Abstract
Purpose
Here, we re-checked the American Joint Committee on Cancer 7th edition subclassification and confirmed the possibility of percent tumor volume as a prognostic factor for biochemical recurrence in the 8th edition subclassification.
Methods
A total of 1073 patients with pathologic T2 stage disease who underwent radical prostatectomy were included. Exclusion criteria were neoadjuvant therapy and pathologic T3 and N1 disease. Biochemical recurrence-free survival was estimated using the Kaplan–Meier method. Cox hazard regression was used to predict biochemical recurrence.
Results
According to the 7th edition subclassification, 141 patients (13.1%) had T2a, 43 (4.0%) had T2b, and 889 (82.9%) had T2c disease. The 7th edition subclassification did not differ significantly on Kaplan–Meier analysis (p = 0.502). Mean percent tumor volume was 8.7 ± 8.0% (interquartile range, 5–10%). Percent tumor volume was positively correlated with initial prostate-specific antigen, grade group, surgical margin, and T2 subclassification (all p < 0.001). The 7th edition subclassification was not a significant factor, whereas percent tumor volume was (hazard ratio, 1.023; 95% confidence interval, 1.005–1.041; p = 0.0128) on multivariate analysis. On Kaplan–Meier analysis, percent tumor volume (> 7.5% vs ≤ 7.5%) differed significantly for biochemical recurrence-free survival (p < 0.001).
Conclusions
The 7th edition pathologic T2 subclassification had poor prognostic value for biochemical recurrence in our cohort. Elimination of the 8th edition subclassification was suitable. Percent tumor volume classified biochemical recurrence prognosis in pathologic T2 stage. Therefore, percent tumor volume can be a candidate factor for the next T2 subclassification.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tumor staging is important to predicting prognosis and planning proper treatment. American Joint Committee on Cancer (AJCC) staging is the most commonly used system for classifying prostate cancer. The AJCC 8th subclassification was published in 2017 and implemented in January 2018 (Buyyounouski et al. 2017). The major changes from the 7th to 8th edition subclassifications were elimination of the pathologic T2 subclassification, inclusion of grade group, and incorporation of serum prostate-specific antigen (PSA) level ≥ 20 ng/mL and grade group 5 into stage III (Buyyounouski et al. 2017). Among these changes, pathologic T2 subclassification had caused controversy because of poor reproducibility and wide variation (Kwast et al. 2011). Therefore, the T2 subclassification of the AJCC 7th subclassification has been merged into one T2 classification in the AJCC 8th subclassification, which has been used to determine personalized staging (Amin et al. 2017). However, to obtain a more personalized staging in organ-confined prostate cancer patients, a newer system is needed.
One alternative method can be to classify T2 stage according to tumor burden. The prognostic value of tumor volume has been determined for other localized cancers such as hepatocellular carcinoma or breast cancer (Fehrenbacher et al. 2014; Nault et al. 2016). In metastatic prostate cancer, patients with low volume had better survival than those with high volume (James et al. 2016). In localized prostate cancer, Gleason score, serum PSA, and surgical margin were well-known predictive factors for biochemical recurrence (BCR) (Zhao et al. 2008). Surgical margin can be related to both surgical technique and tumor characteristics including tumor volume (Ohori et al. 1995). Percent tumor volume was associated with pathologic T stage, Gleason score, and surgical margin (Ku et al. 2011). For the first time, Stamey et al reported that cancer volume was an independent factor for BCR after adjusting for PSA level and Gleason grade (Stamey et al. 1999). However, in the era of the AJCC 7th edition, the effect of percent tumor volume on prognosis was controversial (Meng et al. 2015). The T2 subclassification for prognosis may also be limited because of the multifocality of prostate cancer. Therefore, we sought to re-check the AJCC 7th edition subclassification in our cohort and confirm the possibility of percent tumor volume as a prognostic factor for BCR in the AJCC 8th edition subclassification.
