Abstract
Postswallow residue is widely considered to be a sign of swallowing impairment and is assumed to pose risk for aspiration on subsequent swallows. We undertook a preliminary retrospective study to investigate the link between postswallow residue and penetration–aspiration on the immediately occurring subsequent clearing swallow (i.e., without introduction of a new bolus). Videofluoroscopy clips for 156 thin-liquid single bolus swallows by patients with neurogenic dysphagia were selected for study because they displayed multiple swallows per bolus. Residue for each subswallow (n = 407) was analyzed using the Normalized Residue Ratio Scale for the valleculae (NRRSv) and piriform sinuses. The association between residue presence at the end of a swallow and penetration–aspiration on the next swallow was examined. Postswallow residue in one or both pharyngeal spaces was significantly associated with impaired swallowing safety on the subsequent clearing swallow for the same bolus. However, when analyzed separately by residue location, only vallecular residue was significantly associated with impaired swallowing safety on the next clearing swallow. The distribution of NRRSv scores by swallowing safety demonstrated an NRRSv cut-point of 0.09, above which there was a 2.07 times greater relative risk of penetration–aspiration. Postswallow vallecular residue, measured using the NRRS, is significantly associated with penetration–aspiration on subsequent clearing swallows. A clinically meaningful cut-point of 0.09 on the NRRSv scale demarcates this risk. Further research with different bolus consistencies is needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The videofluoroscopic swallowing study (VFSS) is considered the optimal technique for assessing dysphagia [1] as it allows direct and dynamic visualization of swallowing function. One of the most important parameters assessed by the VFSS is airway protection, including the evaluation of the potential for (and cause of) penetration and/or aspiration. A second major feature identified using VFSS is residue, which occurs when material remains in the pharynx after the completion of a swallow and is related to swallowing inefficiency [2]. Residue has been clinically accepted as posing a risk for postswallow aspiration [3].
Despite the widely accepted clinical assumption that residue results in increased risk of aspiration, only a few studies have explored this relationship. In an early descriptive study of dysphagia following brainstem stroke, Horner et al. [4] reported that 17/23 patients had pharyngeal residue. Of these, a highly significant proportion (15/17) was found to aspirate. However, no details were provided regarding the location of the residue or the measurement methods used to rate residue and aspiration severity. Similar results were reported in a second study by Perlman et al. [5], who explored the relationship between vallecular residue and several physiological swallowing events. Of all the parameters measured, binary ratings for vallecular residue presence were found to have one of the highest co-occurrence rates with aspiration (80 %). In a third study, Han et al. [6] used logistic regression to explore the association between aspiration and 18 oral and pharyngeal phase parameters in 103 stroke patients who swallowed 2 ml of barium. A 5-grade ordinal scale was used to capture depth of aspiration and 4-grade ordinal scales were used to capture residue severity in the valleculae and piriform sinuses, based on a visual perceptual estimate of the percent of the width of the available space that was observed to be filled with residue. Significant associations with aspiration were found for vallecular residue (odds ratio [OR] = 2.75; 95 % confidence interval [CI] = 1.74–4.33) and piriform sinus residue (OR = 3.20; 95 % CI = 2.06–4.98), though cut-points for impairment were not clearly defined.
Although these prior studies claim to have explored the relationship between postswallow residue and aspiration, it can also be argued that they demonstrated, quite simply, that patients who have residue also tend to be patients who aspirate. In particular, they fail to provide details about the time point within the swallow sequence when aspiration occurred. Such information is critical for understanding the aspiration risk associated with residue presence. In order to properly appreciate the clinical significance of postswallow residue for swallowing safety, clarity regarding the relative timing of observed residue and penetration–aspiration is needed to be known.
