Abstract
Objective
The aim of the present study was to investigate the prognostic significance of FDG uptake measured as maximum standardized uptake value (SUVmax) in primary tumor by positron emission tomography with fluorine-18-fluorodeoxyglucose (FDG-PET/CT) and pretreatment serum squamous cell carcinoma antigen (SCC-ag) in patients with cervical cancer.
Methods
82 consecutive patients with biopsy-proven cervical cancer who had PET/CT before any treatment were enrolled in this study. The SUVmax of the primary cervical tumor mass was obtained and compared with pretreatment SCC-ag and pathological prognostic factors after the initial treatment.
Results
There was significant correlation between the SUVmax of the primary tumor and tumor maximum size (p = 0.0024). The serum SCC-ag had a statistically significant association with lymph node metastasis (p = 0.0373), although there was no correlation between the SUVmax of the primary tumor and the serum SCC-ag (r 2 = −0.57). The higher SUVmax of primary tumor (≥11.2) plus pelvic lymph node (PLN) metastasis and higher SUVmax plus higher serum SCC-ag (≥6.4 ng/nl) were two most significant variables that predicted worse prognosis (p = 0.0099 and p = 0.0020, respectively).
Conclusions
Higher pretreatment SUVmax of primary tumor indicated worse prognosis, and the prognosis of patients with higher pretreatment SUVmax plus PLN metastasis was even worse both in patients of squamous cell carcinoma (SCC) and non-SCC of cervix. As for patients with SCC of cervix, higher pretreatment serum SCC-ag not only predicted worse prognosis but also predicted disease recurrence in the posttreatment surveillance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cervical cancer is the third most commonly diagnosed cancer and the fourth leading cause of cancer death in women worldwide, accounting for 9% (529800) of the total new cancer cases and 8% (275100) of the total new cancer deaths among women in 2008 (Jemal et al. 2010). In China, cervical cancer is currently the leading gynecological malignancy in women, with an estimated incidence of more than 131,500 new cases in 2010. According to the International Federation of Obstetrics and Gynecology (FIGO) recommendations, cervical cancer has a 5-year recurrence rate and a 5-year overall mortality rate of 28 and 27.8%, respectively (Benedet et al. 2001). It can be cured by either radical surgery or definitive radiation in almost 80% of patients with early stage of cervical cancer (Chung et al. 2010a, b). Optimal management includes precise clinical staging and optimal treatment followed by deliberate posttherapy surveillance, early detection of recurrence and appropriate salvage therapy (Jao et al. 2010). In the pretreatment setting, it is crucial to stage the tumor accurately and assess the prognostic factor precisely in order to determine the optimal treatment modality (Son et al. 2010). Although LN assessment is not part of the FIGO clinical staging, it is generally performed during the initial workup of patients with cervical cancer as an important component of treatment planning, since the survival rates for patients with nodal metastases are significantly lower than those without nodal metastases (Chung et al. 2010a; Ishikawa et al. 1999; Lai et al. 1999; Sakuragi et al. 1999; Waggoner 2003; Haie-Meder et al. 2010; Kidd et al. 2010a). Other clinical and pathological risk factors including age, histological tumor type, stage, pelvic lymph node (PLN) metastasis, involvement of the resection margin and the parametrium (PM), deep cervical stromal invasion, bulky tumor size, and lymphovascular space invasion (LVSI) have also been identified as predictive of treatment outcome (Chung et al. 2010b; Harry 2010; Kashimura et al. 1990; Werner-Wasik et al. 1995; Perez et al. 1992, 1998).
Serum squamous cell carcinoma antigen (SCC-ag) levels are elevated in 28–88% of patients with squamous cell carcinoma (SCC) and correlate with most predictive factors mentioned above (Nakamura et al. 2010; Sproston et al. 1995; Ngan et al. 1996; Hong et al. 1998; Takeda et al. 2002).
