Abstract
There is general consensus that enteroendocrine cells, EEC, containing the enteric hormone cholecystokinin (CCK) are confined to the small intestine and predominate in the duodenum and jejunum. Contrary to this, EEC that express the gene for CCK have been isolated from the large intestine of the mouse and there is evidence for EEC that contain CCK-like immunoreactivity in the mouse colon. However, the human and rat colons do not contain CCK cells. In the current study, we use immunohistochemistry to investigate CCK peptide presence in endocrine cells, PCR to identify cck transcripts and chromatography to identify CCK peptide forms in the mouse small and large intestine. The colocalisation of CCK and 5-HT, hormones that have been hypothesised to derive from cells of different lineages, was also investigated. CCK immunoreactivity was found in EEC throughout the mouse small and large intestine but positive cells were rare in the rectum. Immunoreactive EEC were as common in the caecum and proximal colon as they were in the duodenum and jejunum. CCK gene transcripts were found in the mucosa throughout the intestine but mRNA for gastrin, a hormone that can bind some anti-CCK antibodies, was only found in the stomach and duodenum. Characterisation of CCK peptides of the colon by extraction, chromatographic separation and radioimmunoassay revealed bioactive amidated and sulphated forms, including CCK-8 and CCK-33. Moreover, CCK-containing EEC in the large intestine bound antibodies that target the biologically active sulfated form. Colocalisation of CCK and 5-HT occurred in a proportion of EEC throughout the small intestine and in the caecum but these hormones were not colocalised in the colon, where there was CCK and PYY colocalisation. It is concluded that authentic, biologically active, CCK occurs in EEC of the mouse large intestine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It has been widely reported and is supported in textbooks and reviews, that CCK-containing enteroendocrine cells (EEC) are restricted to the duodenum, jejunum and proximal ileum in the rat, human and other species (Larsson and Rehfeld 1978; Chao and Hellmich 2012; Gribble and Reimann 2015). In rat, the C-terminal tetrapeptide amide that is common to gastrin and CCK occurs in the ileum but no CCK immunoreactive EEC were found in the proximal part of the colon (Larsson and Rehfeld 1978). Moreover, biologically active CCK is absent from the rat distal colon, although small amounts of pro-CCK are detectable (Lüttichau et al. 1993). In human, CCK is prominent in the duodenum and jejunum but is absent from the colon (Rehfeld 1978; Maton et al. 1984; Martins et al. 2017). A need for further investigation in mouse is highlighted by the observations of Egerod et al. (2012), who used an eGFP reporter coupled to the Cck promotor to locate sites of Cck expression and found an unexpectedly large population of Cck-eGFP-positive EEC throughout the intestine including the colon. In a similar study, glucagon gene-expressing EEC from the mouse colon were shown to express Cck transcripts (Habib et al. 2012). However, these gene expression studies have not identified whether the cells that were identified produce a CCK peptide product. Earlier, using immunohistochemistry, Roth et al. (1992) reported CCK-like immunoreactivity in numerous EEC of the mouse proximal colon but the immunoreactive product was not identified. The Cck gene is translated to pre-pro-CCK. The post-translational processing of this precursor produces a range of peptides, including CC-58, 39, 33, 25, 18, 8, 7 and 5, which may be sulfated or non-sulfated, or amidated or not amidated (Rehfeld 1978; Reeve et al. 1986; Agersnap and Rehfeld 2015), depending on the post-translational machinery possessed by the cell (Rehfeld et al. 2008). Amidated CCK-8 sulfate is generally considered the biologically active form, the bioactive sequence being the heptapeptide sequence, −Tyr(SO4)-Met-Gly-Trp-Met-Asp-Phe-NH2 (Rehfeld et al. 2007).
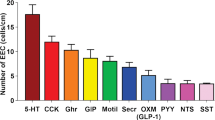
The well-established roles of CCK released from EEC are to facilitate digestion by stimulation of gallbladder contractions and pancreatic exocrine secretion and to signal satiety by activating vagal afferent fibres (Owyang 1996; Beglinger and Degen 2004). Each of these functions is associated with CCK released from EEC of the small intestine in response to nutrients, particularly fats and proteins. CCK is described in most text books as the only hormone expressed by I cells in duodenum and jejunum. It is now clear that this is not so and that Cck can be expressed with the genes for many other gut hormones, including secretin, glucose-dependent insulinotropic peptide (GIP), EEC peptides derived from preproglucagon, i.e., glucagon-like peptide-1 (GLP-1), GLP-2 and oxyntomodulin, neurotensin and peptide YY (PYY). In most cases, colocalisation of CCK and other gut hormones has been confirmed by double-labelling immunohistochemistry (Egerod et al. 2012; Habib et al. 2012; Sykaras et al. 2014).