One study by Eisenhuber et al. [7] set out to test the relationship between pharyngeal residue and “postdeglutitive overflow aspiration” (postswallow residue). Of 386 patients referred for VFSS, 108 had mild, moderate, or severe residue (scores of 1, 2, or 3) as captured by their 4-point ordinal scale for residue retention. These authors provided clear information regarding the time-point in the swallowing sequence at which residue ratings were made (i.e., after an initial swallow of contrast material). However, the test stimuli in the study differed, depending on whether at the beginning of the VFSS the patient was already considered likely to aspirate. For suspected aspirators, 3 ml of thin-liquid nonionic iodinated contrast was administered. For all other patients, the test stimulus was a 15-ml bolus of barium suspension (250 % g/ml). The number of swallows observed ranged between 1 and 8, and bolus volumes varied between 3 and 30 ml. Any penetration of material into the supraglottic region or below was categorized as indicating impaired swallowing safety, and the time points of these events (before, during, or after the swallow) were recorded. Of the 108 patients with postswallow residue, 70 also had postswallow aspiration. Furthermore, the severity of the pharyngeal residue was found to be predictive of postswallow aspiration (OR = 8.46; 95 % CI = 3.73–19.20). While this study more clearly demonstrates a link between postswallow residue and aspiration, several limitations must also be called to attention. First, it remains unclear whether the reported association between residue and aspiration reflects overall co-occurrence rates or a more direct link, i.e., postswallow penetration–aspiration events on swallows that followed those for which residue had been recorded. Second, although a clear definition of the time point at which residue measurements should be made was provided, corresponding operational definitions for the possible timing of penetration–aspiration (i.e., before, during, or after the swallow) were not provided. Third, the a priori decision to administer different stimuli to those patients already suspected to be at risk (or not at risk) of aspiration is problematic. The nonionic iodinated contrast material administered to suspected aspirators was almost certainly of lower viscosity and density than the barium suspension administered to nonaspirators and, therefore, could be more likely to have been aspirated. Conversely, the barium stimulus was arguably more likely to have left postswallow residue given that a known and intended property of such high-density (double-contrast) barium preparations is to coat mucosa. Thus, the opportunity to develop residue, to aspirate, and to demonstrate a relationship between residue and aspiration was not uniform across patients.
Finally, as summarized in Pearson et al. [8], ordinal scales such as those used by Eisenhuber et al. have been shown to have limited precision and poor reliability.
In the present study, our aim was to overcome some of the limitations in the existing literature and to explore the relationship between postswallow residue in the valleculae and/or piriform sinuses and penetration–aspiration on the immediately occurring subsequent clearing swallow. Figure 1 provides a schematic illustration of our research question. Our study is a preliminary exploration of the association between residue and aspiration in a retrospective sample of patients with neurogenic dysphagia who presented with multiple swallows per bolus, and focused specifically on clearing swallows. Residue present in the pharynx at the beginning of each of these clearing swallows (henceforth known as preswallow residue) was present after the immediately preceding swallow of the same bolus and was the only material available for possible aspiration. No new bolus material was added, and situations of piecemeal deglutition involving oral division of a bolus into two or more portions [9] were excluded. Our hypothesis was that aspiration would be significantly related to the presence of preswallow residue, measured using a recently introduced anatomically referenced scale for capturing residue severity, the Normalized Residue Ratio Scale (NRRS) [8].
Illustration of a hypothetical three-swallow sequence of a single bolus (A). The relationship of interest is between “preswallow” residue (i.e., NRRS A1) and swallow safety on the immediately occurring subsequent swallow of the same bolus (i.e., PAS A2). PAS penetration–aspiration score; NRRS normalized residue ratio scale
Methods
Materials
Data for this study were extracted from the VF_VAR dataset, a clinical archive of 136 videofluoroscopies that was collected to document variability and change in swallowing across repeated VFSS. The inclusion criterion for the database was that the patients had undergone more than one VFSS during the 4-year period (2007–2010) over which the database was built. Recordings in the database come from 55 subacute patients with neurogenic dysphagia. While the majority of the patients were referred from stroke, brain injury, and geriatric units, exact etiological details for these patients were not available in this retrospective dataset. All studies in the database were conducted using a Toshiba Ultimax (Toshiba America Medical Systems, Inc., Tustin, CA) fluoroscope in lateral view at 30 pulses per second, and were captured and recorded at 30 frames per second. Standardized 22 % w/v ultrathin barium [10] was used for all thin-liquid swallowing tasks. The exact volume of the boluses administered was regrettably not documented, but data extraction for this study was restricted to clips of single sip or teaspoon amounts (continuous cup and straw drinking were excluded).
