Abstract
In oral cancer treatment, function loss such as speech and swallowing deterioration can be severe, mostly due to reduced lingual mobility. Until now, there is no standardized measurement tool for tongue mobility and pre-operative prediction of function loss is based on expert opinion instead of evidence based insight. The purpose of this study was to assess the reliability of a triple-camera setup for the measurement of tongue range of motion (ROM) in healthy adults and its feasibility in patients with partial glossectomy. A triple-camera setup was used, and 3D coordinates of the tongue in five standardized tongue positions were achieved in 15 healthy volunteers. Maximum distances between the tip of the tongue and the maxillary midline were calculated. Each participant was recorded twice, and each movie was analysed three times by two separate raters. Intrarater, interrater and test–retest reliability were the main outcome measures. Secondly, feasibility of the method was tested in ten patients treated for oral tongue carcinoma. Intrarater, interrater and test–retest reliability all showed high correlation coefficients of >0.9 in both study groups. All healthy subjects showed perfect symmetrical tongue ROM. In patients, significant differences in lateral tongue movements were found, due to restricted tongue mobility after surgery. This triple-camera setup is a reliable measurement tool to assess three-dimensional information of tongue ROM. It constitutes an accurate tool for objective grading of reduced tongue mobility after partial glossectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oral cancer is the sixth most common cancer worldwide and the global incidence is around 275,000 per year [1]. In the Netherlands, 1056 patients were diagnosed with oral cancer in 2012 with a five-year cancer specific survival (adjusted for age related death; period 1989–2010) of 59 % [2].
Oral tongue carcinoma accounts for one-third of all oral carcinomas and most frequently arises at the lateral border of the tongue. Surgical resection is the preferred treatment for stage T1–T3 lesions, whereas larger lesions will be treated with chemoradiation if functionally unresectable [3]. Depending on the stage of the disease, surgical removal may have serious impact on the mobility of the tongue. Reduction of this mobility has been proven to be one of the main causes of impaired function as speech and swallowing deteriorate and problems with oral food transport [4–7]. Furthermore, rehabilitation (e.g. logopedic training) is predominantly based on the improvement of the lingual mobility to regain effective oral function [8]. Although lingual movement and its range of motion (ROM) are of great importance, there is no standardized and reproducible measuring system. As a result pre-operative prediction of reduced mobility and function loss is still matter of expert opinion and not based on scientific evidence [9]. If, however, we would be able to grade the reduced mobility and function loss, we would be able to (a) assess each individual patient on functional inoperability; (b) inform the patient better on the expected function loss and (c) adjust rehabilitation therapy to the specific needs of the patient to improve swallowing and speech function.
The constant problem in the assessment of tongue mobility is the fact that the tongue is concealed in the oral cavity and therefore hard to follow during movements. Different methods have been tried to capture tongue movements during action. Cine MRI, video fluoroscopy, and ultrasound are used methods, but all have their limitations: poor temporal resolution, exposure to radiation and velocity measurement with little information about the actual ROM of the tongue, respectively [10–12]. For static measurements of tongue range of motion a regular ruler (e.g. TheraBite® measuring disc) is used in literature [7]. However, most authors use 3-point scales on tongue mobility [4–6]. Disadvantage of the latter is that it only gives a broad idea on tongue ROM since no exact measurements are performed. The ruler constitutes more detailed information, although (near to) physical contact is needed which might influence motion. Moreover, only one value for distance is registered and not the actual 3D position of the tongue. This is an important aspect, particularly if one realizes that within one-dimensional assessment multiple directions of the tongue position remain unexplored. The assessment of three coordinates (i.e. X–Y–Z values) results in more detailed information on the exact location of the tongue. Furthermore, it would be desirable if the actual movements could be stored, so the pre-operative tongue movements can be compared to altered movements in a later stage of treatment.