These studies suggest that there is a major developmental lineage for enteroendocrine cells in the mouse that leads to cells that express CCK, GIP, GLP-1 and 2, PYY, neurotensin and secretin. It has been proposed that other, separate, lineages lead to (1) EEC that express 5-HT and substance P, (2) EEC that express ghrelin and in some species motilin and (3) EEC that express somatostatin (Roth et al. 1992). However, 5-HT and CCK, which are hypothesised to be in cells of different lineages, have been reported to be colocalised in the mouse small intestine (Cho et al. 2014; Reynaud et al. 2016). About 60% of the CCK cells were also 5-HT immunoreactive (Cho et al. 2014). In the mouse proximal colon, Roth et al. (1992) reported that fewer than 1% of 5-HT immunopositive cells contained CCK.
CCK is sulfated in its C-terminal, which is necessary for its biological activity in modifying digestive function and satiety but it also occurs as the non-sulfated peptide (Rehfeld et al. 2007; Agersnap and Rehfeld 2014). It also has similarity to gastrin, with which it shares a C-terminal pentapeptide amide (Larsson and Rehfeld 1977). Thus, depending on the antibodies used, CCK-like immunoreactivity could be due to the presence of non-sulfated CCK, gastrin or gastrin gene-derived peptides. In the present work, we use antibodies specific to the sulfated and non-sulfated forms of CCK to determine the localisation of CCK in EEC throughout the mouse gut. We investigate the expression of CCK and gastrin genes in the mucosa throughout the digestive tract and isolate and characterise immunoreactive CCK. We also investigate patterns of co-localisation of CCK with 5-HT throughout the intestines and with PYY in the colon.
Materials and methods
Animals and tissue preparation
Experiments were conducted according to the National Health and Medical Research Council of Australia guidelines and approved by the University of Melbourne Animal Experimentation Ethics Committee. Adult C57BL/6 male mice were housed in the Biomedical Animal Facility at the University of Melbourne and were provided standard chow and water ad libitum. Mice (8–10 weeks, 20–25 g) were anesthetised with isoflurane and then killed by cervical dislocation. Segments of gastric corpus and antrum, the descending part of the duodenum, the first 4 cm of the jejunum starting from the root of the mesentery, 4 cm of proximal ileum 4 cm away from the jejunum, 4 cm of distal ileum 2 cm away from the caecum, caecum, middle of the proximal colon, first and second half of the distal colon (called distal colon A and B, respectively) between the colonic flexure and the pelvic brim and the rectum within the pelvis were removed. For immunohistochemistry, the segments were opened along the mesenteric attachment, cleaned of contents and pinned unstretched, with mucosa up, to balsa wood sheets in ice-cold phosphate-buffered saline (PBS: 0.15 M NaCl in 0.01 M sodium phosphate buffered, pH 7.2). The tissue was then placed in fixative (2% formaldehyde plus 0.2% picric acid in 0.1 M sodium phosphate buffer, pH 7.2) overnight at 4 °C. The following day, the tissues were washed three times (10 min) with dimethyl sulfoxide (DMSO) and then three times (10 min) with PBS, then transferred to PBS-sucrose-azide (PBS containing 0.1% sodium azide and 30% sucrose as a cryoprotectant) and stored at 4 °C. The next day, the tissue samples were placed in 50% PBS-sucrose-azide and 50% OCT mixture (Tissue Tek, Elkhart, IN, USA) for a further 24 h, before being trimmed and embedded in 100% OCT and frozen in isopentane cooled with liquid nitrogen.
Immunohistochemistry
Sections of 12 μm thickness were cut, allowed to dry at room temperature for 1 h on microscope slides (SuperFrostPlus®; Menzel-Glaser; Thermo Fisher, Scoresby, Vic, Australia) and incubated with 10% normal horse serum for 30 min. Mixtures of primary antibodies (Table 1) for double staining were then added and sections were left at 4 °C overnight. The tissue was washed three times in PBS and incubated in secondary antibody (Table 2) for 1 h at room temperature. To stain the nuclei with Hoechst 33258 solution (Bisbenzimide–Blue, diluted to 10 μg/mL in dH2O), preparations were washed once with PBS then twice with distilled water and then incubated for 5 min with the stain. Sections were then washed three times with distilled water before mounting with non-fluorescent mounting medium (Dako, Carpinteria, CA, USA).
Image analysis
After staining, slides were kept overnight then examined using an AxioImager microscope (Zeiss, Sydney, Australia). For quantitation purposes, both a V-slide fluorescent slide scanner (Zeiss) and an LSM 800 confocal microscope with Airyscan (Zeiss) were used to capture images. These images were exported to be analysed off-line using ImageJ (imagej.nih.gov/ij/). Immunoreactive cells were quantified by counting around 100 cells from each part of the gut. A higher number was counted when needed statistically. This analysis was repeated in 3 animals. The Airyscan microscope was used to capture high-resolution images that were exported into CorelDraw (Corel, Ottowa, Canada) for final preparation of figures.