For each of the 367 thin-liquid-bolus videoclips available in the dataset, we recorded the number of subswallows that occurred. A bolus videoclip was defined as the swallowing behavior that was captured on fluoroscopy for a single bolus (i.e., the swallowing sequence elicited in response to a single bolus). A subswallow was defined as an individual swallow within the swallow sequence elicited in response to a single bolus. Of the total of 618 available subswallows, 211 clips were excluded from further consideration because the entire bolus was swallowed in a single swallow without requiring any clearing swallows. The remaining 156 bolus clips contained a total of 407 subswallows. Of these subswallows, 156 were initial subswallows resulting in postswallow residue and 251 were clearing swallows in which preswallow residue was present. This set could be further subdivided into 154 subclips of secondary swallows, 63 subclips of tertiary swallows, and 34 subclips that represented a fourth (or higher-ordered) clearing swallow.
Swallow Rating
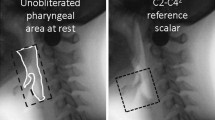
The available data for swallows in the VF_VAR dataset were assigned an alphanumeric code and subjected to a variety of measurements, including the Penetration–Aspiration Scale [11] and the NRRS [8]. Raters were blinded to participant identity and to results of other rating values. The Penetration–Aspiration Scale and NRRS ratings were obtained for each subswallow by rating bolus-level clips arranged in random order. The Penetration–Aspiration Scale scores and the NRRS scores for the valleculae (NRRSv) and the piriform sinuses (NRRSp) were used for the current analysis. NRRS measures were calculated using a single video frame for each subswallow, capturing the hyoid at its lowest (most inferior) position, immediately after epiglottic return to the vertical position, and after postswallow pharyngeal relaxation [8]. As the hyoid descends from peak position, the pharynx reconfigures (widens and lowers) from its contracted (pressure generating) state to a resting state. We consider pharyngeal relaxation to be the moment when this process is complete.
Reliability Rating
All VFSS ratings were completed by the first author. For intrarater reliability measures, 20 % of these ratings were selected at random and repeated. Additionally, 20 % of the ratings were scored by a second rater, a speech-language pathologist with experience in physiological measurement of deglutition, to determine interrater reliability. Reliability measures (two-way mixed intraclass coefficients for consistency, or ICCs) were calculated separately for the NRRSv, NRRSp, and Penetration–Aspiration Scale scores and appear in Table 1. We acknowledge that some of the ICCs for the NRRS scores fall within the “fair-to-good” range of 0.40–0.75 [12]. However, it should be noted that our reliability procedures did not include specification of the frame upon which NRRS measures should be taken. Thus, some of the variation observed within and between raters for NRRS scores may be attributable to differences in frame selection, particularly given difficulty with identifying the end of hyoid movement after a swallow [13]. Previous work [8] has shown that when the frame for measurement is controlled (i.e., chosen by the experimenters), inter- and intrarater reliability ICC scores for NRRS components range between 0.97 and 1.00.
Cut-Points for Impairment
In order to identify in our dataset the subswallow clips in which residue of concern was present, it was necessary to establish a binary cut-point for residue presence/absence. This was done at the level of the overall VF_VAR dataset, using all available thin-liquid subswallow clips (n = 618). Swallows that were the final swallow in a sequence (including single swallows) were deemed “terminal swallows.” Swallows that were followed by a subsequent clearing swallow were deemed “nonterminal swallows.” Clinically significant residue was operationally defined as residue that led to a subsequent clearing swallow (i.e., residue associated with nonterminal swallows). Table 2 provides descriptive statistics for NRRSv and NRRSp scores for nonterminal versus terminal swallows in the VF_VAR dataset. Based on the upper 95 % confidence interval boundaries for residue present at the end of terminal swallows, an NRRS cut-point ≥0.06 was determined to indicate clinically significant residue.