Materials and methods
This study protocol was approved by our institution’s ethical review board. We retrospectively reviewed the data of 1073 patients who underwent radical prostatectomy for prostate cancer between May 2012 and June 2017. Patients who were treated with neoadjuvant therapy and had pathologic T3 and N1 disease were excluded. Clinical data for age at diagnosis, initial PSA levels, operation type, biopsy grade group, clinical T stage, and pathological variables were collected. Patients were followed using serum PSA every 3–6 months for the first 2 years and annually thereafter. BCR was defined as a consecutively increasing PSA > 0.2 ng/mL twice. The follow-up period was 31.6 months (interquartile range 19.1–48.8 months).
The radical prostatectomy specimen was covered by India ink and fixed in 10% formalin. The specimen was cut at 3- to 5-mm intervals. After paraffin embedding and hematoxylin–eosin staining, the tissue was examined microscopically. The tumor’s contour was marked with a pen on the slide. The slide was overlaid with transparent paper, upon which prostate shape and tumor lesion were sketched. Percent tumor volume was calculated as the division of the sum of tumor lesions by the sum of prostate sections. Positive surgical margin was defined as cancer cells within the inked margin of the prostate. Patients were classified according to AJCC 7th edition T staging system subclassification (American College of Surgeons 2010).
The baseline clinicopathological characteristics of the patients and tumors are expressed as mean ± standard deviation or number and percentage. Continuous variables were compared using Student’s t test. Linear regression analysis was used to assess the relationships between initial PSA and percent tumor volume. Grade group was correlated with percent tumor volume by Spearman correlation analysis. Cox proportional hazard regression was used to analyze the prognostic factors for predicting BCR. Harrell’s concordance index (c-index) was used to evaluate model accuracy. A c-index of 1.0 means perfect predictive accuracy, while a c-index of 0.5 represents chance agreement. BCR-free survival was estimated using the Kaplan–Meier method with the log-rank test according to percent tumor volume stratified by given cutoff value. The cutoff value was estimated by the “maxstat” package for maximal separation of the Kaplan–Meier curve (Lausen and Schumacher 1992). All statistical analyses were performed with R (version 3.4.1; R Project for Statistical Computing, Vienna, Austria). P values < 0.05 were considered statistically significant.
Results
The clinicopathological characteristics of the 1073 patients are presented in Table 1. The mean age and initial PSA were 67.5 ± 7.0 years and 7.2 ± 9.8 ng/mL, respectively. Patients underwent radical prostatectomy using open (23.3%) or robotic (76.7%) techniques. Regarding clinical T stage, 141 (131%) were T3a and 21 (2.0%) were T3b, but in pathology, all were T2. According to the AJCC 7th edition subclassification, 141 (13.1%) were T2a, 43 (4.0%) were T2b, and 889 (82.9%) were T2c. Biopsy grade groups 4 and 5 comprised 13.5% and grade group 1 comprised 43.0%. Pathologic grade groups 4 and 5 comprised 5.6% and grade group 1 comprised 24.4%. The surgical margin was positive in 305 (28.4%). Mean prostate volume was 32.9 ± 15.9 cc. The percent tumor volume was 8.7 ± 8.0% (interquartile range 5–10%).
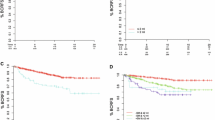
In the total cohort, BCR occurred in 108 patients (10.1%) after a median duration of 21.7 months. The 3-year BCR-free survival rate was 88.6%. According to AJCC 7th edition subclassification, there was no significant difference among T2 stage subclassifications (p = 0.502; Fig. 1). The estimated mean BCR-free survivals were 66.6 months [95% confidence interval (CI) 63.4–69.9] for T2a, 61.5 months (95% CI, 54.7–68.4) for T2b, and 68.7 months (95% CI, 67.1–70.4) for T2c. The 3-year BCR-free survival rates were 92.7% for T2a, 83.1% for T2b, and 88.3% for T2c.