RNA isolation and Reverse Transcriptase-Polymerase Chain Reaction (RT-PCR)
Total RNA was isolated from freshly dissected mucosal scrapings of the mouse stomach, duodenum, jejunum, ileum, proximal colon, distal colon A, distal colon B and rectum from three mice using the RNeasy Mini Kit (Qiagen, Melbourne, Australia). One microgram of total RNA from each sample was reverse-transcribed using the iScript cDNA Synthesis Kit (Bio-Rad Laboratories, Gladesville, NSW, Australia) according to the manufacturer guidelines. cDNA was amplified by PCR using 5PRIME MasterMix (5PRIME, Hamburg, Germany) with appropriate intron-spanning primers. Forward and reverse PCR primer sequences were, respectively: for CCK, 5′-AGCGGCGTATGTCTGTGCGT-3′ and 5′-CACTGCGCCGGCCAAAATCC-3′ to produce a 316-bp product (Gonzalez-Coto et al. 2014); for gastrin, 5′-AGCTGACCCAGCGCCACAAC-3′ and 5′-ACTGCGGCGGCCAAAGTCCA-3′ to produce a 338-bp product (Gonzalez-Coto et al. 2014); and for β-actin (which was used as a control for cDNA quality), 5′-GCTCGTCGTCGACAACGGCT C-3′ and 5′-CAAACATGATCTGGGTCATCTTCTC-3′ to produce a 353-bp product. The CCK and gastrin primers were from Invitrogen (Australia) and the β-actin primers were provided with the Superscript III First-Strand Synthesis System for RT-PCR (Invitrogen). All amplifications were performed with an initial step at 94 °C for 2 min, followed by 35 cycles of denaturation at 94 °C for 30 s, annealing at 61 °C for 30 s, extension at 72 °C, with a final extension at 72 °C for 5 min. Reactions were also conducted without reverse transcriptase to confirm the absence of genomic DNA. Amplification products were visualised by electrophoresis on a 1.5% agarose gel containing SYBR Safe DNA Gel Stain (Thermo-Fisher Scientific, Australia). The gels were imaged with the Gel Doc EZ Gel Documentation System (Bio-Rad Laboratories). The PCR gene product for CCK was sequenced at the Centre for Translational Pathology (Department of Pathology, The University of Melbourne, Australia).
Extraction and chromatographic characterisation of CCK
The jejunum and distal colon were taken from six male C57BL/6 mice for extraction and characterisation of CCK immunoreactive peptides. The distal colon was chosen, rather than the proximal colon, because faeces are more readily removed from the distal colon. The mucosa was immediately stripped free from the intestinal wall and specimens were frozen on dry ice and stored at −80 °C. Samples were immersed in liquid nitrogen and pulverised by a cryoPREP impactor. Pulverised samples were boiled for 20 min in 10 mL/g distilled water and homogenised. The extracts were centrifuged at 10,000 rpm and the supernatant was collected as the “neutral extract”. The pellet was then resuspended in 0.5 M acetic acid (10 mL/g), homogenised and incubated for 20 min at room temperature. It was then centrifuged at 10,000 rpm for 30 min at 4 °C and the supernatant was collected as the “acid extract”.
The CCK peptides in the extracts were measured using two sequence-specific assays as previously detailed (Agersnap and Rehfeld 2015). CCK-antiserum # 92128 (Table 1) binds the α-amidated C-terminus of only sulfated CCK peptides. This antiserum does not react with either sulfated or non-sulfated gastrins. CCK-antiserum # 94179 was used to detect non-sulfated CCK. It binds the N-terminal pentapeptide sequence of nonsulfated CCK-8.
The tissue extracts were applied to Sephadex G50 superfine columns to separate the molecular forms of CCK according to size. The samples were applied to calibrated columns and eluted with 0.02 mol/L barbital buffer, pH 8.4, containing 1 g/L bovine albumin and 0.1 M NaCl at a flow rate of 4 mL/h. The fractions were collected and the concentration of CCK measured by radioimmunoassay. The total concentration of sulfated and non-sulfated CCK in each tissue was measured by RIA in each of the neutral and acidic extracts separately. AUC calculations were performed on chromatograms for sulfated and non-sulfated CCKs, respectively, based on the known elution of the individual CCK forms in the calibrated columns. The estimation of the concentration of each molecular form was performed for the neutral and acidic extracts separately.
Statistical analysis
Prism 5.0 (GraphPad Software, San Diego, CA, USA) was used to analyse data and present it as mean ± SEM. Differences were evaluated with 2-tailed Student’s t tests and by ANOVA.