Some studies draw a conclusion that the efficacy of FDG uptake measured as standardized uptake value maximum (SUVmax) in the primary tumor by positron emission tomography with fluorine-18-fluorodeoxyglucose (FDG-PET/CT) was predictive of an inferior outcome (Allal et al. 2002; Downey et al. 2004; Sasaki et al. 2005); however, other studies did not agree (Hoang et al. 2008). Several researches had been done to discuss the relationship between FDG uptake in primary cervical cancer and patients’ outcome (Xue et al. 2006; Schwarz et al. 2007). Since the number of these articles was relatively small, the predictive value of FDG uptake remained uncertain.
In this study, we investigated the SUVmax of the primary cervical cancer and pretreatment serum SCC-ag of the primary SCC of cervix in order to correlate them with clinicopathological characteristics and survival rates in patients with cervical cancer.
Methods
Patients
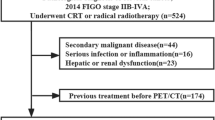
Informed consent was waived due to the retrospective design of the study. All clinical, histological, and imaging data of patients at our institution were collected and stored in a computerized database. Eighty-two consecutive patients with cervical cancer who underwent FDG-PET/CT as part of their initial clinical evaluation at Shanghai Cancer Hospital between November 2003 and March 2011 were included in this analysis. All patients also underwent routine clinical staging including history and physical examination, serum chemistry, liver function panels, and complete blood count. The primary tumor was staged according to the FIGO stage system, and the local extent of disease was diagrammed on a tumor staging form. All patients had biopsy confirmation of their disease. Chest radiography, contrast-enhanced computed tomography (CECT) of the abdomen and pelvis, and FDG-PET/CT were obtained in all patients. Patients were excluded from analysis if any of the following criteria was present :(1) previous diagnosis of another malignant disease, (2) follow-up duration less than 6 months, and (3) lost to follow-up.
Treatment
Patients were treated in the following manners: 29 patients received a combination of external irradiation and intracavitary brachytherapy with curative intent, 8 patients underwent surgery only, 29 patients underwent surgery and received postoperative irradiation, and 16 patients received palliative treatment only. Radiation treatment for cervical cancer was based on standard treatment practices for cervical cancer at the majority of patients who received irradiation also received concurrent cisplatin chemotherapy (40 mg/m2 weekly for 6 cycles).
Serum SCC-antigen assays
The assay for SCC-ag was carried out by radioimmunoassay prior to any treatment at our nuclear medicine laboratory at Shanghai Cancer hospital. The upper limit of normal according to the manufacturer was 1.6 ng/ml.
PET/CT technique
All patients were instructed to fast for at least 6 h before the injection of 18F-FDG with a dosage range of 10–15 mCi (7.4 MBq/kg, 370–555 MBq). Blood glucose was measured before injection of the tracer to ensure glucose blood level was below 10 mmol/l. Before and after injection, patients were kept lying comfortably in a quiet, dimly lit room.
Scanning was initiated 1 h after administration of the tracer. FDG-PET/CT scans were performed on a Siemens biograph 16HR PET/CT scanner. Scan coverage was generally from the orbits to the proximal thighs.
The data acquisition procedures were as follows: CT scanning without administration of oral or intravenous contrast material was first performed, from the proximal thighs to head, with 120 kV, 80–250 mA, pitch 3.6. The CT images were used for attenuation correction of the PET scans. Immediately after CT scanning, a PET emission scan that covered the identical transverse field of view was obtained. PET studies were acquired in 3-dimensional acquisition mode at 3 min per bed position. Images were reconstructed using ordered subset expectation maximum with a 128*128 matrix size. PET/CT images were reviewed on an Advantage Workstation (Syngo Systems; Siemens). PET, CT, and PET/CT fusion datasets were reviewed in multiple imaging planes. All PET/CT scans were reviewed by experienced nuclear radiologists at our institution.