Percent tumor volume was positively related to serum PSA level (p < 0.001; Fig. 2a) and grade group (p < 0.001; Fig. 2b). The mean percent tumor volume of T2a was lower than that of T2b (4.3% vs 6.6%, p < 0.001), while that of T2b was lower than that of T2c (6.6% vs 9.4%, p < 0.001; Fig. 2c). Positive surgical margin showed higher mean percent tumor volume than negative surgical margin (11.4% vs 7.5%, p < 0.001; Fig. 2d).
Percent tumor volume according to prostate-specific antigen (PSA), grade group, pathologic T stage subclassification, and surgical margin. a Percent tumor volume was positively correlated with initial PSA (p < 0.001). b Percent tumor volume was positively correlated with grade group (p < 0.001). c Percent tumor volume was significantly increased in T2b and T2c than T2a (each p < 0.001). d Percent tumor volume was significantly increased in positive surgical margins (p < 0.001)
In the multivariate Cox analysis (Table 2), pathologic grade group [2 vs 1: hazard ratio (HR), 2.384; 95% CI 1.055–5.387; p = 0.0367; 3 vs 1: HR, 4.474; 95% CI 1.958–10.225; p = 0.0004; 4 vs 1: HR, 11.816; 95% CI 4.716–29.602; p < 0.0001; 5 vs 1: HR 5.283; 95% CI 1.706–16.359; p = 0.0039] and positive surgical margin (HR 4.348; 95% CI 2.896–6.528; p < 0.0001) were significant factors for BCR. Although pathologic T stage (AJCC 7th edition subclassification) was not a significant factor, percent tumor volume was a significant factor (HR 1.023; 95% CI 1.005–1.041; p = 0.0128). The multivariate model that included percent tumor volume, pathologic grade group, and surgical margin had a c-index of 0.8012 (standard error, 0.0295).
The cutoff value for maximal separation of Kaplan–Meier curves was 7.5%. As shown in Fig. 3, percent tumor volume (> 7.5% vs ≤ 7.5%) showed a significant difference in BCR-free survival (p < 0.001). The estimated mean durations to BCR were 72.0 months (95% CI 70.5–73.5) for ≤ 7.5% tumor volume and 60.7 months (95% CI 58.2–63.1) for > 7.5% tumor volume. The 3-year BCR-free survival rates were 92.5% for the ≤ 7.5% group and 82.7% for the >7.5% group.
Discussion
We reconfirmed the poor ability of the AJCC 7th edition subclassification for predicting prognosis in our cohort. Elimination of the 8th edition subclassification was suitable. Multiple studies reported that the subclassification had little prognostic significance (DeCastro et al. 2008; Ettel et al. 2016; Kordan et al. 2009). Before the AJCC 7th edition was published in 2010, the AJCC adopted the T2 subclassification (T2a, half of a lobe or less; T2b, more than half of a lobe; T2c, both lobes) of the AJCC 4th edition in 1992. In 1997, the AJCC 5th edition made the change of unilateral lobe as T2a and bilateral lobes as T2b. The AJCC 6th edition in 2002 and 7th edition in 2010 used the 4th edition subclassification. During these changes, the subclassification of T2 was controversial; finally, the 8th edition removed the subclassification. The poor discrimination of the subclassification may result from the multifocal heterogeneity of prostate cancer (Andreoiu and Cheng 2010). More than 80% of prostate cancer cases had specimen multifocality (Andreoiu and Cheng 2010). In our study, T2c cases comprised 82.9%. By comparison, another reason can be the small proportion of T2b, only 4.0% of our cohort. The proportion of T2b was also low in other studies (DeCastro et al. 2008; Ettel et al. 2016; Kordan et al. 2009).
We suggest percent tumor volume as a criterion of T2 subclassification. In our study, percent tumor volume was related to the well-known prognostic factors of PSA, Gleason score, and surgical margin. In the multivariate analysis, percent tumor volume was an independent factor for BCR.
