Abstract
Introduction
Accurately measuring tongue space is challenging, but this information can be useful to many dental specialties. This study was intended to estimate the reliability of using cone-beam computed tomography (CBCT) to measure tongue space, which includes tongue volume and the oral cavity air capacity.
Methods
For this preliminary study, CBCT images from ten participants (five females and five males, mean age of 29.8 ± 3.3 years) were available for evaluation. Each participant was radiographed two times (T0 and T1). The average time between T0 and T1 was 15.8 ± 3.7 days. CBCT scans were standardized to reduce variability. Three-dimensional landmarks were established to identify tongue space and 3D image analysis software (SimPlant® 17 Pro; Materialise Dental, Leuven, Belgium) was used to measure the volume circumscribed by the landmarks. Two investigators independently calculated airway, tongue dimensions, and total tongue space for CBCT image T0 twice (day 1 and day 14), and T1 once. Intraclass correlation coefficients (ICCs) were used to estimate intra-rater and inter-rater reliability. Bland–Altman charts were constructed to demonstrate agreement within and between raters.
Results
The intra-rater and inter-rater ICCs of the CBCT measurements at T0 were excellent (> 0.90). Measurements for T0 vs. T1 show good (0.75–0.90) intra-rater and excellent (> 0.90) inter-rater reliability. Bland–Altman charts show that 90–95% of the total measurements fall within the 95% limits of agreement for both intra- and inter-rater pairs
Conclusions
The results of this preliminary study suggest that the landmarks chosen to measure the overall tongue space are reproducible and can be measured clearly using CBCT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tongue space may be defined as the area the tongue occupies. This space may include tongue volume and the oral cavity air capacity. Understanding tongue space is important for orthodontists. Currently, they do not focus on the changes they create in tongue space during treatment, possibly due in part to the lack of agreement and a specific method on how to measure tongue space. Previous methods have measured the area of the tongue using lateral cephalogram [1,2,3,4], which failed to show complex three-dimensional (3D) variations including mobility, shape variation, and variable posture of the tongue. They lacked natural radiographic marker points and did not measure tongue space in three dimensions. Cone-beam computed tomography (CBCT) can do this. The use of CBCT in orthodontic practice has slowly increased to the point where it is now being used for diagnosis, treatment planning, and research [5]. Image quality is comparable to that obtained with computed tomography (CT), but with lower effective radiation dosage [6].
Orthodontic treatment commonly involves tooth extraction or surgical intervention, procedures that may have an impact on the amount of available tongue space. Inadequate tongue space can lead to problems such as tongue thrusting, which may lead to additional problems. Inadvertent biting of the lateral border of the tongue may also occur [7,8,9]. Information concerning tongue space is important, because discrepancies between the inward force of cheeks and lips and the outward forces of the tongue can lead to malocclusions, and change the mandibular posture, or vertical face height [10, 11]. The influence of the tongue on the morphology of dental arches and occlusion depends on the amount of space it occupies, as well as its posture and mobility [11]. It is important to control the relationship between tongue volume and the oral cavity capacity, because a reduction in overall tongue space may increase the chance of relapse following treatment.
Anatomical definitions of the tongue and the tongue space are inconsistent [12]. The anterior portion of the tongue is attached to the cingulum of the anterior teeth and the mandible, while the posterior portion of the tongue may go all the way to the airway. The tongue occupies the anterior wall of the oropharynx and connects with the soft palate, epiglottis and pharynx [13]. Past modalities of measuring tongue volume and oral cavity capacity have included MRI, lateral cephalograms, alginate impressions, fluid displacement, and CT [9, 14, 15]. Direct measurements are problematic because the posterior portion of the tongue is difficult to measure [9, 14]. Aside from CT, no technique is available that can accurately evaluate the volume of the tongue relative to the oral cavity [12]. CBCT is useful for investigating the morphologic structures in the oral cavity. 3D image quality is comparable to medical CT, but with a lower effective radiation dose [16]. When using CBCT, the patient is sitting upright, which prevents the tongue from falling back under the influence of gravity.
The purpose of this study was to examine the reliability of a novel method for using CBCT to measure tongue space in orthodontic patients. This protocol, if shown to be reliable, may allow orthodontists to evaluate changes in the airway and tongue space resulting from treatment.