PET imaging evaluation
All PET imaging studies were initially evaluated prospectively by two experienced nuclear physicians informed of the clinical data of the patient at the moment of the scan. Based on knowledge of the normal biodistribution of FDG, lesions were identified as foci with increased tracer accumulation compared to that in comparable normal contralateral structures and/or surrounding soft tissues. The attenuation collection data by CT were measured using SUVmax, a semiquantitative measure of radiotracer uptake, which was normalized using the lean body mass. For measurements of SUV, the region of interest (ROI) was manually defined over the area of abnormal tracer uptake at the site of primary cervical disease and local/regional lymph node and other distant metastatic sites. The SUV was calculated using the following formula:
For the purposes of this analysis, the maximal SUV (SUVmax) was used for correlation with overall survival (OS).
Histological analysis and outcome evaluation
All surgical specimens were diagnosed by one experienced pathologist, and the longest diameter reported by the pathologist was used as the tumor size in this analysis. Tumor-related parameters were collected including histological type, presence or absence of PLN, involvement of the resection margin and the PM, tumor size, and depth of cervical stromal invasion. Tumor recurrence was confirmed by either tissue biopsy or the demonstration of progressive disease by serial imaging methods. Clinical proofs of no recurrent disease consisted of a negative physical and gynecological examination, negative tissue biopsy, and negative findings on serial follow-up imaging methods. Progressive elevation of serum SCC-ag accompanied by an increase in lesion size or appearance of new lesions was considered to be evidence of disease recurrence. All patients had follow-up examinations approximately every 2 months for the first 6 months, every 3 months for the next 2 years, and every 6 months thereafter.
Statistical analysis
Student’s test for unpaired data was used to analyze the differences between two groups. Univariate analysis was performed by the following factors: the SUVmax, serum SCC-ag, and clinic pathological variables (age, histological tumor type, stage, PLN metastasis, involvement of the resection margin and PM, deep cervical stromal invasion, bulky tumor size, and LVSI). All tests were 2-tailed and only p values of <0.05 were considered significant. Survival curves were estimated by the Kaplan–Meier method and examined by the log-rank test. The OS time was defined as the interval between the date of diagnosis and the last date when the patient was reported to be alive (censored) or date of death for any reason (uncensored). Cox proportional hazards regression (Cos 1972) was then used to examine the independent effects of each significant variable. The statistical software (SAS 8.0) was used for all analyses.
Results
Patients’ characteristics
The patient characteristics including initial FIGO stage, histology of disease, age, and treatment are summarized in Table 1. The mean follow-up for all patients who were alive at the time of last follow-up was 19 months (range, 1–57 months). There were 16 patients who had no serum SCC-ag test before treatment (10 non-SCC patients and 6 SCC patients). The mean serum SCC-ag for the 66 patients was 6.4 ng/ml, with a range of 0–94.3 ng/ml. The median serum SCC-ag was 15.75 ng/ml.
Correlation among FDG uptake, FIGO stage, and the presence or absence of lymph node involvement
The mean SUVmax for FDG uptake in the primary cervical disease in all patients was 11.62 ± 5.15 (standard deviation). The median SUVmax was 11.2. The mean values of SUVmax grouped by FIGO stage and nodal status are shown in Table 2. There was no correlation between the SUVmax of the primary cervical cancer and either FIGO stage or the presence or absence of LN involvement on FDG-PET/CT (Table 2).
SUVmax as a predictor of survival
The median SUVmax and the median pretreatment SCC-ag in the study cohort were used as the cutoff value to evaluate the relationship between the OS and primary tumor FDG uptake and/or pretreatment SCC-ag.
The mean survival time was significantly shorter in the higher SUVmax group than in the lower SUVmax group (mean survival time: 18.95 months vs. 19.43 months p = 0.0179).
The univariate analysis showed that the SUVmax (p = 0.0119, Fig. 1) was related to OS as well as other predictive factors, serum SCC-ag (p = 0.0101), stage (p < 0.0001), PLN metastasis (p = 0.0041), and involvement of the resection margin and PM (p = 0.0025) (Table 3).
