagia.
References
Benjamin JR, Smith PB, Cotten CM, Jaggers J, Goldstein RF, Malcolm WF. Long-term morbidities associated with vocal cord paralysis after surgical closure of a patent ductus arteriosus in extremely low birth weight infants. J Perinatol. 2010;30:408–13.
Pereira KR, Firpo C, Gasparin M, Teixeira AR, Dornelles S, Bacaltchuk T, et al. Evaluation of swallowing in infants with congenital heart defect. Int Arch Otorhinolaryngol. 2015;19:055–60.
Daya H, Hosni A, Bejar-Solar I, Evans JNG, Bailey CM. Pediatric vocal fold paralysis: a long-term retrospective study. Arch Otolaryngol Head Neck Surg. 2000;126:21.
Périé S, Laccourreye O, Bou-Malhab F, Brasnu D. Aspiration in unilateral recurrent laryngeal nerve paralysis after surgery. Am J Otolaryngol. 1998;19:18–23.
de Gaudemar I, Roudaire M, François M, Narcy P. Outcome of laryngeal paralysis in neonates: a long term retrospective study of 113 cases. Int J Pediatr Otorhinolaryngol. 1996;34:101–10.
Nichols BG, Jabbour J, Hehir DA, Ghanayem NS, Beste D, Martin T, et al. Recovery of vocal fold immobility following isolated patent ductus arteriosus ligation. Int J Pediatr Otorhinolaryngol. 2014;78:1316–9.
Gould FDH, Ohlemacher J, Lammers AR, Gross A, Ballester A, Fraley L, et al. Central nervous system integration of sensorimotor signals in oral and pharyngeal structures: oropharyngeal kinematics response to recurrent laryngeal nerve lesion. J Appl Physiol. 2016;120:495–502.
Holman SD, Campbell-Malone R, Ding P, Gierbolini-Norat EM, Lukasik SL, Waranch DR, et al. Swallowing kinematics and airway protection after palatal local anesthesia in infant pigs: swallowing after palatal anesthesia. Laryngoscope. 2014;124:436–45.
German RZ, Crompton AW, Owerkowicz T, Thexton AJ. Volume and rate of milk delivery as determinants of swallowing in an infant model animal (Sus scrofa). Dysphagia. 2004;19:147–54.
Bookstein FL. A brief history of the morphometric synthesis. In: Marcus LF, editor. Advances in morphometrics. Cambridge: University Press; 1993.
German RZ, Crompton AW, Hertweck DW, Thexton AJ. Determinants of rhythm and rate in suckling. J Exp Zool. 1997;278:1–8.
Gould FDH, Lammers AR, Ohlemacher J, Ballester A, Fraley L, Gross A, et al. The physiologic impact of unilateral recurrent laryngeal nerve (RLN) lesion on infant oropharyngeal and esophageal performance. Dysphagia. 2015;30:714–22.
German RZ, Crompton AW, Thexton AJ. The role of animal models in understanding feeding behavior in infants. Int J Orofacial Myology. 2004;30:20–30.
Thexton AJ, Crompton AW, German RZ. Transition from suckling to drinking at weaning: a kinematic and electromyographic study in miniature pigs. J Exp Zool. 1998;280:327–43.
German RZ, Crompton AW, Levitch LC, Thexton AJ. The mechanism of suckling in two species of infant mammal: miniature pigs and long-tailed macaques. J Exp Zool. 1992;261:322–30.
Holman SD, Campbell-Malone R, Ding P, Gierbolini-Norat EM, Griffioen AM, Inokuchi H, et al. Development, reliability, and validation of an infant mammalian penetration–aspiration scale. Dysphagia. 2013;28:178–87.
Rasband WS. ImageJ. Bethesda: NIH; 1997. http://imagej.nih.gov/ij/.
Okada T, Aoyagi Y, Inamoto Y, Saitoh E, Kagaya H, Shibata S, et al. Dynamic change in hyoid muscle length associated with trajectory of hyoid bone during swallowing: analysis using 320-row area detector computed tomography. J Appl Physiol. 2013;115:1138–45.
Kuhl FP, Giardina CR. Elliptic Fourier features of a closed contour. Comput Gr Image Process. 1982;18:236–58.
Iwata H. SHAPE: a computer program package for quantitative evaluation of biological shapes based on elliptic Fourier descriptors. J Hered. 2002;93:384–5.