Results
The immunohistochemical localisation of CCK was investigated throughout the intestinal tract from the duodenum to the rectum (Fig. 1), using an anti-CCK antibody, R183B, which recognises both CCK and gastrin (Cho et al. 2014). We also used two peptide specific antibodies, #92128 (Rehfeld 1998) that recognises sulfated CCK but not gastrin and # 94179 (Agersnap and Rehfeld 2014) that recognises the non-sulfated form of CCK. The distributions of CCK-immunoreactive cells observed with anti-CCK R183B and anti-sulfated CCK antibodies (#92128) were virtually the same; this is shown quantitatively for the large intestine in Fig. 2. An antibody against the non-sulfated form of CCK (# 94179) did not reveal EEC in the large intestine. Scattered cells that were immunoreactive for non-sulfated CCK cells were observed in the duodenum and jejunum.
Distribution of CCK immunoreactive enteroendocrine cells, per mm2 of mucosa, along the mouse small and large intestines. Duod duodenum, Jej jejunum, P il proximal ileum, D il distal ileum, Cec caecum, PC proximal colon, DC(A) the first half of the distal colon, DC (B) the second half of the distal colon, Rect rectum
In the small intestine, the numbers of EEC that expressed CCK (revealed by antibody R183B) increased from 19.9 ± 3.1 cells/mm2 in the duodenum to 39.1 ± 5.7 cells/mm2 in the proximal ileum, (n = 3 mice) then decreased starting in the distal ileum (26.5 ± 4.3 cells/mm2, n = 3 mice). The cell numbers in both the duodenum and jejunum were significantly different to the numbers in the proximal ileum (P < 0.05). The decrease continued gradually in the large intestine to reach extremely rare cells in the rectum (14.1 ± 2.3 cells/mm2 in proximal colon to 3.1 ± 0.6 cells/mm2 in distal colon A, n = 3 mice). The decrease along the large intestine was significant (one-way ANOVA, P < 0.05).
Colocalisation of CCK and 5-HT in the small and large intestine
Investigation of the colocalisation of CCK and 5-HT showed colocalisation throughout the small intestine and in the caecum. The greatest proportion of CCK cells that also contained 5-HT was in the caecum (75% of CCK cells in the caecum coexpressed 5-HT), while in the proximal ileum, where the greatest number of CCK immunoreactive EEC were found, 40% of CCK cells expressed 5-HT. EEC that contained both CCK and 5-HT were not found in the colon, although cells with each hormone alone were found (Figs. 3 and 4).
Double staining for CCK and 5-HT. Examples of EEC in which CCK and 5-HT are separately expressed (EEC with arrows) and in which both hormones are expressed (EEC with asterisks). Each set of panels (a, a’, a”, etc.) show the same field with CCK, 5-HT and the merged images illustrated. Scale bar 10 μm
Colocalisation of CCK and PYY in the large intestine
As described above, in contrast to the small intestine and caecum, CCK and 5-HT are in separate EEC in the colon. The most numerous EEC type (other than 5-HT cells) in the mouse colon are PYY/GLP-1 cells (Cho et al. 2015). We therefore investigated the overlap between CCK and PYY immunoreactivity, which we chose to do in the proximal colon where CCK cells are numerous. In double-stained sections from the proximal colon, analysed in 3.2-μm Z-stacks from each of the 3 mice, about 65% of PYY cells were also immunoreactive for CCK (Fig. 5).
Colocalisation of CCK in PYY cells of the mouse proximal colon. Examples of cells in which PYY and CCK were colocalised (a, a’, a”) and in which only PYY was located (b, b’, b”) are illustrated. Scale bar 10 μm. About 65% of PYY containing EEC were also CCK immunoreactive (c). Data are mean ± SEM from three mice
CCK and gastrin mRNA expression, Cck and Gast, detected by RT-PCR
CCK mRNA was detected by RT-PCR using intron-spanning primers in mucosal extracts from the stomach, duodenum, jejunum, ileum, proximal colon, proximal region of the distal colon (distal colon part A), distal region of the distal colon (distal colon part B) and rectum (Fig. 6). Bands for Cck transcripts had the predicted molecular sizes of 316 bp as previously reported (Gonzalez-Coto et al. 2014). Cck expression was very weakly detected in the mucosal extract from 1 mouse stomach and was not detected in the other 2 mouse stomach samples. Bands were not observed in control reactions with the omission of reverse transcriptase and in the absence of template cDNA. The quality of RNA extracted was validated with the detection of β-actin in all mouse mucosal samples. RT-PCR Cck products were confirmed to have the correct structure by sequencing samples from the duodenum and distal colon part B.
Reverse transcriptase-polymerase chain reaction (RT-PCR) gel showing the predicted product size of 316 base-pairs (bp) of CCK in mucosal extracts from the mouse stomach, duodenum, jejunum, proximal colon, proximal region of the distal colon (distal colon part A), distal region of the distal colon (distal colon part B) and rectum (upper panel). The predicted product size of 338 base-pairs (bp) of gastrin occurred in extracts from stomach and duodenum but not other regions (lower panel). Results in the presence (+) and in the absence (−) of reverse transcriptase (RT) are shown. Duod duodenum, Jejun jejunum, P colon proximal colon, D col A distal colon part A, D col B distal colon part B, NTC no template control.