Kaplan–Meier plots for the OS rates of patients with cervical cancer before any treatment according to their SUVmax (n = 82) of primary tumor or their serum SCC-ag (n = 66). a Serum SCC-ag and OS, Upper line serum SCC-ag (<15.75 ng/nl) (n = 45), Lower line serum SCC-ag (≥15.75 ng/nl) (n = 21). b SUVmax + SCC-ag and OS, Upper line either SUVmax of primary tumor (<11.2) or serum SCC-ag (<15.75 ng/nl) (n = 54), Lower line serum SUVmax of primary tumor (≥11.2) plus serum SCC-ag (≥15.75 ng/nl) (n = 12). c SUVmax and OS, Upper line SUVmax of primary tumor (<11.2) (n = 43), Lower line serum SUVmax of primary tumor (≥11.2) (n = 39). d SUVmax + PLN metastasis and OS, Upper line SUVmax of primary tumor (<11.2) or SUVmax of primary tumor (≥11.2) plus negative LN metastasis (n = 43), Lower line serum SUVmax of primary tumor (≥11.2) plus positive LN metastasis (n = 39)
Figure 1 showed the OS curves of 66 patients who underwent pretreatment of SCC-ag of cervix, according to serum SCC-ag, serum SCC-ag plus SUVmax. It also showed the OS curves of all 82 patients underwent the pretreatment SUVmax of primary tumor and SUVmax of primary tumor plus PLN metastasis. The SUVmax and SCC-ag cutoff value of primary tumor as determined by the median value were 11.2 and 6.4 (ng/ml), respectively. The OS rates of patients grouped by each of the four variables were statistically different. Interestingly, the higher serum SCC-ag plus SUVmax and SUVmax of primary tumor plus PLN metastasis were found to be two most significant variables.
However, age, histological tumor type, deep cervical stromal invasion, bulky tumor size, and LVSI did not show significant relation to OS. With the patients of early stage of cervical cancer, which all had operation later, we used a Cox proportional hazards model to do a multivariate analysis and found only involvement of the resection margin and PM (hazard ratio, 5.810; p = 0.0496) was an independent predictor of survival in early stage of cervical cancer (Table 4).
Discussion
Positron emission tomography (PET) as a noninvasive imaging technique is now widely used in oncology in recent years. It provides both functional and metabolic assessment of normal tissues or diseased conditions (Weissleder 2006; Juweid and Cheson 2006; Maisey 2002).
The prognostic value of FDG uptake was first reported by Fukunaga et al. (1998), revealing that patients with high SUV had a worse prognosis than patients with low SUV. Many studies had been conducted to evaluate PET scanning in the assessment of prognosis, therapeutic response, and the potential to alter management of oncologic patients including patients with lung cancer and esophageal cancer. In a meta-analysis (Pan et al. 2009), the authors discussed the prognostic significance of SUVmax on PET/CT in patients with esophageal cancer and found that higher SUV was associated with a significantly poorer OS and DFS, with the overall HR 1.70 (95%CI: 1.28–2.26) and 2.18 (95%CI: 1.59–2.99), respectively.
Historically, prognostic factors for cervical cancer had included FIGO stage, tumor volume, lymph node status, patient’s age, and treatment techniques (Kodaira et al. 2003; Yalman et al. 2003; Hong et al. 2005).
A previous study conducted by Kidd et al. (2010b) evaluated the prognostic significance of SUVmax for the most FDG-avid pelvic lymph node (SUVPLN) in 83 patients with FIGO stage IB1 to IIIB cervical cancer and demonstrated that SUVPLN was more predictive of outcome than FIGO stage. Another study also showed that SUVmax in the primary tumor of diagnosis was a more significant predictor of outcome in cervical cancer than FIGO stage, tumor volume, histology, or LN involvement (Grigsby et al. 2001). In cervical cancer, CT and/or MRI was usually used in assessment for lymph node metastasis followed by treatment primarily by RT. Several studies revealed the range of sensitivity in detecting LN metastasis compared with surgicopathological findings in cervical cancer of CT and MRI was 24–65% and 24–71%, respectively (Kim et al. 1993; Matsukuma et al. 1989; Yang et al. 2000). Havrilesky et al. (2005) revealed that PET was more sensitive than CT or MRI for the detection of PLN metastasis of cervical cancer (79% vs. 47% vs. 72%, respectively). These findings corresponded well with those reported by earlier studies in other solid tumors such as colorectal carcinomas and ovarian cancers (Heriot et al. 1999; Bipat et al. 2004; Kantorová et al. 2003; Nam et al. 2010).