There are two main hypotheses to explain the multifocal heterogeneity of prostate cancer (Andreoiu and Cheng 2010). One is that initial tumor spread to other regions with allele loss (Cheng et al. 1998), and the other is that multiple precursor lesions form various tumors (Ruijter et al. 1996). Because Gleason pattern 3 may progress to Gleason pattern 4 with PTEN allelic loss (Sowalsky et al. 2013), Gleason score can be associated with the first hypothesis of multifocal heterogeneity. By comparison, percent tumor volume may support the second hypothesis. The carcinogenesis that occurs in various lesions can be merged or grow in place; consequentially, the progression of each tumor can be related to increasing tumor volume. Therefore, in the situation of early localized prostate cancer, tumor volume and Gleason score may act on the prognosis independently of each other. However, in cases of advanced prostate cancer, percent tumor volume may not be significant. You et al reported that percent tumor volume was not a significant factor for BCR in cases of pathologic stage T3 or T4 (You et al. 2014).
PSA is a very important biomarker for screening, risk classification, and follow-up in prostate cancer despite a lack of specificity (Rodriguez and Eggener 2018). Various risk classifications in localized prostate cancer have the criteria of PSA as 10 ng/mL for intermediate risk and 20 ng/mL for high risk (Faisal et al. 2014). In our cohort, patients with PSA > 10 ng/mL comprised only 14.2%, and the ratio of PSA could conceal the significance in the Cox analysis. However, the ratio of patients with a PSA > 10 ng/mL was similar with the data (13.3%) of the surveillance, epidemiology, and end results with T2 stage cohort (24,479 patients) (Izard et al. 2013). Another explanation may be that preoperative PSA of the gray zone had a limited relationship with cancer morphology because of relatively large individual variations (Stamey et al. 2002). Positive surgical margins can be affected by tumor volume and location, surgeon’s experience, and neurovascular bundle-sparing techniques (Izard et al. 2013). Therefore, we suggest the inclusion of percent tumor volume as the independent factor for BCR.
Some reports have claimed non-significance of percent tumor volume. Hansen et al reported that percent tumor volume did not predict early BCR within 2 years in high-risk prostate cancer patients (n = 595) (Hansen et al. 2014). However, their cohort included only 10% of specimen-confined prostate cancer. Wolters et al also reported that percent tumor volume was not a significant factor in multivariate analysis for BCR or cancer-specific survival in pathologic stage T2 (Wolters et al. 2010). However, the sub-cohort of pathologic stage T2 consisted of only 262 patients, and all data were collected by screening; thus, they would have lead time bias. In addition, over the last decade, multiparametric magnetic resonance imaging (mpMRI) has become an essential part of prostate cancer management. The index tumor volume calculated from mpMRI was associated with adverse pathology (Sugano et al. 2019).
Our study has some limitations. Percent tumor volume was assessed visually. Visual estimation could be subjective and show different interobserver agreements. Therefore, the cutoff value that we suggested could not be exact, and we showed the tendency of percent tumor volume for BCR. The planimetry method performed using a computer could be more exact for small tumor volume with poor visibility (Thompson et al. 2011). However, the technique requires additional software and more effort. Visual estimation showed a strong positive correlation with the computer-assisted method (Humphrey and Vollmer 1997). Therefore, a uniform method for reproducibility should be agreed in the field of pathology. In addition, BCR and survival data can be a good outcome to validate stage. There were few cases of mortality during our observation, so we just used BCR, which occurred at a frequency of 10.1% after radical prostatectomy. Further follow-up will give us additional data regarding survival.
Conclusions
We confirmed that the pathologic T2 subclassification of the AJCC 7th edition had poor prognostic value for BCR in our cohort. Thus, elimination of the subclassification in the AJCC 8th edition was deemed suitable. Additionally, to offer more personalized information for localized prostate cancer patients, a new subclassification is necessary. Percent tumor volume classified the prognosis of BCR in pathologic stage T2. Therefore, percent tumor volume can be a candidate for the next T2 subclassification.