RT-PCR for the gastrin transcript was strong in the stomach and weak in the duodenum but was not detected in any other region, indicating that the EEC located in all regions, with the possible exception of the duodenum, expressed Cck, not Gast.
Characterisation of CCK forms
Bioactive (amidated and sulfated) CCK was found in both the colon and jejunal extracts but at lower concentrations in colon extracts, 2.9 ± 0.9 pmol/g, than in jejunal extracts, 55.9 ± 11.2 (n = 6; Table 3). This difference in concentration can be related in part to differences in cell numbers, 3.5 per mm2 in the mucosa of the distal colon compared to 20 per mm2 in the jejunal mucosa (Fig. 1). Non-amidated (gly-extended) CCK and pro-CCK were also found in both regions. Acid extracts from the colon revealed a major extended CCK, CCK-33, plus peaks corresponding to CCK-58 and CCK-12. Neutral extraction revealed that the dominant sulfated form was CCK-8 (Fig. 7). Chromatographic characterization of jejunal CCK revealed three major peaks, corresponding to CCK-33, CCK-22 and CCK-8 and a small amount of CCK-58.
Elution profile of CCK immunoreactive peptides (amidated and sulfated), extracted from the distal colon, after gel chromatographic separation, measured with the specific assay for amidated, sulfated CCK (using antibody #92128). a CCK in the acetic acid extracts. The first two peaks correspond to CCK-58 and -33 (the major peak). The third peak includes CCK-12. b CCK in the neutral tissue extract, which is mainly CCK-8 and perhaps a little CCK-12
Discussion
This study shows that CCK, revealed by two antisera, one of which is specific for sulfated CCK and the other having a broader binding characteristics, occurs in EEC throughout the mouse intestine, including the colon, where the literature suggests that CCK does not occur in mammals. Gene transcripts for CCK but not for gastrin, were found in the mucosa of the colon. Gastrin transcripts were only detectable in the stomach and, weakly, in the duodenum. Peptide extraction from the colon revealed the presence of CCK, primarily its sulfated form. This extracted CCK is deduced to come from EEC, as these are the only CCK-immunoreactive cell type in the colon; CCK-immunoreactive neurons and nerve fibres being absent in mature mouse small intestine and colon (Lay et al. 1999; Rehfeld et al. 2008; present study). The presence of CCK in colonic EEC in mouse is consistent with studies using a Cck-reporter mouse (Egerod et al. 2012) and contrasts with human, where CCK cells could not be found in the sigmoid colon (Martins et al. 2017) and adult rat, where CCK is also absent (Larsson and Rehfeld 1978; Lüttichau et al. 1993). There were no differences in the distributions in the mouse colon determined by the two antibodies that recognise sulfated CCK. Cells were not observed in the large intestine with an anti-non-sulfated CCK antibody (which did show a small number of EEC in the duodenum and jejunum). The results indicate that biologically active sulfated CCK occurs in mouse colonic EEC.
As noted in the “Introduction”, the well-established roles of CCK released from EEC are to facilitate nutrient digestion by contracting the gallbladder to release bile into the intestine, to stimulate the release of digestive enzymes from the pancreas and to signal satiety by activating vagal afferent fibres (Owyang 1996; Beglinger and Degen 2004). All these signals arise from the stimulation of receptors on EEC by nutrients in the luminal contents. The nutrient receptors on CCK-secreting cells in the small intestine include receptors for fats, amino acids and bitter compounds (Raybould 1999; Chen et al. 2006; Edfalk et al. 2008; Wang et al. 2011; Daly et al. 2013). The highest abundance of intestinal CCK cells was in the mouse ileum (Fig. 1). CCK released from this part of the intestine may signal satiety in response to nutrients that are not digested and absorbed in the duodenum or jejunum.
The colocalisation of 5-HT in a proportion of CCK cells in the small intestine suggests that the two hormones may interact in signalling from this region. 5-HT and CCK have synergistic effects to increase pancreatic enzyme secretion, a function that is linked to release of CCK from the proximal small intestine (Owyang 1996). In conscious rats, nutrient infusion into the small intestine elicited increases in pancreatic enzyme secretion that were reduced by 54% when CCK receptors were blocked and 92% when both CCK and 5-HT receptors were blocked (Li et al. 2000). CCK and 5-HT also act synergistically to suppress food intake (Voigt et al. 1995; Hayes and Covasa 2005). The CCK-mediated satiety effect is caused by nutrients stimulating CCK release from EEC in the proximal small intestine and CCK activating vagal afferent nerve endings (Raybould 2007). Thus, it is relevant that combined CCK and 5-HT receptor block causes a greater reversal of suppression of eating in response to intraduodenal nutrient than either antagonist alone (Savastano and Covasa 2007). 5-HT and CCK may also have synergistic actions in the control of segmentation in the small intestine (Ellis et al. 2013). These authors found that segmentation that was elicited by fat in the lumen fat was mimicked by inhibiting 5-HT uptake (thus increasing 5-HT levels) and also by CCK. Furthermore, the increase in segmentation caused by fat was inhibited by both CCK and 5-HT receptor antagonism.