Pallardy et al. (2010) also found that PET findings with ≤1 focus detected in women who were suspected of having cervical cancer recurrence had better OS than those with PET findings with 2 foci (p = 0.043) or with PET findings with 3–5 foci (p = 0.007). Chung et al. (2010b) showed that the preoperative SUVmax in the primary tumor on PET/CT was the most powerful significant prognostic factor to predict recurrence in stage IB to IIA cervical cancer.
Serum SCC-ag has been shown to correlate with the clinical FIGO stage, tumor volume, and risk of lymph node metastasis (Sproston et al. 1995; Ngan et al. 1996; Hong et al. 1998; Takeda et al. 2002). The most important clinical correlation for pretreatment serum SCC-ag is its ability to predict clinical outcome and its application in the posttreatment surveillance of patients with cervical cancers. The reported lead time between elevation of SCC-ag levels and detection of recurrence is approximately 6 months (Maiman 2002). Nakamura et al. (2010) found serum SCC-ag was significantly greater in association with increasing FIGO stage and tumor maximum size but not associated with OS. It is concluded in Chan et al’s (2002) study and in previous ones that measurement of SCC-ag levels could assist in predicting disease recurrence but would not alter clinical management, because most recurrent lesions were too advanced for curative treatment by the time they were detected by imaging modalities. In our analysis, serum SCC-ag was significantly greater in patients with PLN metastasis though there was no correlation between serum SCC-ag and the SUVmax of the primary tumor in SCC of cervix (Fig. 2). Kidd et al. (2010a) found that the SUVPLN was predictive of treatment response, risk of pelvic disease recurrence, disease-specific survival, and OS, but not strongly correlated with PLN size or the SUVmax of the primary cervical tumor.
In the current study, whether the SUVmax of the primary tumor was correlated with clinicopathological characteristics in patients with cervical cancer was also examined. It is found that the SUVmax of the primary tumor in patients with pretreatment of cervical cancer showed a statistically significant association with tumor maximum size (Table 2). Lee et al. (2009) had reported that a high pretreatment baseline SUVmax in primary cervical cancer was associated with a poor prognosis in patients with early cervical cancer receiving surgery with/without adjuvant therapy. Xue et al. (2006) also found the same phenomenon in patients with advanced cervical cancer who were receiving definitive radiotherapy or concurrent chemotherapy.
There are some limitations in this study: firstly, this study was a retrospective research; secondly, the number of patients was relatively small and this made subgroup analysis rather difficult. Survival curves were so clear more than we expected. Although the patients in this paper were consecutive, they were carefully selected by the clinicians in advance and this may partially cause the potential bias in enrolled patients. But this study did shed some lights on the usefulness of the FDG-PET/CT in prognosis of cervical cancers.
According to our paper and the previous studies and their statements, we can draw some conclusions as follows. Higher pretreatment SUVmax of primary tumor indicated worse prognosis, and the prognosis of patients with higher pretreatment SUVmax plus PLN metastasis was even worse both in patients of SCC and non-SCC of cervix. As for patients of SCC of cervix, higher pretreatment serum SCC-ag not only could predict worse prognosis but also could predict disease recurrence, guide early treatment in the posttreatment surveillance and help improving the overall survival.