Similarly, an operationally defined binary cut-point for penetration–aspiration of concern was set at a Penetration–Aspiration Scale score of ≥3 and hereafter referred to as an “unsafe” swallow. Penetration–Aspiration Scale scores of 1 (no penetration or aspiration) and 2 (high transient penetration) were considered to be functional [14, 15] and are hereafter referred to as “safe.”
Data Analysis
Descriptive statistics were calculated for NRRSv and NRRSp scores according to swallow number (i.e., position) within the swallow sequence. The primary comparison of interest for this study was the two-by-two relationship between preswallow residue of concern (i.e., residue present at the beginning of a swallow as the result of an inefficient previous swallow of the same bolus) and impaired swallow safety (penetration–aspiration) on the subsequent swallow (Fig. 1). This relationship was first explored based on the intersection of residue in either the valleculae or piriform sinuses (i.e., observed anywhere in the pharynx), and then separately for the two pharyngeal spaces of interest. All comparisons were conducted using two-tailed Pearson’s χ2 statistics, with an α criterion for significance set at p ≤ 0.05. All statistical analyses were conducted using IBM SPSS Statistics version 20.
Results
Table 3 gives the overall distribution of NRRSv and NRRSp scores according to swallow position in the sequence for the entire VF_VAR dataset.
Figure 2 illustrates the relationship between preswallow residue in either one or both pharyngeal spaces and swallowing safety on the immediately occurring subsequent clearing swallow. A significantly greater proportion (43.5 %) of swallows displaying preswallow residue of concern were found to be unsafe compared to the proportion (29.1 %) seen in swallows without preswallow residue of concern (χ2 = 5.091, df = 1, p = 0.024). However, when analyzed separately by residue location, only preswallow residue in the valleculae demonstrated a significant relationship with subsequent swallow safety (χ2 = 15.029, df = 1, p = 0.000). As shown in Fig. 3, a significantly larger proportion of swallows with preswallow vallecular residue of concern were unsafe (53.0 %) compared to swallows without preswallow vallecular residue of concern (26.3 %).
The number of swallows with preswallow residue in one or both pharyngeal spaces by swallow safety (χ2 = 5.091, df = 1, p = 0.024). Clinically significant residue was determined by NRRS ≥0.06. An unsafe swallow was determined by penetration–aspiration scale score of 3 or higher. NRRS normalized residue ratio scale
The number of swallows with preswallow vallecular residue by swallow safety (χ2 = 15.029, df = 1, p = 0.000). Clinically significant residue was determined by NRRS ≥0.06. An unsafe swallow was determined by penetration–aspiration scale score of 3 or higher. NRRSv normalized residue ratio scale for vallecular residue
Interestingly, for piriform sinus residue, no significant relationship with unsafe swallows was found. The proportion of unsafe swallows associated with preswallow piriform sinus residue of concern (28/75 or 37.3 %), was not significantly different from the proportion of unsafe swallows with no preswallow piriform sinus residue of concern (52/157 or 33.1 %).
Given the finding of a significant relationship between preswallow vallecular residue and unsafe swallowing on the subsequent swallow, we conducted post hoc analyses to determine a cut-point on the NRRSv that distinguishes safe from unsafe swallows. Figure 4 demonstrates the distribution of NRRSv scores by swallow safety status (mean values with 95 % CI error bars). A conservative NRRSv cut-point was set at the lower 95 % CI boundary (i.e., NRRSv ≥0.09). This cut-point demarcates a 2.07 times greater relative risk of penetration–aspiration above this value (95 % CI = 1.42–2.88).
Discussion
The presence of residue after the completion of a swallow is a presumed risk for aspiration; however, previous studies have failed to sufficiently control timing relationships and/or use precise measurement techniques to adequately study this important clinical phenomenon. In this study, we chose a sample of patients who performed multiple swallows of a single thin-liquid bolus. For each subswallow, we rated penetration–aspiration status and the amount of residue remaining at the end of each subswallow. This allowed us to focus on the relationship between preswallow residue (residue apparent from the previous swallow) and swallowing safety of the immediately occurring subsequent swallow.