This study aims at the development of an objective and accurate grading scale to assess tongue ROM after partial glossectomy. During assessment, possible interference of mobility should be kept to a minimum and movements should be stored for later comparison. We investigated the reliability of a triple-camera setup for the measurement of tongue ROM with respect to intrarater, interrater and test–retest reliability. Secondly, feasibility of the measuring system was tested in ten patients surgically treated for oral tongue carcinoma. This is a first step towards prediction of expected function loss for different stages of oral tongue carcinoma.
Materials and Methods
Participants
The first part of this study consists of 15 healthy volunteers who were recruited on institute premises. Participants had to be 18 years or older and were eligible if they were healthy and had no history of tongue carcinoma, no neurovascular diseases or other conditions that could influence tongue mobility.
Secondly, to assess feasibility of the method, we examined tongue ROM of ten patients who had undergone a partial glossectomy. Surgery had to be at least 6 months ago, and patients did not receive radiotherapy at the tongue.
Movements
All participants were asked to perform five movements: reach with tip of the tongue to the left side (I), reach with tip of the tongue to the right side (II), protrude the tongue (III), elevation: reach to the tip of the nose (IV) and depression: reach to the tip of the chin (V). Participants were asked to reach as far as they were able in all directions. Movements were performed twice: firstly as described above and secondly with a plastic widener in place to retract the lips. The widener was included in the first part of this study in the search to retain the most controlled and reliable measurement condition. Because of no additional value, this device was abandoned in the second part of this study when tongue ROM in patients was assessed.
Camera System and Measurements
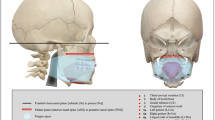
Tongue movements were recorded with a standardized camera setup consisting of three cameras in a fixed position. This setup made it possible to reconstruct 3D coordinates based on known positions in the three video frames. The chosen cameras are the Basler® avA1000-100gc. Its specifications are resolution 1024 × 1024 pixels, frame rate of 101 fps, sensor HAI-1050 ½ inch, connections gigE 12-pinconnector, size of 40.7 × 62 × 62 mm and weight 300 g. A fixed focal 8.5-mm lens is mounted on these cameras in order to get a view of 25 cm in height (roughly the head size) when placing them 30 cm from the subject. Cameras were placed at a 15-cm distance of each other. Lateral ones were placed in 20° rotation towards the middle (Fig. 1). The calibration parameters of the cameras were obtained with a calibration object consisting of 27 beads that are arranged on a 3 × 3 × 3 orthogonal grid.
For 3D information on tongue position, two reference points were applied on the surface of the tongue and four additional markers on the face: I-tip of the nose, II-centre between both eyes (nasion), and III and IV-midline both eyes (Fig. 2). By using these four reference points, measurements were corrected for any head movement during capturing of the tongue movements.
Before recorded movies were analysed offline, the computer program needed to be calibrated to the 3D location of the interdental papilla in relation to the reference markers on the face. Hereby, the system sets the interdental papilla as the centre and distances from there to the tip of the tongue were calculated, although only the reference markers were selected. This is necessary, because the interdental papilla of the maxillary midline was not visible during all tongue movements. For analysis, the frames in which the maximal tongue excursion was achieved were selected for all five movements. Next, in these frames, the four reference markers and the tongue tip were selected manually. The 2D image coordinates of each marker visible in the frames of the three cameras were reconstructed to a 3D position. The root mean square error of this 3D localization was 0.73 mm, estimated with a leave-one-out method. From the 3D positions of the markers, the distances between the interdental papilla of the maxillary midline and the tip of the tongue were calculated.
To determine intrarater variability, the five tongue distances of all participants were measured three times in a row by the first author. For interrater variability, the second author also measured all tongue movements of eight participants three times in a row. The second author was blinded for the measurements made by the first author. Test–retest reliability was assessed by recording tongue ROM of all participants for a second time on another day. Because healthy adults were tested, symmetrical movements were expected. Thus, for the method to be valid, left and right distances should be equal, and therefore, differences in left–right distances were calculated.