Materials and methods
The goal of this preliminary study was to determine if the protocol and/or chosen landmarks yielded acceptably reliable inter-rater and intra-rater measurements of tongue space before proceeding with a confirmatory study.
Subjects
Participants were selected from among patients who had a CBCT image scanned previously using a standardized protocol at the Postgraduate Orthodontic Program, Arizona School of Dentistry & Oral Health, A.T. Still University, Mesa, Arizona. Each participant in the study was informed of the effective dose of radiation that they would incur and consented to voluntarily enroll in the study. CBCT images were de-identified. A total of ten adults (five females and five males) were used in this study, mean age, 29.8 ± 3.3 years. The minimum and maximum ages of participants were 24.7 and 36.3 years, respectively. Participants were all Caucasians with Class I malocclusion and 1–3 mm of anterior overjet and overbite. The patients did not have any craniofacial deformity, abnormal oral function, moderate (4–6 mm) or severe crowding (> 7 mm) in the anterior teeth, nor a history of maxillofacial surgery. Institutional review board approval was granted by A.T. Still University (IRB Protocol #2018-177) in Mesa, Arizona to conduct this study.
CBCT scans
Two CBCT scans (T0 and T1) were taken for each of the 10 participants using a standardized protocol. T0 was the initial scan and T1 was a new scan taken roughly 2 weeks later. The CBCT was taken by previous investigators for creating a protocol for standardization of CBCT volume acquisition of the airway in the field of orthodontics. The average interval between T0 and T1 was 15.8 ± 3.7 days. We chose a sample size of 10 subjects with two observations per subject to achieve 90% power to detect ICC of 0.90 under the alternative hypothesis that the intraclass correlation under the null hypothesis is 0.50, alpha = 0.05, two tailed. The CBCT images were taken using i-CAT FLX® V-Series (i-CAT; Hatfield, Pennsylvania, USA) with ‘3D Ceph Quick Scan+’ setting to give the provider/investigator the necessary field of view (FOV) to capture the essential landmarks, while exposing participants to the least amount of radiation feasible. The volume size of the scan was 16 cm × 13 cm, voxel size of 0.6 mm, the scan time of 4.8 s, Dose Area Product (DAP) of 99.2 mGy cm2, and effective dose of 11.4 µSv [17]. The images were taken with the Frankfort horizontal plane (orbitale to porion) parallel to the floor. Each patient was asked to place his or her tongue to the most anterior superior position, and their teeth in full occlusion or maximum intercuspation. Patients were then asked to take a deep breath, exhaled, and hold his or her breath after the end of expiration, without swallowing while the CBCT was taken. Breath holding at this moment provides a static pharyngeal airway size that can be recorded consistently in all CBCT scans and reducing variations caused by changes in pharyngeal airway caliber during the respiratory cycle [18, 19].
3D image analysis
The participants’ Digital Imaging and Communications in Medicine (DICOM) data were imported into 3D image analysis software (SimPlant® 17 Pro; Materialise Dental, Leuven, Belgium) to facilitate the measurement of the tongue space. Before analyzing the CBCT images, the head orientation of each patient was standardized using three planes: Frankfort horizontal, midsagittal, and transporionic planes. The Frankfort horizontal plane was defined by right and left porion and orbitale. The midsagittal plane was defined as the plane orthogonal to axial and coronal planes passing through the nasion landmark. The transporionic plane was defined bilaterally by porion landmarks and perpendicular to the Frankfort horizontal plane. In the sagittal, axial, and coronal views, the volume was rotated until the Frankfort horizontal plane was oriented horizontally, and the midsagittal, and transporionic planes were oriented vertically [20, 21].
Definitions of cephalometric and anatomic landmarks
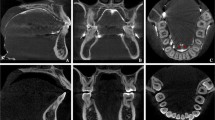
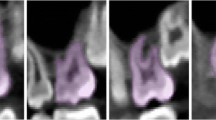
Landmarks were established for the tongue space (Fig. 1 and Table 1). The superior border of the tongue space was the palatal plane [anterior nasal spine (ANS) to posterior nasal spine (PNS)], parallel to the Frankfort horizontal plane (Fig. 2). This included the height of the palatal vault (HPV), which was the distance from the maxillary occlusal plane (tangential to the most distal points of the maxillary first molars) to the deepest point of the palate in the plane. The anterior border of the tongue space was the cingulum of the anterior teeth when they are in maximum intercuspation. The lateral border of the tongue space was the lingual side of the mandible (both right and left) all the way forward to the genial tubercle (GT). The inferior border of the tongue space was the hyoid bone to the genial tubercle and the anteroinferior point of the third cervical vertebra (C3) (Fig. 3). The posterior border of the tongue space was the left and right side gonion (Go) perpendicular to the Frankfort horizontal plane.