Using this paradigm, we were able to demonstrate a significant relationship between preswallow residue in both of the pharyngeal spaces and swallowing safety (Fig. 2) and when vallecular residue was analyzed independent of piriform sinus residue (Fig. 3). When vallecular residue exceeded a cut-point of a NRRSv value of 0.09, there was a heightened risk of penetration–aspiration on the next swallow (Fig. 4).
Interestingly, a significant independent relationship between preswallow piriform sinus residue and swallowing safety was not found. This finding was unexpected given the proximity of the piriform sinuses to the laryngeal vestibule. It is possible that the use of multiple swallows is a functional strategy for dealing with piriform sinus residue given the proximity of the piriform sinuses to the upper esophageal sphincter, but that this strategy is not effective for safely dealing with vallecular residue. Support for this explanation can be garnered from the data in Table 3. Inspection of mean NRRS scores across successive swallows reveals gradually declining piriform sinus residue; however, vallecular residue appears to be resistant to change across multiple swallows. This may, in part, explain the different results seen in our analysis of penetration–aspiration risk by residue location. Another explanation for the lack of a clear relationship between piriform sinus residue and subsequent penetration–aspiration would be that patients who aspirate in the presence of preswallow piriform sinus residue may aspirate for reasons other than this residue, thereby weakening the causative connection between these phenomena.
Based on the distribution of NRRSv scores seen in our analysis, we have proposed a critical cut-point for vallecular residue at NRRSv ≥0.09 and have shown that the relative risk of impaired swallowing safety doubled above this value. The establishment of a clinically meaningful threshold above which residue should be considered an impairment is an important contribution given that residue has been observed in healthy controls [16] and in up to 20 % of elderly nondysphagic individuals [17]. Our data suggest that when vallecular residue is present up to a threshold of NRRSv = 0.09, there should be no need for clinical concern. However, such an interpretation requires validation with other textures and in the context of a new bolus being introduced when there is already preswallow residue from a prior swallow.
There are several limitations to acknowledge for this study. In this retrospective analysis, we were limited to single sips or teaspoon amounts of a 22 % w/v ultra-thin liquid barium. We caution against extending these findings to continuous drinking, other textures, or other barium densities. Furthermore, our goal of investigating preswallow residue necessitated that our analysis be limited to cases in which multiple swallows were used to clear a single bolus. Presumably, patients who do not elicit multiple swallows in response to postswallow residue are also at risk for penetration–aspiration. A further limitation of our retrospective data is that we did not have access to whether swallows were spontaneously initiated or cued by the clinician during the exam. We acknowledge the limitation that radiation exposure considerations in videofluoroscopy cannot allow extended monitoring of residue post swallow and its risk for delayed postswallow aspiration. In addition to exploring the consequences of residue for swallowing safety with additional textures, known volume manipulations, and barium concentrations, future studies might employ both videofluoroscopy and endoscopy to enable extended viewing of the risks associated with postswallow residue in patients who do not spontaneously perform clearing swallows.
It is notable that the standard deviations observed for the NRRSv and NRRSp measures in this study are quite large, relative to the observed mean values, particularly for terminal swallows (both vallecular and piriform), as shown in Table 2, and for the NRRSp measure, as shown by swallow number within the sequence in Table 3. Closer post hoc inspection of the distribution of the data showed that the data distributions were non-normal and heavily skewed by the presence of near-zero values (very small amounts of residue). This may reflect the scale resolution of the NRRS, but it also very clearly speaks to the likelihood that there are clinically relevant cut factors within the distribution that dissociate risk from typically tolerated amounts of residue. Given that the analysis in the present study does not involve an ANOVA-type analysis for which there are assumptions regarding the distribution of the residuals, this is a significant concern for the current analysis. For future studies, if comparisons of residue severity are going to be made between groups of patients or between pre- and post-treatment measures, then assumptions regarding the distribution of residuals inherent to selected statistical tests will need to be carefully investigated.
Conclusion
In conclusion, we have shown that preswallow vallecular residue, but not piriform sinus residue, measured with an anatomically referenced and normalized ratio scale, is significantly associated with impaired swallowing safety on the subsequent clearing swallow in a sample of patients who recruit multiple swallows to clear thin-liquid boluses.