The Medical Ethic Committee of our institute did approve the study protocol, and informed consent was received of all participants and patients.
Statistical Analysis
All statistical analyses were performed using IBM SPSS statistics version 20.0. As a degree of reliability of the method, intra class correlation coefficient (ICC) is computed and intrarater, interrater and test–retest ICCs are given. An ICC of >0.75 is considered as a very high strength of agreement, a value of 0.4–0.75 between fair and good agreement, and an ICC value of <0.4 as poor agreement. Differences of tongue movements between participants, as well as the influence of other factors (the presence of a widener and differences between days, gender or raters) on tongue movements, were analysed with regression analysis. Wald χ 2 p values ≤0.05 are considered as a significant difference between groups.
Results
We included 15 healthy participants and ten surgically treated oral tongue cancer patients. All participants were able to perform all movements as instructed and were recorded successfully. Application of the reference markers and recording of tongue movements took between 45 and 90 s per participant.
The group of healthy participants consisted of eight men (53 %) and seven women (47 %) with a mean age of 27 years (SD 2.4). Mean distances between the tip of the tongue and the interdental papilla of the maxillary incisors without mouth widener were 36.1 mm (protrusion), 49.0 mm (left), 48.6 mm (right), 19.4 mm (elevation) and 62.3 mm (depression). With mouth widener, distances were 36.3, 44.5, 44.5, 17.1 and 55.3 mm for protrusion, left side, right side, elevation and depression, respectively (Table 1).
Reliability
Intrarater reliability measured by the first author showed an ICC of 0.99 (95 % CI 0.99–0.99). The ICC measured by the second author was 0.99 (95 % CI 0.98–0.99). Measurements between the two separate raters showed an ICC of 0.95 (95 % CI 0.93–0.97) as a degree of interrater reliability. When measurements of day 1 and day 2 are compared, an ICC of 0.93 (95 % CI 0.89–0.93) was found as a degree of test–retest reliability (Table 2).
Mouth Widener
All participants performed the five movements with and without mouth widener. There was a significant difference between the overall distances with and without the device in situ (p < 0.001). When sides were analysed separately, the difference was found for the two lateral movements ‘left’ and ‘right’, both p < 0.001, and for ‘depression’ of the tongue (p < 0.001). Elevation and protrusion were not influenced by the presence of the widener; p = 0.06 and p = 0.14, respectively. These results are summarized in Tables 1 and 3.
Symmetry of Movement
Distances of the forward movement differed significantly of both lateral movements left and right (p < 0.001). Distances towards left and right showed no significant difference (p = 0.509) (Table 3).
Gender
The healthy participants group consisted of 15 persons of which eight were men and seven were women. There was no significant difference between the range of tongue motion in men and women, β = 1.29, χ 2(1) = 0.44 and p = 0.51 (Table 3).
Inter-participant Variability
Mean distances of tongue ROM of all 15 participants are described in Table 1. Measurements of participant no 2 were most near the mean values of the total group. Therefore, participant two was set up as comparison participant in regression analysis. This analysis showed that there was a non-significant difference with only one other participant (Nos. 2 and 3 with β = 0.11, χ 2(1) = 0.20, p = 0.652). All other participants significantly differed in tongue ROM of subject 2 with p < 0.001.
Patients
To determine the feasibility of the method, we included ten partial glossectomy patients in this study. The patient group consisted of five men (50 %) and five women (50 %) with a mean age at the time of resection of 65 years (SD 10.0). All patients underwent lateral tongue resection with primary closure. Five patients had stage I disease (50 %), one patient stage II (10 %) and four patients stage III (40 %). Two patients underwent re-excision because of incomplete resection and one other patient, 4 months later, because of leukoplakia. Only one patient underwent selective neck dissection and received post-operative radiotherapy on the ipsilateral neck. Mean time between operation and assessment of tongue ROM was 29 months (SD 18.1).