In the large intestine, we found that a high proportion of PYY cells also contained CCK, whereas 5-HT cells were not CCK immunoreactive, consistent with earlier observations (Roth et al. 1992). There may be a synergism between CCK and PYY released from the colon, both being satiety factors. PYY is released when short chain fatty acids, oleic acid, glucose or an amino acid mix are instilled into the colon of the rat (Fu-Cheng et al. 1995). In humans, intrarectal administration of sodium acetate but not intravenous acetate, caused a significant increase in plasma PYY (Freeland and Wolever 2010), while in mouse, intracolonic propionate also caused PYY release (Psichas et al. 2015). A link between release of PYY from colonic EEC and satiety has been demonstrated in humans (Chambers et al. 2015). These authors utilised an inulin-propionate ester to deliver propionate to the colon of human volunteers. Studies of inulin-propionate ester metabolism and plasma propionate after a meal indicated effective delivery to the colon. Inulin-propionate released PYY, whose concentration in plasma was increased 6 fold, 60 min after the propionate was estimated to reach the colon. Acute administration of inulin-propionate reduced appetite and inclusion of 10 g/day in food for 24 days significantly reduced weight gain (Chambers et al. 2015). Thus, the literature suggests that CCK and PYY released from colonic EEC in mouse may have synergistic effects on food intake but this has yet to be tested experimentally. It is also possible that they interact to affect local colonic functions, such as contractions of smooth muscle or epithelial water and electrolyte transport. For example, CCK affects smooth muscle of the colon, contracting the circular muscle in the cat (Mangel 1984) and dog (Huizinga et al. 1984) and relaxing it in the rat (Kishimoto et al. 1994). PYY decreases water and electrolyte transport in the mouse and human colon (Cox and Tough 2002; Tough et al. 2011) but the effects of CCK do not appear to have been investigated. Actions of CCK released from colonic EEC to control the gall-bladder or pancreatic function do not have apparent physiological rationales. Clearly, further research is required to deduce the range of possible roles of CCK produced by EEC in the large intestine of mouse.
This study adds to the evidence that the distributions and chemical attributes of EEC differ considerably between species. Other examples are the presence of motilin in EEC and its physiological roles in human, rabbit, dog and pig and its absence from rat, mouse and guinea-pig (Smith et al. 1981; Itoh 1997; Sanger and Furness 2016) and the prominence of PYY containing EEC in the duodenum of pig and its absence or rarity in the duodenum of other species (Cho et al. 2015).
In conclusion, we demonstrated that a subpopulation of colonic EEC in mouse synthesise and store CCK in a biologically active form. In the small intestine, there is colocalisation of 5-HT in a proportion of CCK cells but this does not occur in the colon. In the proximal colon, about 65% of PYY cells contain CCK. It is concluded that CCK cells of different regions may have different functions and that in the colon PYY and CCK may synergise to regulate food intake.