References
Rosenbek JC, Roecker EB, Wood JL, Robbins J. Thermal application reduces the duration of stage transition in dysphagia after stroke. Dysphagia. 1996;11:225–33.
Logemann JA. Evaluation and treatment of swallowing disorders. 2nd ed. Austin, TX: Pro-Ed; 1998.
Dodds WJ, Logemann JA, Stewart ET. Radiologic assessment of abnormal oral and pharyngeal phases of swallowing. AJR Am J Roentgenol. 1990;154:965–74.
Horner J, Buoyer FG, Alberts MJ, Helms MJ. Dysphagia following brain-stem stroke. Clinical correlates and outcome. Arch Neurol. 1991;48:1170–3.
Perlman AL, Grayhack JP, Booth BM. The relationship of vallecular residue to oral involvement, reduced hyoid elevation, and epiglottic function. J Speech Hear Res. 1992;35:734–41.
Han TR, Paik N, Park JW. Quantifying swallowing function after stroke: a functional dysphagia scale based on videofluoroscopic studies. Arch Phys Med Rehabil. 2001;82:677–82.
Eisenhuber E, Schima W, Schober E, Pokieser P, Stadler A, Scharitzer M, et al. Videofluoroscopic assessment of patients with dysphagia: pharyngeal retention is a predictive factor for aspiration. AJR Am J Roentgenol. 2002;178:393–8.
Pearson WG Jr, Molfenter SM, Smith Z, Steele CM. Image-based measurement of post-swallow residue: the normalized residue ratio scale. Dysphagia. 2013. doi:10.1007/s00455-012-9426-9.
Ertekin C, Aydoğdu İ, Yüceyar N. Piecemeal deglutition and dysphagia limit in normal subjects and in patients with swallowing disorders. J Neurol Neurosurg Psychiatry. 1996;61:491–6.
Fink TA, Ross JB. Are we testing a true thin liquid? Dysphagia. 2009;24:285–9.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration–aspiration scale. Dysphagia. 1996;11:93–8.
Fleiss JL. The design and analysis of clinical experiments. New York: Wiley; 1986.
Ishida R, Palmer JB, Hiiemae KM. Hyoid motion during swallowing: factors affecting forward and upward displacement. Dysphagia. 2002;17:262–72.
Allen JE, White CJ, Leonard RJ, Belafsky PC. Prevalence of penetration and aspiration on videofluoroscopy in normal individuals without dysphagia. Dysphagia. 2010;25:347–8.
Daggett A, Logemann J, Rademaker A, Pauloski B. Laryngeal penetration during deglutition in normal subjects of various ages. Dysphagia. 2006;21:270–4.
Omari TI, Dejaeger E, Van Beckevoort D, Goeleven A, De Cock P, Hoffman I, et al. A novel method for the nonradiological assessment of ineffective swallowing. Am J Gastroenterol. 2011;106:1796–802.
Ekberg O, Feinberg MJ. Altered swallowing function in elderly patients without dysphagia: Radiologic findings in 56 cases. AJR Am J Roentgenol. 1991;156:1181–4.
Acknowledgments
SMM has received funding for her doctoral studies from the Natural Sciences and Engineering Research Council (Canada) Create CARE program, the Ontario Student Opportunity Trust Fund, and the Ontario Graduate Studies scholarship program. CMS holds a New Investigator award from the Canadian Institutes of Health Research. The authors thank Becky Cliffe Polacco, Sarah Hori, Chelsea Leigh, and Clemence Tsang for assistance with data collection and analysis, and they acknowledge the support of Toronto Rehabilitation Institute, which receives funding under the Provincial Rehabilitation Research Program from the Ministry of Health and Long-term Care in Ontario. The views expressed do not necessarily reflect those of the ministry. This work was presented in part at the 2nd European Society for Swallowing Disorders Congress on October 26, 2012 in Barcelona, Spain.
Conflict of interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Molfenter, S.M., Steele, C.M. The Relationship Between Residue and Aspiration on the Subsequent Swallow: An Application of the Normalized Residue Ratio Scale. Dysphagia 28, 494–500 (2013). https://doi.org/10.1007/s00455-013-9459-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-013-9459-8