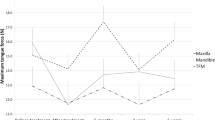
Mean distances between the tip of the tongue and the interdental papilla of the maxillary incisors were 35.9 mm (protrusion), 42.3 mm (left), 47.3 mm (right), 17.8 mm (elevation) and 52.1 mm (depression) (Table 4). These measurements did not differ significantly from the overall measurement of the healthy subjects [t (1134) = 1.86; p = 0.06, 95 % CI −0.1 to 4.96].
In healthy individuals, lateral movements did not differ significantly. The lateral movements of patients, divided in resection side versus contralateral side, were significantly different (p < 0.001) with distances of 47.5 and 42.2 mm, respectively (Table 4).
When measurements per patient were analysed, it is seen that, in general, the lateral movement towards the resected side is not altered after partial glossectomy.
Discussion
This study shows a new and reliable technique for the assessment of the range of motion of the tongue with excellent intrarater, interrater and test–retest reliability. Furthermore, it shows that there is a high degree of symmetry in the range of tongue motion in healthy adults. The used 3D camera setup seems a promising method to accurately measure tongue ROM. The detected altered tongue movements in patients treated for oral tongue carcinoma is the first step towards a tongue mobility grading system, followed by predicting functional consequences after tongue surgery.
In this study, an arbitrary study group of 15 participants was chosen. Furthermore, the study group consisted of participants with a mean age of 27 years which is lower than the average patient with oral cavity carcinoma [13]. Because this study aimed to test the reliability of a new method to assess tongue ROM, this difference seems not to be of importance. Also, tongue function as mean swallowing pressure does not differ between younger and older age groups [14].
Regression analysis in the participant group showed significant differences between tongue ROM in all directions of all but two subjects, so no standard or minimal ROM can be suggested from this study. Nevertheless, we showed that there definitely is a measurable difference in tongue ROM in patients with oral tongue carcinoma compared to healthy subjects. Especially, the asymmetry of lateral movement in patients seems to be of importance. We hypothesize that patients with a smaller tongue ROM before treatment are more likely to develop larger functional problems compared to patients with a larger tongue ROM with the same tumour (or resection) volume and location. This might be one of the core concepts why patients with the same tumour characteristics evolve different speech and swallowing problems [6].
To our knowledge, only a few studies describe movements of the tongue in relation to function. Matsui et al. found that intelligibility with respect to objective (as measured by a qualified speech pathologist) and naïve (as experienced by the patient) speech is correlated with tongue tip elevation [6]. In this study, tongue tip elevation was measured on a 3-point elevation score: 0: no elevation possible; 1: can elevate but not contact the palate and 2: can reach the palate. Less tongue mobility was significantly correlated with lower speech functioning scores. The same correlation was found in the study of Bressmann et al. where nine different tongue movements were tested on a 3-point scale (1: normal, 2: mild impairment, 3: marked impairment) [5]. In both studies, no absolute measurements of the tongue movements were performed, and therefore, it gives only a broad idea about the tongue mobility and subtle differences cannot be measured. Lazarus et al. developed a tongue ROM score (combination of protrusion, lateralization and elevation score) with the use of a ruler (the TheraBite® measuring disc) [7]. They found statistical significant correlation between ROM scores and eating and oral transport scores, with lower ROM indicating larger functional deficits. Although a ruler was used and more detailed information was assessed, in the analysis, the patients were divided into subgroups of ‘normal’, ‘mild-moderately impaired’, ‘severely impaired’ and ‘totally impaired’ movement. As our study shows no ‘normal’ ROM seems appropriate because of a large variation in distances (in all directions) between healthy subjects exists. Also no additional data on the test–retest or rater reliability of the measuring disc are delivered.