References
Agersnap M, Rehfeld JF (2014) Measurement of nonsulfated cholecystokinins. Scand J Clin Lab Invest 74:424–431
Agersnap M, Rehfeld JF (2015) Nonsulfated cholecystokinins in the small intestine of pigs and rats. Peptides 71:121–127
Beglinger C, Degen L (2004) Fat in the intestine as a regulator of appetite - role of CCK. Physiol Behav 83:617–621
Chambers ES, Viardot A, Psichas A et al (2015) Effects of targeted delivery of propionate to the human colon on appetite regulation, body weight maintenance and adiposity in overweight adults. Gut 64:1744–1174
Chao C, Hellmich MR (2012) Gastrointestinal hormones: gastrin, cholecystokinin, somatostatin and ghrelin. In: Johnson LR (ed) Physiology of the gastrointestinal tract. Academic, London
Chen MC, Wu SV, Reeve JR Jr, Rozengurt E (2006) Bitter stimuli induce Ca2+ signaling and CCK release in enteroendocrine STC-1 cells: role of L-type voltage-sensitive Ca2+ channels. Am J Physiol Cell Physiol 291:C726–C739
Cho H-J, Callaghan B, Bron R, Bravo DM, Furness JB (2014) Identification of enteroendocrine cells that express TRPA1 channels in the mouse intestine. Cell Tissue Res 356:77–82
Cho H-J, Kosari S, Hunne B, Callaghan B, Rivera LR, Bravo DM, Furness JB (2015) Differences in hormone localisation patterns of K and L type enteroendocrine cells in the mouse and pig small intestine and colon. Cell Tissue Res 359:693–698
Cox HM, Tough IR (2002) Neuropeptide Y, Y1, Y2 and Y4 receptors mediate Y agonist responses in isolated human colon mucosa. Br J Pharmacol 135:1505–1512
Daly K, Al-Rammahi M, Moran A, Marcello M, Niomiya Y, Shirazi-Beechey SP (2013) Sensing of amino acids by the gut-expressed taste receptor T1R1-T1R3 stimulates CCK secretion. Am J Physiol Gastrointest Liver Physiol 304:G271–G282
Edfalk S, Steneberg P, Edlund H (2008) Gpr40 is expressed in enteroendocrine cells and mediates free fatty acid stimulation of incretin secretion. Diabetes 57:2280–2287
Egerod KL, Engelstoft MS, Grunddal KV et al (2012) A major lineage of enteroendocrine cells coexpress CCK, secretin, GIP, GLP-1, PYY, and neurotensin but not somatostatin. Endocrinology 153:5782–5795
Ellis M, Chambers JD, Gwynne RM, Bornstein JC (2013) Serotonin and cholecystokinin mediate nutrient-induced segmentation in guinea pig small intestine. Am J Physiol Gastrointest Liver Physiol 304:G749–G761
Freeland KR, Wolever TMS (2010) Acute effects of intravenous and rectal acetate on glucagon-like peptide-1, peptide YY, ghrelin, adiponectin and tumour necrosis factor-α. Br J Nutr 103:460–466
Fu-Cheng X, Anini Y, Chariot J, Voisin T, Galmiche J-P, Rozé C (1995) Peptide YY release after intraduodenal, intraileal, and intracolonic administration of nutrients in rats. Eur J Physiol 431:66–75
Gonzalez-Coto AF, Alonso-Ron C, Alcalde I, Gallar J, Meana A, Merayo-Lloves J, Belmonte C (2014) Expression of cholecystokinin, gastrin, and their receptors in the mouse cornea. Invest Ophthalmol Vis Sci 55:1965–1975
Gribble FM, Reimann F (2015) Enteroendocrine cells: chemosensors in the intestinal epithelium. Annu Rev Physiol 78:3.1–3.23
Habib AM, Richards P, Cairns LS, Rogers GJ, Bannon CAM, Parker HE, Morley TCE, Yeo GSH, Reimann F, Gribble FM (2012) Overlap of endocrine hormone expression in the mouse intestine revealed by transcriptional profiling and flow cytometry. Endocrinology 153:3054–3065
Hayes MR, Covasa M (2005) CCK and 5-HT act synergistically to suppress food intake through simultaneous activation of CCK-1 and 5-HT3 receptors. Peptides 26:2322–2330
Huizinga JD, Chang G, Diamant NE, El Sharkawy TY (1984) The effects of cholecystokinin-octapeptide and pentagastrin on electrical and motor activities of canine circular muscle. Can J Physiol Pharmacol 62:1440–1447
Itoh Z (1997) Motilin and clinical application. Peptides 18:593–608
Kishimoto S, Machino H, Kobayashi H, Haruma K, Kajiyama G, Miyoshi A, Fuji K (1994) Inhibitory action of CCK-OP on rat proximal colon. Ann N Y Acad Sci 713:407–409
Larsson L-I, Rehfeld JF (1977) Evidence for a common evolutionary origin of gastrin and cholecystokinin. Nature 269:335–338
Larsson L-I, Rehfeld JF (1978) Distribution of gastrin and CCK cells in the rat gastrointestinal tract evidence for the occurrence of three distinct cell types storing COOH-terminal gastrin immunoreactivity. Histochemistry 58:23–31
Lay JM, Gillespie PJ, Samuelson LC (1999) Murine prenatal expression of cholecystokinin in neural crest, enteric neurons, and enteroendocrine cells. Dev Dyn 216:190–200
Li Y, Hao Y, Zhu J, Owyang C (2000) Serotonin released from intestinal enterochromaffin cells mediates luminal non-cholecystokinin-stimulated pancreatic secretion in rats. Gastroenterology 118:1197–1207