References
American College of Surgeons (2017) AJCC cancer staging handbook: from the AJCC cancer staging manual, 7th edn. Springer, New York
Amin MB et al (2017) The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more "personalized" approach to cancer staging. CA Cancer J Clin 67:93–99. https://doi.org/10.3322/caac.21388
Andreoiu M, Cheng L (2010) Multifocal prostate cancer: biologic, prognostic, and therapeutic implications. Hum Pathol 41:781–793. https://doi.org/10.1016/j.humpath.2010.02.011
Buyyounouski MK et al (2017) Prostate cancer: major changes in the American joint committee on cancer eighth edition cancer staging manual. CA Cancer J Clin 67:245–253. https://doi.org/10.3322/caac.21391
Cheng L et al (1998) Evidence of independent origin of multiple tumors from patients with prostate cancer. J Natl Cancer Inst 90:233–237
DeCastro GJ, McCann T, Benson MC, McKiernan JM (2008) Pathologic T2 stage subgroups and recurrence-free survival after radical prostatectomy. Urology 72:1214–1218. https://doi.org/10.1016/j.urology.2008.01.054
Ettel M, Kong M, Lee P, Zhou M, Melamed J, Deng FM (2016) Modification of the pT2 substage classification in prostate adenocarcinoma. Hum Pathol 56:57–63. https://doi.org/10.1016/j.humpath.2016.05.016
Faisal FA et al (2014) Outcomes of men with an elevated prostate-specific antigen (PSA) level as their sole preoperative intermediate- or high-risk feature. BJU Int 114:E120–E129. https://doi.org/10.1111/bju.12771
Fehrenbacher L, Capra AM, Quesenberry CP Jr, Fulton R, Shiraz P, Habel LA (2014) Distant invasive breast cancer recurrence risk in human epidermal growth factor receptor 2-positive T1a and T1b node-negative localized breast cancer diagnosed from 2000 to 2006: a cohort from an integrated health care delivery system. J Clin Oncol 32:2151–2158. https://doi.org/10.1200/JCO.2013.52.0858
Hansen J et al (2014) Percentage of high-grade tumour volume does not meaningfully improve prediction of early biochemical recurrence after radical prostatectomy compared with Gleason score. BJU Int 113:399–407. https://doi.org/10.1111/bju.12424
Humphrey PA, Vollmer RT (1997) Percentage carcinoma as a measure of prostatic tumor size in radical prostatectomy tissues. Mod Pathol 10:326–333
Izard JP, Salazar MA, Chatterjee S, Lin DW, Wright JL (2013) Positive surgical margins at radical prostatectomy: Population-based averages within PSA and Gleason strata. Can Urol Assoc J 7:E561–566. https://doi.org/10.5489/cuaj.315
James ND et al (2016) Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet 387:1163–1177. https://doi.org/10.1016/S0140-6736(15)01037-5
Kordan Y et al (2009) Pathological stage T2 subgroups to predict biochemical recurrence after prostatectomy. J Urol 182:2291–2295. https://doi.org/10.1016/j.juro.2009.07.020
Ku JH, Moon KC, Kwak C, Kim HH (2011) Significance of predicted tumor volume as a predictor of pathologic stage in patients undergoing radical prostatectomy. Korean J Urol 52:24–30. https://doi.org/10.4111/kju.2011.52.1.24
Lausen B, Schumacher M (1992) Maximally selected rank statistics. Biometrics 48:73–85. https://doi.org/10.2307/2532740
Meng Y, Li H, Xu P, Wang J (2015) Do tumor volume, percent tumor volume predict biochemical recurrence after radical prostatectomy: a meta-analysis. Int J Clin Exp Med 8:22319–22327
Nault JC et al (2016) Percutaneous treatment of localized infiltrative hepatocellular carcinoma developing on cirrhosis. Ann Surg Oncol 23:1906–1915. https://doi.org/10.1245/s10434-015-5064-4
Ohori M, Wheeler TM, Kattan MW, Goto Y, Scardino PT (1995) Prognostic significance of positive surgical margins in radical prostatectomy specimens. J Urol 154:1818–1824
Rodriguez JF, Eggener SE (2018) Prostate cancer and the evolving role of biomarkers in screening and diagnosis. Radiol Clin North Am 56:187–196. https://doi.org/10.1016/j.rcl.2017.10.002