Tongue movements vary widely between individuals. Therefore, if the aim is to determine the surgical effect on mobility, tongue movements can only be compared to the pre-operative measurements within the same patient. To our knowledge, in literature, no 3D measurement tool had been described to assess tongue range of motion. Instead, a commonly used tool is a simple ruler which constitutes a practical and easy way to assess distances [7, 8, 15]. Apart from the earlier-mentioned (near to) physical contact during assessment, and the lack of digitalization of the movements for second analysis, there are more limitations to this method: Only one value for distance is registered and not the actual 3D position of the tongue. This is an important aspect, particularly if one realizes that within one-dimensional assessment, multiple directions of the tongue position remain unexplored. With the use of a 3D camera setup, three coordinates of the tongue tip are assessed (X–Y–Z values), which makes it possible to correct for (small) differences in direction. Therefore, apart from the advantages described earlier, more detailed information is acquired through the 3D camera setup, especially on the exact location of the tongue’s tip.
To assess feasibility of the 3D camera setting in measuring tongue ROM, we analysed five different tongue movements: elevation, depression, protrusion and both lateral directions. These movements were chosen based on international literature. Matsui et al. used elevation of the tongue’s tip and dorsum as a mobility test, and Bressmann et al. used nine different movements for a combined mobility score, and no sub-analyses of the different movements are described [5, 6]. In a third study, of Konstantinović and Dimić, tongue’s mobility was also measured, but correlation with functional aspects was not investigated [4]. They used a 3-point scale, and six different movements were tested. This study showed that lateral movements significantly differed between patient groups with different reconstructions, and therefore, we included lateral movements next to protrusion. Elevation and depression of the tongue body are of great functional importance as they reflect the ‘finger function’ of the tongue that facilitates manipulation and shaping of the food bolus and clearance of food particles from the labial and buccal sulcus, as described in Chepeha et al. [16]. Future research should focus on correlation of altered ROM and functional consequences. We measured the maximal possible movement of the tongue in all directions, because reliability of the method was the first incentive of this study. Question is if, or to what extent, these maximal possible positions contribute to the swallow and speech function. Future research should focus on this aspect. Nevertheless, detailed information on tongue positions can accurately be acquired with the triple-camera setup.
In the search to retain the most controlled and thus reliable measurement condition, we added a mouth widener in the test array. Results show that without the mouth widener in place, good and reliable measurements of the range of tongue motion can be made as well. Also, the presence of a mouth widener significantly restricted tongue ROM for the movements ‘left’, ‘right’ and depression and therefore should be excluded in future experiments.
The 3D camera setup has previously been used in our research group and therefore available to assess 3D location on tongue movements [17]. However, a similar setup could also be made of two regular consumer cameras with a lower frame rate, or even just by capturing pictures. In preliminary studies, such a less costly setup was used with a comparable calibration error.
With this novel technique on the measurement of tongue movements, more detailed information on tongue ROM can be assessed and smaller differences will be detected. This method allows one to objectively register 3D tongue movements and creates an accurate and reliable dataset for pre- and post-operative measurements. In addition, this video system allows one to capture other aspects such as tongue shape and velocity measurement, if desirable for further studies. A large study on tongue movement outcomes is needed for a good perception on the deteriorating effect of surgery on tongue mobility. Since the extra effort is limited, we believe this method can be an expedient alternative. Eventually, correlation of tongue movements with functional outcomes will assist head and neck surgeons to inform patients better, than they can do nowadays, with respect to expected function loss.
Conclusion
This 3D camera setup is a reliable method to assess tongue ROM in healthy subjects as well as in patients who underwent partial glossectomy. Our results show an excellent intrarater, interrater as well as test–retest reliability. Regression analysis confirmed these findings and also showed symmetry of movement (left and right distances as being equal) as a core concept of tongue ROM in healthy adults.
Capturing tongue movement is challenging, and tongue ROM had never been evaluated in detail as it has been in this study. With this 3D camera setup, a first step in resolving this problem has been made. Future experiments should confirm the reliability and expand the possibilities of this measuring system in capturing tongue movements in patients treated for different stages of oral tongue carcinoma.
References
Warnakulasuriya S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2008;45:309–16.
www.cijfersoverkanker.nl. Accessed 12 July 2014.