References
Allal AS, Dulguerov P, Allaoua M, Haenggeli CA, El-Ghazi el A, Lehmann W, Slosman DO (2002) Standardized uptake value of 2-[(18)F] fluoro-2-deoxy-d-glucose in predicting outcome in head and neck carcinomas treated by radiotherapy with or without chemotherapy. J Clin Oncol 20(5):1398–1404
Benedet JL, Odicino F, Maisonneuve P, Beller U, Creatman WT, Heintz AP et al (2001) Carcinoma of the cervix uteri. J Epidemiol Biostat 6:7–43
Bipat S, Glas AS, Slors FJ, Zwinderman AH, Bossuyt PM, Stoker J (2004) Rectal cancer: local staging and assessment of lymph node involvement with endoluminal US, CT, and MR imaging—a meta-analysis. Radiology 232(3):773–783 (Epub 2004 Jul 23)
Chan YM, Ng TY, Ngan HY, Wong LC (2002) Monitoring of serum squamous cell carcinoma antigen levels in invasive cervical cancer: is it cost-effective? Gynecol Oncol 84(1):7–11
Chung HH, Kang KW, Cho JY, Kim JW, Park NH et al (2010a) Role of magnetic resonance imaging and positron emission tomography/computed tomography in preoperative lymph node detection of uterine cervical cancer. Am J Obstet Gynecol 203(2):156.e1–156.e5
Chung HH, Nam BH, Kim JW, Kang KW, Park NH, Song YS et al (2010b) Preoperative [18F]FDG PET/CT maximum standardized uptake value predicts recurrence of uterine cervical cancer. Eur J Nucl Med Mol Imaging 37(8):1467–1473
Cos DR (1972) Regression models and life-tables. J R Stat Soc B 34:187–200
Downey RJ, Akhurst T, Gonen M, Vincent A, Bains MS, Larson S, Rusch V (2004) Preoperative F-18 fluorodeoxyglucose-positron emission tomography maximal standardized uptake value predicts survival after lung cancer resection. J Clin Oncol 22(16):3255–3260
Fukunaga T, Okazumi S, Koide Y (1998) Evaluation of esophageal cancers using fluorine-18-fluorodeoxyglucose PET. J Nucl Med 39(6):1002–1007
Grigsby PW, Siegel BA, Dehdashti F (2001) Lymph node staging by positron emission tomography in patients with carcinoma of the cervix. J Clin Oncol 19(17):3745–3749
Haie-Meder C, Mazeron R, Magné N (2010) Clinical evidence on PET-CT for radiation therapy planning in cervix and endometrial cancers. Radiother Oncol 96(3):351–355
Harry VN (2010) Novel imaging techniques as response biomarkers in cervical cancer. Gynecol Oncol 116(2):253–261
Havrilesky LJ, Kulasingam SL, Matchar DB, Myers ER (2005) FDG-PET for management of cervical and ovarian cancer. Gynecol Oncol 97(1):183–191
Heriot AG, Grundy A, Kumar D (1999) Preoperative staging of rectal carcinoma. Br J Surg 86(1):17–28
Hoang JK, Hoagland LF, Coleman RE, Coan AD, Herndon JE II et al (2008) Prognostic value of fluorine-18 fluorodeoxyglucose positron emission tomography imaging in patients with advanced-stage non-small-cell lung carcinoma. J Clin Oncol 26(9):1459–1464
Hong JH, Tsai CS, Chang JT, Wang CC, Lai CH, Lee SP et al (1998) The prognostic significance of pre- and posttreatment SCC levels in patients with squamous cell carcinoma of the cervix treated by radiotherapy. Int J Radiat Oncol Biol Phys 41(4):823–830
Hong JH, Tsai CS, Lai CH, Chang TC (2005) Risk stratification of patients with advanced squamous cell carcinoma of cervix treated by radiotherapy alone. Int J Radiat Oncol Biol Phys 63(2):492–499
Ishikawa H, Nakanishi T, Inoue T, Kuzuya K et al (1999) Prognostic factors of adenocarcinoma of the uterine cervix. Gynecol Oncol 73(1):42–46