Bonhomme V, Picq S, Gaucherel C, Claude J. Momocs: outline analysis using R. J Stat Softw. 2014;56:1–24.
Ferson S, Rohlf FJ, Koehn RK. Measuring shape variation of two-dimensional outlines. Syst Biol. 1985;34:59–68.
Zelditch ML, Swiderski DL, Sheets HD. Geometric morphometrics for biologists: a primer. Cambridge: Academic Press; 2012.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2015.
Ding P, Fung GSK, Lin M, Holman SD, German RZ. The effect of bilateral superior laryngeal nerve lesion on swallowing: a novel method to quantitate aspirated volume and pharyngeal threshold in videofluoroscopy. Dysphagia. 2014;30:47–56.
Ding P, Campbell-Malone R, Holman SD, Lukasik SL, Thexton AJ, German RZ. The effect of unilateral superior laryngeal nerve lesion on swallowing threshold volume. Laryngoscope. 2013;123:1942–7.
Belo LR, Gomes NAC, Coriolano MGWS, de Souza ES, Moura DAA, Asano AG, et al. The relationship between limit of dysphagia and average volume per swallow in patients with Parkinson’s disease. Dysphagia. 2014;29:419–24.
Zargaraan A, Rastmanesh R, Fadavi G, Zayeri F, Mohammadifar MA. Rheological aspects of dysphagia-oriented food products: a mini review. Food Sci Hum Wellness. 2013;2:173–8.
Thexton A, Crompton A, Owerkowicz T, German R. Correlation between intraoral pressures and tongue movements in the suckling pig. Arch Oral Biol. 2004;49:567–75.
Inamoto Y, Saitoh E, Okada S, Kagaya H, Shibata S, Ota K, et al. The effect of bolus viscosity on laryngeal closure in swallowing: kinematic analysis using 320-row area detector CT. Dysphagia. 2013;28:33–42.
Ding P, Campbell-Malone R, Holman SD, Lukasik SL, Fukuhara T, Gierbolini-Norat EM, et al. Unilateral superior laryngeal nerve lesion in an animal model of dysphagia and its effect on sucking and swallowing. Dysphagia. 2013;28:404–12.
Holman SD, Waranch DR, Campbell-Malone R, Ding P, Gierbolini-Norat EM, Lukasik SL, et al. Sucking and swallowing rates after palatal anesthesia: an electromyographic study in infant pigs. J Neurophysiol. 2013;110:387–96.
Michou E, Hamdy S. Cortical input in control of swallowing. Curr Opin Otolaryngol Head Neck Surg. 2009;17:166–71.
Leopold NA, Daniels SK. Supranuclear control of swallowing. Dysphagia. 2010;25:250–7.
Herring SW. Ontogeny of bone strain: the zygomatic arch in pigs. J Exp Biol. 2005;208:4509–21.
German RZ, Crompton AW, McCluskey C, Thexton AJ. Coordination between respiration and deglutition in a preterm infant mammal, Sus scrofa. Arch Oral Biol. 1996;41:619–22.
De Groote I, Aiello LC. Letter to the editor: response to Deane and Kremer’s comment: 3D, or not to 3D. Am J Phys Anthropol. 2011;144:498–9.
Brainerd EL, Baier DB, Gatesy SM, Hedrick TL, Metzger KA, Gilbert SL, et al. X-ray reconstruction of moving morphology (XROMM): precision, accuracy and applications in comparative biomechanics research. J Exp Zoo Part A Ecol Genet Physiol. 2010;313A:262–79.
Acknowledgements
The authors would like to thank the staff and the NEOMED comparative medicine unit, as well as Jackie Kulish, Katie DeLozier, and Tim Ohlemacher for their assistance in data collection.
Funding
This work was funded by NIH Grant R01 009980 to Rebecca German.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interests
None of the authors have any conflicts of interests to report.
Rights and permissions
About this article
Cite this article
Gould, F.D.H., Yglesias, B., Ohlemacher, J. et al. Pre-pharyngeal Swallow Effects of Recurrent Laryngeal Nerve Lesion on Bolus Shape and Airway Protection in an Infant Pig Model. Dysphagia 32, 362–373 (2017). https://doi.org/10.1007/s00455-016-9762-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-016-9762-2