Lüttichau HR, Solinge WWV, Nielsen FC, Rehfeld JF (1993) Developmental expression of the gastrin and cholecystokinin genes in rat colon. Gastroenterology 104:1092–1098
Mangel AW (1984) Potentiation of colonic contractility to cholecystokinin and other peptides. Eur J Pharmacol 100:285–290
Martins P, Fakhry J, Chaves de Oliveira E, Hunne B, Fothergill LJ, Ringuet M, d’Ávila Reis D, Rehfeld JF, Callaghan B, Furness JB (2017) Analysis of eneteroendocrine cell populations in the human colon. Cell Tissue Res 367:361–368
Maton PN, Selden AC, Chadwick VS (1984) Differential distribution of molecular forms of cholecystokinin in human and porcine small intestinal mucosa. Regul Pept 8:9–19
Owyang C (1996) Physiological mechanisms of cholecystokinin action on pancreatic secretion. Am J Physiol 271:G1–G7
Psichas A, Sleeth ML, Murphy KG, Brooks L, Bewick GA, Hanyaloglu AC, Ghatei MA, Bloom SR, Frost G (2015) The short chain fatty acid propionate stimulates GLP-1 and PYY secretion via free fatty acid receptor 2 in rodents. Int J Obes 39:424–429
Raybould HE (1999) Nutrient tasting and signaling mechanisms in the gut I. Sensing of lipid by the intestinal mucosa. Am J Physiol 277:G751–G755
Raybould HE (2007) Mechanisms of CCK signaling from gut to brain. Curr Opin Pharmacol 7:570–574
Reeve JR, Eysselein V, Walsh, JH, Ben-Avram CM, Shively JE (1986) New molecular forms of cholecystokinin J. Biol. Chem. 261:16392–16397
Rehfeld JF (1978) Immunochemical studies on cholecystokinin. II. Distribution and molecular heterogeneity in the central nervous system and small intestine of man and hog. J Biol Chem 253:4022–4030
Rehfeld JF (1998) Accurate measurement of cholecystokinin in plasma. Clin Chem 44:991–1001
Rehfeld JF, Friis-Hansen L, Goetze JP, Hansen TVO (2007) The biology of cholecystokinin and gastrin peptides. Curr Top Med Chem 7:1154–1165
Rehfeld JF, Bundgaard JR, Hannibal J, Zhu X, Norrbom C, Steiner DF, Friis-Hansen L (2008) The cell-specific pattern of cholecystokinin peptides in endocrine cells versus neurons is governed by the expression of prohormone convertases 1/3, 2, and 5/6. Endocrinology 149:1600–1608
Reynaud Y, Fakhry J, Fothergill L, Callaghan B, Ringuet MT, Hunne B, Bravo DM, Furness JB (2016) The chemical coding of 5-hydroxytryptamine containing enteroendocrine cells in the mouse gastrointestinal tract. Cell Tissue Res 364:489–497
Roth KA, Kim S, Gordon JI (1992) Immunocytochemical studies suggest two pathways for enteroendocrine cell differentiation in the colon. Am J Physiol Gastrointest Liver Physiol 263:G174–G180
Sanger GJ, Furness JB (2016) Ghrelin and motilin receptors as drug targets for gastrointestinal disorders. Nat Rev Gastroenterol Hepatol 19:38–48
Savastano DM, Covasa M (2007) Intestinal nutrients elicit satiation through concomitant activation of CCK1 and 5-HT3 receptors. Physiol Behav 92:434–442
Smith PH, Davis BJ, Seino Y, Yanaihara N (1981) Localization of motilin-containing cells in the intestinal tract of mammals: a further comparison using region-specific motilin antisera. Gen Comp Endocrinol 44:288–291
Sykaras AG, Demenis C, Cheng L, Pisitkun T, Mclaughlin JT, Fenton RA, Smith CP (2014) Duodenal CCK cells from male mice express multiple hormones including ghrelin. Endocrinology 155:3339–3351
Tough IR, Forbes S, Tolhurst R, Ellis M, Herzog H, Bornstein JC, Cox HM (2011) Endogenous peptide YY and neuropeptide Y inhibit colonic ion transport, contractility and transit differentially via Y1 and Y2 receptors. Br J Pharmacol 164:471–484
Voigt J-P, Fink H, Marsden CA (1995) Evidence for the involvement of the 5-HT1A receptor in CCK induced satiety in rats. Naunyn Schmiedeberg’s Arch Pharmacol 351:217–220
Wang Y, Chandra R, Samasa LA, Gooch B, Fee BE, Cook JM, Vigna SR, Grant AO, Liddle RA (2011) Amino acids stimulate cholecystokinin release through the Ca2+-sensing receptor. Am J Physiol Gastrointest Liver Physiol 300:G528–G537
Acknowledgements
We thank Chelsea Dumensy for assistance with CCK characterisation and Mitchell Ringuet for assistance with the preparation of the paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
Brid Callaghan and John B Furness are equal senior authors
Rights and permissions
About this article
Cite this article
Fakhry, J., Wang, J., Martins, P. et al. Distribution and characterisation of CCK containing enteroendocrine cells of the mouse small and large intestine. Cell Tissue Res 369, 245–253 (2017). https://doi.org/10.1007/s00441-017-2612-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-017-2612-1