Landmarks for measuring tongue space. The superior landmarks and border of tongue space is the palatal plane [anterior nasal spine (ANS) to posterior nasal spine (PNS)], parallel to the Frankfort horizontal plane [orbitale (Or) to porion (Po)]. The lateral landmark is the lingual of the mandible from gonion (right and left) to the genial tubercle (GT); the lingual side of the dentition is also part of the lateral border. Posteriorly, the tongue space goes all the way to the gonion of the mandible and includes part of the airway, specifically portions of the oropharynx and hypopharynx. The inferior border of the tongue space is the hyoid bone to the GT and to the most anteroinferior point of the third cervical vertebra (C3)
Posteriorly, the tongue space includes part of the airway, specifically part of the oropharynx. The oropharynx was divided into two areas: velopharynx and glossopharynx [22]. The velopharynx was defined from the horizontal level of the palatal plane to the horizontal level of the end of the uvula. The glossopharynx was defined from the horizontal level of the end of the uvula to the horizontal level of the C3 (the most anteroinferior point of the third cervical vertebra) [23]. The overall tongue space included the oral cavity and part of the airway superior to the hyoid bone to GT and anteroinferior point of C3 and inferior to the palatal plane (Fig. 1).
Data collection
Two orthodontists (M.Z. and Y.S.) completed the data collection. M.Z. and Y.S. are fellows in their respective departments and both have extensive training with the 3D image analysis software (SimPlant® 17 Pro; Materialise Dental, Leuven, Belgium). The first CBCT scan (T0) was landmarked and airway and tongue dimensions along with total tongue space were measured. The landmarks were then removed, and 14 days later, the landmarks were replaced and measured for a second time on T0 CBCT scans. The landmarks were also placed on the T1 CBCT scans, and the airway, tongue dimension, and tongue space were measured.
Statistical analysis
Data were analyzed using SPSS version 25 (IBM Corporation, Armonk, New York, USA). Reliability analysis was conducted to assess the level of agreement across time points and raters using a two-way random-effects (consistency) model based on a single rating. For the ICC estimates, values of less than 0.50 were to be considered poor, between 0.50 and 0.74 as moderate, between 0.75 and 0.90, good, and above 0.90, excellent reliability [24, 25]. Inter- and intra-rater ICC’s were calculated for airway, tongue, and total tongue space (tongue volume and the oral cavity air capacity) measurements.
To further assess and visualize agreement on the measurements, Bland–Altman plots were constructed based on mean differences [24, 25]. This allowed us to evaluate bias between mean measurement differences, and to estimate an agreement interval within which 95% of the differences between the two measurements should fall. In Bland–Altman charts, the Y-axis shows the difference between the two paired measurements (A–B) and the X-axis is the average of these measures [(A + B)/2]. Bland and Altman recommended that 95% of the data points should lie within ± 1.96SD of the mean difference [26]. The average of paired differences would be zero if no bias existed between the raters.
Results
Analysis of CBCT scan T0 measured at day 1 and day 14
Table 2 provides the average measurements (means and standard deviations) for T0 and T1 for both reviewers. Table 3 presents the descriptive statistics illustrating the difference in scores of CBCT scan T0. Table 4 presents the ICCs for the intra-rater reliability when comparing the measurement of CBCT scan T0 measured at day 1 and day 14. The variables exhibited an excellent ICC for all the intra-rater repeatability measurements. The ICC for airway measurement was 1.00; tongue measurement was 0.96; and total tongue space measurement was 0.97.
The results for inter-rater reliability of the CBCT scan T0 measured at day 1 and day 14 were also excellent (Table 5). The ICC for airway measurement was 0.99; for tongue measurement, 0.97; and for total tongue space measurement, 0.99.