Sessions DG, Spector GJ, Lenox J, Haughey B, Chao C, Marks J. Analysis of treatment results for oral tongue cancer. Laryngoscope. 2002;112:616–25.
Konstantinović V, Dimić N. Articulatory function and tongue mobility after surgery followed by radiotherapy for tongue and floor of the mouth cancer patients. Br J Plast Surg. 1998;51:589–93.
Bressmann T, Sader R, Whitehill TL, Samman N. Consonant intelligibility and tongue motility in patients with partial glossectomy. J Oral Maxillofac Surg. 2004;62:298–303.
Matsui Y, Ohno K, Yamashita Y, Takahashi K. Factors influencing postoperative speech function of tongue cancer patients following reconstruction with fasciocutaneous/myocutaneous flaps–a multicenter study. Int J Oral Maxillofac Surg. 2007;36:601–9.
Lazarus CL, Husaini H, Jacobson AS, Mojica JK, Buchbinder D, Okay D, et al. Development of a new lingual range-of-motion assessment scale: normative data in surgically treated oral cancer patients. Dysphagia. 2014;29:489–99.
Husaini H, Krisciunas GP, Langmore S, Mojica JK, Urken ML, Jacobson AS, et al. A survey of variables used by speech-language pathologists to assess function and predict functional recovery in oral cancer patients. Dysphagia. 2014;29:376–86.
Kreeft MA, Tan IB, Leemans CR, Balm JMA. The surgical dilemma in advanced oral and oropharyngeal cancer: how we do it. Clin Otolaryngol. 2011;36:260–6.
Kreeft AM, Rasch CRN, Muller SH, Pameijer FA, Hallo E, Balm AJM. Cine MRI of swallowing in patients with advanced oral or oropharyngeal carcinoma: a feasibility study. Eur Arch Otorhinolaryngol. 2012;269:1703–11.
Rastadmehr O, Bressmann T, Smyth R, Irish JC. Increased midsagittal tongue velocity as indication of articulatory compensation in patients with lateral partial glossectomies. Head Neck. 2008;30:718–27.
Lazarus CL, Logemann JA, Rademaker AW, Lurie TRH, Larson CR, Mittal BB. Swallowing and tongue function and oropharyngeal cancer. J Speech Lang Hear Res. 2000;43:1011–24.
www.oncoline.nl/mondholte-en-orofarynxcarcinoom. Accessed 17 July 2014.
Youmans SR, Youmans GL, Stierwalt JAG. Differences in tongue strength across age and gender: is there a diminished strength reserve? Dysphagia. 2009;24:57–65.
Van der Molen L, van Rossum MA, Ackerstaff AH, Smeele LE, Rasch CRN, Hilgers FJM. Pretreatment organ function in patients with advanced head and neck cancer: clinical outcome measures and patients’ views. BMC Ear Nose Throat Disord. 2009;9:10.
Chepeha DB, Teknos TN, Shargorodsky J, Sacco AG, Lyden T, Prince ME, et al. Rectangle tongue template for reconstruction of the hemiglossectomy defect. Arch Otolaryngol Head Neck Surg. 2008;134:993–8.
Van Alphen MJA, Eskes M, LE Smeele, van der Heijden F. In vivo intraoperative hypoglossal nerve stimulation for quantitative tongue motion analysis. Comput Methods Biomech Biomed Eng imaging Vis. 2015;. doi:10.1080/21681163.2015.1072056.
Acknowledgments
This research project was supported by private funding from Mr D. van den Brink and Mrs A. van den Brink. The 3D camera setup was funded by the Maurits and Anna de Kock Foundation. The authors thank Lisette van der Molen for her contribution in completion of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
van Dijk, S., van Alphen, M.J.A., Jacobi, I. et al. A New Accurate 3D Measurement Tool to Assess the Range of Motion of the Tongue in Oral Cancer Patients: A Standardized Model. Dysphagia 31, 97–103 (2016). https://doi.org/10.1007/s00455-015-9665-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-015-9665-7