Ruijter ET, van de Kaa CA, Schalken JA, Debruyne FM, Ruiter DJ (1996) Histological grade heterogeneity in multifocal prostate cancer: biological and clinical implications. J Pathol 180:295–299. https://doi.org/10.1002/(SICI)1096-9896(199611)180:3%3c295:AID-PATH663%3e3.0.CO;2-W
Sowalsky AG, Ye H, Bubley GJ, Balk SP (2013) Clonal progression of prostate cancers from Gleason grade 3 to grade 4. Cancer Res 73:1050–1055. https://doi.org/10.1158/0008-5472.CAN-12-2799
Stamey TA, McNeal JE, Yemoto CM, Sigal BM, Johnstone IM (1999) Biological determinants of cancer progression in men with prostate cancer. JAMA 281:1395–1400
Stamey TA, Johnstone IM, McNeal JE, Lu AY, Yemoto CM (2002) Preoperative serum prostate specific antigen levels between 2 and 22 ng./ml. correlate poorly with post-radical prostatectomy cancer morphology: prostate specific antigen cure rates appear constant between 2 and 9 ng./ml. J Urol 167:103–111
Sugano D et al (2019) Index tumor volume on MRI as a predictor of clinical and pathologic outcomes following radical prostatectomy. Int Urol Nephrol 51:1349–1355. https://doi.org/10.1007/s11255-019-02168-4
Thompson IM 3rd et al (2011) Tumor volume as a predictor of adverse pathologic features and biochemical recurrence (BCR) in radical prostatectomy specimens: a tale of two methods. World J Urol 29:15–20. https://doi.org/10.1007/s00345-010-0611-x
van der Kwast TH et al (2011) International society of urological pathology (ISUP) consensus conference on handling and staging of radical prostatectomy specimens. working group 2: T2 substaging and prostate cancer volume. Mod Pathol 24:16–25. https://doi.org/10.1038/modpathol.2010.156
Wolters T et al (2010) Should pathologists routinely report prostate tumour volume: the prognostic value of tumour volume in prostate cancer. Eur Urol 57:821–829. https://doi.org/10.1016/j.eururo.2009.07.027
You D, Jeong IG, Song C, Cho YM, Hong JH, Kim CS, Ahn H (2014) High percent tumor volume predicts biochemical recurrence after radical prostatectomy in pathological stage T3a prostate cancer with a negative surgical margin. Int J Urol 21:484–489. https://doi.org/10.1111/iju.12348
Zhao KH, Hernandez DJ, Han M, Humphreys EB, Mangold LA, Partin AW (2008) External validation of University of California, San Francisco, cancer of the prostate risk assessment score. Urology 72:396–400. https://doi.org/10.1016/j.urology.2007.11.165
Funding
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2019R1C1C1005170) and Korea Health Technology R&D Project, the Korea Health Industry Development Institute (H16C2193).
Author information
Authors and Affiliations
Contributions
Study conception and design: SYC, CSK. Data acquisition: BHC, YSK, BL. Data analysis and interpretation: DY, IGJ, CS. Manuscript drafting: SYC. Critical manuscript revisions: JHH, HA. Funding sourcing: SYC, CSK. Supervision: CSK.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
The study protocol was approved by the Institutional Review Board of the Asan Medical Center (2018-1061). All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board of the Asan Medical Center and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
The Institutional Review Board of the Asan Medical Center waived the requirement for informed consent because of the retrospective design of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Choi, S.Y., Chi, B.H., Lim, B. et al. Percent tumor volume vs American Joint Committee on Cancer staging system subclassification for predicting biochemical recurrence in patients with pathologic T2 prostate cancer. J Cancer Res Clin Oncol 146, 537–543 (2020). https://doi.org/10.1007/s00432-019-03085-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-019-03085-w