Figure 4 provides the Bland–Altman charts for the CBCT scan T0 measured at day 1 and day 14, comparing the scan readings for both intra- and inter-rater reliability. The intra-rater plots (Fig. 4a–c) showed acceptable reliability. For all the measurements (airway, tongue, and total tongue space measurements), 19 out of 20 measurements (95%) fell within the limits of agreement. The inter-rater plots (Fig. 4d–f) show that 19 of 20 (95%) measurements fell within the limits of agreement for the airway and total tongue space measurements. Eighteen out of 20 (90%) tongue measurements fell within the limits of agreement.
Analysis of CBCT T0 vs. T1
Table 6 presents the descriptive statistics for samples of CBCT T0 vs. T1. Table 7 presents the ICCs for the intra-rater reliability for measurements of CBCT T0 vs. T1. The variables exhibited good intra-rater reliability. The ICC for the airway measurement was 0.86, for tongue measurement 0.83, and for the total tongue space measurement, 0.84.
The results for the inter-rater measurements of CBCT T0 measured at day 1 and day 14 were also excellent and showed high reproducibility (Table 8). The ICC for airway, tongue, and total tongue space measurements was 0.99.
Figure 5 provides the Bland–Altman charts for measurements of CBCT of the 10 participants at T0 vs. T1, including both the intra- and inter-rater reliability. The intra-rater plots (Fig. 5a–c) show acceptable reliability for all the measurements (airway, tongue, and total tongue space measurements), except for one patient. Eighteen of 20 measurements (90%) fall within the limits of agreement. The inter-rater plots (Fig. 5d–f) show that 19 out of 20 (95%) measurements fall within the limits of agreement for the airway, tongue, and total tongue space measurements.
Based on the high concordance shown in Fig. 5 for inter-rater measurements (D–F), and the more variable measurements for inter-rater measurements (A–C), it appears that the head posture of one patient was in a significantly different position between the two scans. The two dots that appear above the upper limit of agreement for the inter-rater charts are from the same patient. Both raters scored this patient very differently for the two measurements. However, their measurements agreed (inter-rater) for this patient.
Discussion
The objective of this study was to introduce landmarks and develop a new reliable protocol to measure tongue space from CBCT images. Tongue space is of interest to many specialties, including orthodontists, surgeons, and sleep medicine professionals, but a procedure for acquiring this information reliably has not been agreed upon. One reason for this may be the resolution limitations of early CBCT technology. CBCT was introduced to dentistry in 1998 in Europe and approved for use in the USA in 2001 [27]. Unfortunately, early images were not of high quality, and few providers had access to CBCT. With the availability of CBCT and advanced 3D software, 3D craniofacial anatomy has become easier to measure and analyze [5]. The effective dose for CBCT is lower than a standard medical CT [16, 28]. Magnetic resonance imaging (MRI) uses non-ionizing electromagnetic radiation and allows for repetitive 3D imaging without harmful radiation exposure, so while it is a viable option for measuring tongue space, it is expensive, has limited availability, is time-consuming, adds concern for claustrophobic patients, has magnetic safety concerns, and does not produce ideal cortical bone contrast [28, 29].
There has been no standardized protocol for patient positioning during CBCT scan acquisition. Minor changes to head position and tongue position, the need for patients to hold their breath and not swallow, and the scanning period are all factors that could impact the accuracy of the measurement and result in analytical challenges [30, 31]. For example, studies have shown the position of the hyoid bone can be influenced by head posture and will be altered by anteroposterior changes in the head position [32,33,34]. Because a standardized protocol for taking CBCT scans is applied to all patients at our university, variability is reduced and CBCT scans are reproducible.
The CBCT images used in this study were from patients who had already had a CBCT image scanned previously using a standardized protocol at the Postgraduate Orthodontic Program. All participants consented to voluntarily enroll in the study. The effective dose of the scan was 11.4 μSv. In comparison, a one-way coast-to-coast flight exposes each passenger 35 μSv, and the daily background radiation on average is 4.11–9.59 μSv [17, 35]. This shows that the amount of radiation the participants were exposed to for both CBCT scans (T0 and T1) was comparable to simply being alive for 2 days.
In this study, the landmarks circumscribing the areas of interest were carefully selected based on the anatomy of the tongue and airway (Fig. 1 and Table 1). Each of these landmarks is easily recognizable and by having a standardized protocol for capturing CBCT images, these landmarks should provide accurate and reproducible measurements. The overall tongue space has to reflect all the space that the tongue occupies during normal activities such as breathing, speech, swallowing, and mastication. Several of the chosen landmarks were hard tissue instead of soft tissue because the soft tissues are continuously moving or may move depending on the activities.
The superior border of the tongue space was the palatal plane [anterior nasal spine (ANS) to posterior nasal spine (PNS)]. This was chosen because there were lots of changes to the position of the soft palate. For example, on the onset of the swallowing reflex, the soft palate is being drawn upward [36]. Posteriorly, the tongue space reaches the gonion of the mandible, and part of the airway, specifically portions of the oropharynx, which can be divided into the velopharynx and glossopharynx. The oropharynx extends from the soft palate to the most anteroinferior part of the C3 and includes the base of the tongue [37]. The inferior landmarks include the genial tubercle, hyoid bone, and anterior, inferior of C3. The reason we chose the landmarks described above is that the floor of the mouth consists of the geniohyoid and mylohyoid muscle. The origin of the geniohyoid muscle is the inferior mental spine of the mandible, while the insertion is the hyoid bone. The origin of the mylohyoid muscle is the mylohyoid line of the mandible, and the insertion of the muscle is the body of the hyoid bone. The C3 was chosen, because the hyoid bone lies at the level of C3 [38]. Since the hyoid bone is the inferior border of the tongue space, we proposed the C3 is a good reference point for the posteroinferior portion of the tongue space.
The method proposed in this study using the chosen anatomical landmarks suggests that tongue space can be measured reliably from CBCT imaging. Reliability was assessed in this study by ICC, measurement errors, and the Bland–Altman method. Even if ICC values are excellent (> 0.90), they may still hide clinically important measurement errors [39]. However, the Bland–Altman charts support the accuracy of the landmarks chosen for this study. When comparing the measurement of the T0 CBCT images at day 1 and day 14, the airway, tongue dimensions, and total tongue space measurements all have excellent repeatability for both intra- and inter-rater measurements, as corroborated by our ICC values (Tables 4, 5). These results suggest that the proposed landmarks were easily identified.
Even though the T0 and T1 CBCT scans were taken using a standardized protocol, it is almost impossible to have identical positioning at different time points. Minor changes in head posture will change the airway, hence possibly changing the overall tongue space [30, 31]. This is clearly illustrated in Fig. 5, where the inter-rater measurements (A–C) show that the head posture of one patient was significantly different between the two scans. The T0 vs. T1 image differences exceeded the limits of agreement, but both raters scored this patient consistently (Fig. 5d–f).
Being able to measure tongue space may help orthodontists better evaluate the effect that orthodontic treatments, such as extraction, expansion, and orthognathic surgery, have on tongue space by comparing pre- and post-treatment volume. This would help practitioners evaluate whether there have been any changes to the airway during treatment, an important topic in the orthodontic field. The limitation of using CBCT to measure tongue space to compare pre- and post-treatment effects is when a practice does not have a standardized protocol to take the CBCT scan. As mentioned earlier, the patient’s posture is very important, especially head and tongue posture. These should be nearly identical when taking pre- and post-treatment CBCT images.
Further studies must be conducted using these well-defined landmarks with larger sample sizes, and multiple investigators to validate the proposed landmarks and protocol for measuring tongue space.
Conclusions
This study provides preliminary evidence that the proposed protocol for measuring tongue space using CBCT imaging is reliable. CBCT images should be captured based on a standardized protocol to reduce variability and increase the accuracy of the measurements. Our findings suggest that the 3D CBCT evaluation for a tongue space, including the actual tongue volume, oral cavity, and air capacity, could be a reliable and reproducible method within and between different raters. Being able to measure tongue space may help orthodontists better evaluate the effects of orthognathic surgery, extraction, expansion of the airway, and overall tongue space relative to orthodontic treatment by comparing pre- and post-treatment volumes.
Change history
03 June 2020
A Correction to this paper has been published: https://doi.org/10.1007/s11282-020-00451-0
References
Kadhum MA. Assessment of tongue space are in a sample of Iraqi adults with Class I dental and skeletal pattern. J Bagh Coll Dentistry. 2015;27:117–20.
Vig PS, Cohen AM. The size of the tongue and intermaxillary space. Angle Orthod. 1975;44:25–8.
Cohen AM, Vig PS. A serial growth study of the tongue and intermaxillary space. Angle Orthod. 1976;46:332–6.
Ardran GM, Kemp FH. A functional assessment of relative tongue size. Am J Roentgenol Radium Ther Nucl Med. 1972;114:282–8.
Kapila SD, Nervina JM. CBCT in orthodontics: assessment of treatment outcomes and indications for its use. Dentomaxillofac Radiol. 2015;44:1–19.
Suomalainen A, Kiljunen T, Kaser Y, Peltola J, Kortesniemi M. Dosimetry and image quality of four dental cone beam computed tomography. Dentomaxillofac Radiol. 2009;38:367–78.
Alpern M. Diagnosing functional tongue space. Orthod Prod 2011.
Waese S. Concern about space for the tongue. Am J Orthod Dentofac Orthod. 2011;140:756.
Takada K, Sakuda M, Yoshida K, Kawamura Y. Relations between tongue volume and capacity of the oral cavity proper. J Dent Res. 1980;59:2026–31.
Uysal T, Yagci A, Ucar FU, Veli I, Ozer T. Cone-beam computed tomography evaluation of relationship between tongue volume and lower incisor irregularity. Eur J Orthod. 2013;35:555–62.
Liegeois F, Albert A, Limme M. Comparison between tongue volume from magnetic resonance images and tongue are from profile cephalograms. Eur J Orthod. 2009;32:381–6.
Lauder R, Muhl Z. Estimation of tongue volume from magnetic resonance imaging. Angle Orthod. 1991;61:175–84.
Tseng Y, Wu J, Chen C, Hsu K. Correlation between change of tongue area and skeletal stability after correction of mandibular prognathism. Kaoshiung J Med Sci. 2017;33:302–7.
Ding X, Suzuki S, Shiga M, Ohbayashi N, Kurabayashi T, Moriayama K. Evaluation of tongue volume and oral cavity capacity using cone-beam computed tomography. Odontology. 2018;106:266–73.
Roehm E. Computed tomographic measurement of tongue volume relative to its surrounding space. Am J Orthod Dentofac Orthop. 1982;81:172.
Lorenzoni D, Bolognese A, Daniela G, Fabio R, Sant’Anna E. Cone beam computed tomography and radiographs in dentistry: aspects related to radiation dose. Int J Dent. 2012;2012:1–10.
Ludlow JB, Walker C. Assessment of phantom dosimetry and image quality of i-CAT FLX cone-beam computed tomography. Am J Orthod Dentofac Orthop. 2013;144:802–17.
Iwasaki T, Saitoh I, Takemoto Y, Inada E, Kakuno E, Kanomi R, et al. Tongue posture improvement and pharyngeal airway enlargement as secondary effects of rapid maxillary expansion: a cone-beam computed tomography study. Am J Orthod Dentofac Orthop. 2013;143:235–45.
Li HY, Chen NH, Wang CR, Shu YH, Wang PC. Use of 3-dimensional computed tomography scan to evaluate upper airway patency for patients undergoing sleep-disordered breathing surgery. Otolaryngol Head Neck Surg. 2003;129:336–42.
Cevidanes L, Oliveira AEF, Motta A, Phillips C, Burke B, Tyndall D. Head orientation in CBCT-generated cephalograms. Angle Orthod. 2009;79:971–7.
Ludlow JB, Gubler M, Cevidanes L, Mol A. Precision of cephalometric landmark identification: CBCT vs. conventional cephalometric views. Am J Orthod Dentofac Orthop. 2009;136:312–410.
Park JH, Kim S, Lee YJ, Bayome M, Kook YA, Hong M, et al. Three-dimensional evaluation of maxillary dentoalveolar changes and airway space after distalization in adults. Angle Orthod. 2018;88:187–94.
Chen Y, Hong L, Wang CL, Zhang SJ, Cao C, Wei F, et al. Effect of large incisor retraction on upper airway morphology in adult bimaxillary protrusion patients. Angle Orthod. 2012;82:964–70.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10.
Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–63.
Altman DG, Bland JM. Measurement in medicine: the analysis of method comparison studies. J R Stat Soc B. 1983;32:307–17.
Hatcher D. Operational principles for cone-beam computed tomography. J Am Dent Assoc. 2010;141:3S–6S.
Shah A. Use of MRI in orthodontics—a review. J Imaging Interv Radiol. 2017;1:1–3.
Tai K, Park JH, Hayashi K, Yanagi Y, Asaumi JI, Iida S. Preliminary study evaluating the accuracy of MRI images on CBCT images in the field of orthodontics. J Clin Pediatr Dent. 2011;36(2):211–8.
Hajeer MY, Millett DT, Ayoub AF, Siebert JP. Applications of 3D imaging in orthodontics: part II. J Orthod. 2004;31:154–62.
Ryan DP, Bianchi J, Ignácio J, Wolford LM, Gonçalves JR. Cone-beam computed tomography airway measurements: can we trust them? Am J Orthod Dentofac Orthop. 2019;156:53–60.
Winnberg A, Pancherz H, Westesson PL. Head posture and hyo-mandibular function in man. A synchronized electromyographic and videofluorographic study of the open-close-clench cycle. Am J Orthod Dentofac Orthop. 1988;94:393–404.
Muto T, Kanazawa M. Positional change of the hyoid bone at maximal mouth opening. Oral Surg Oral Med Oral Pathol. 1994;77:451–5.
Sahin Sağlam AM, Uydas NE. Relationship between head posture and hyoid position in adult females and males. J Craniomaxillofac Surg. 2006;34:85–92.
Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, Gould R, et al. Radiation dose associated with common computed tomography examinations and the associated life-time attributable risk of cancer. Arch Intern Med. 2009;169:2078–86.
Kieser JA, Farland MG, Jack H, Farella M, Wang Y, Rohrle O. The role of oral soft tissues in swallowing function: what can tongue pressure tell us? Aust Dent J. 2014;59:155–61.
Mete A, Akbudak IH. Functional anatomy and physiology of airway. Intech Open J. 2018;89:3–21.
Oh CH, Ji GY, Yoon SH, Hyun D, Choi CG, Lim HK, et al. Surface landmarks do not correspond to exact levels of the cervical spine: references according to the sex, age and height. Korean J Spine. 2014;11:178–82.
Mattos CT, Cruz CV, da Matta TC, Pereira LA, Solon-de-Mello PA, Ruelas AC, et al. Reliability of upper airway linear, area, and volumetric measurements in cone-beam computed tomography. Am J Orthod Dentofac Orthop. 2014;145:188–97.
Acknowledgements
We would like to thank Dr. Brent Jorgensen, Dr. Alan Kai, and Dr. Darshan Patel for providing assistance in the research.
Author information
Authors and Affiliations
Contributions
Each author's contribution to the submission: IAH: contributed to leading the research; reviewing the literature prior to starting the research/manuscript; editing and finalizing the figure; presenting the research in the form of PowerPoint and poster presentation and receiving feedback to improve on the manuscript; writing, reviewing, editing the manuscript; working with all authors and including their input on the manuscript; JHP: contributed to supervising the research; coming with ideas to start and expand on the research; improving illustration, tables, figures; reviewing and editing the research as an author/editor; final approval of the manuscript; corresponding author; EJWL: contributed to expanding the research ideas; introducing a software that will help with the research/data collection; initial input and finalizing on landmarks for the study; reviewing and editing the manuscript as an author and editor; MZ: contributed to reviewing the literature prior to starting the research; data collection since he has the most experience with the software; initial input and finalizing on landmarks for the study; teaching the software to other authors especially Dr. Samawi; editing the paper; YSAS: contributed reviewing the literature prior to starting the research; one of the main people on data collection; finalizing on landmarks for the study; learning and teaching the software to all authors at Mesa, AZ; RCB: contributed to the IRB approval process; doing all the statistical analysis, and writing the statistical analysis for the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Drs. Ivan A. Halim, Jae Hyun Park, Eric J. W. Liou, Mohammad Zeinalddin, Yazan Sharif Al Samawi and R. Curtis Bay declare that they have no conflict of interest.
Animal and/or human studies
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: In the original publication of the article the fourth author name was incorrectly published. The correct name is given in this correction.
Rights and permissions
About this article
Cite this article
Halim, I.A., Park, J.H., Liou, E.J.W. et al. Preliminary study: evaluating the reliability of CBCT images for tongue space measurements in the field of orthodontics. Oral Radiol 37, 256–266 (2021). https://doi.org/10.1007/s11282-020-00443-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11282-020-00443-0