Jao MS, Chang TC, Chang HP, Wu TI, Chao A, Lai CH et al (2010) Long-term follow up of cervical cancer patients with unexplained squamous cell carcinoma antigen elevation after post-therapy surveillance using positron emission tomography. J Obstet Gynaecol Res 36(5):1003–1008
Jemal A, Siegel R, Xu J, Ward E (2010) Cancer statistics, 2010. CA Cancer J Clin 60(5):277–300
Juweid ME, Cheson BD (2006) Positron-emission tomography and assessment of cancer therapy. N Engl Med 354:496–507
Kantorová I, Lipská L, Bêlohlávek O, Visokai V, Trubaĉ M, Schneiderová M (2003) Routine (18)F-FDG PET preoperative staging of colorectal cancer: comparison with conventional staging and its impact on treatment decision making. J Nucl Med 44(11):1784–1788
Kashimura M, Kashimura Y, Oikawa K, Sakamoto C, Matsuura Y et al (1990) Placental site trophoblastic tumor: immunohistochemical and nuclear DNA study. Gynecol Oncol 38(2):262–267
Kidd EA, Siegel BA, Dehdashti F, Rader JS, Mutch DG, Powell MA, Grigsby PW (2010a) Lymph node staging by positron emission tomography in cervical cancer: relationship to prognosis. J Clin Oncol 28(12):2108–2113
Kidd EA, Siegel BA, Dehdashti F, Grigsby PW (2010b) Pelvic lymph node F-18 fluorodeoxyglucose uptake as a prognostic biomarker in newly diagnosed patients with locally advanced cervical cancer. Cancer 116(6):1469–1475
Kim SH, Choi BI, Han JK, Kim HD (1993) Preoperative staging of uterine cervical carcinoma: comparison of CT and MRI in 99 patients. J Comput Assist Tomogr 17(4):633–640
Kodaira T, Fuwa N, Toita T, Nomoto Y (2003) Comparison of prognostic value of MRI and FIGO stage among patients with cervical carcinoma treated with radiotherapy. Int J Radiat Oncol Biol Phys 56(3):769–777
Lai CH, Hong JH, Hsueh S, Ng KK, Chang TC, Tseng CJ et al (1999) Preoperative prognostic variables and the impact of postoperative adjuvant therapy on the outcomes of stage IB or II cervical carcinoma patients with or without pelvic lymph node metastases: an analysis of 891 cases. Cancer 85(7):1537–1546
Lee YY, Choi CH, Kim CJ, Kang H, Kim TJ, Lee JW, Lee JH (2009) The prognostic significance of the SUVmax (maximum standardized uptake value for F-18 fluorodeoxyglucose) of the cervical tumor in PET imaging for early cervical cancer: preliminary results. Gynecol Oncol 115(1):65–68 (Epub 2009 Jul 15)
Maiman M (2002) The clinical application of serum squamous cell carcinoma antigen level monitoring in invasive cervical carcinoma. Gynecol Oncol 84(1):4–6
Maisey MN (2002) Overview of clinical PET. Br J Radiol 75(Spec No):S1–S5
Matsukuma K, Tsukamoto N, Matsuyama T, Ono M, Nakano H (1989) Preoperative CT study of lymph nodes in cervical cancer—its correlation with histological findings. Gynecol Oncol 33(2):168–171
Nakamura K, Okumura Y, Kodama J, Hongo A, Kanazawa S, Hiramatsu Y (2010) The predictive value of measurement of SUVmax and SCC-antigen in patients with pretreatment of primary squamous cell carcinoma of cervix. Gynecol Oncol 119(1):81–86 (Epub 2010 Jun 26)
Nam EJ, Yun MJ, Oh YT, Kim JW, Kim JH, Kim S (2010) Diagnosis and staging of primary ovarian cancer: correlation between PET/CT, Doppler US, and CT or MRI. Gynecol Oncol 116(3):389–394 (Epub 2009 Nov 18)
Ngan HY, Cheung AN, Lauder IJ, Wong LC, Ma HK (1996) Prognostic significance of serum tumour markers in carcinoma of the cervix. Eur J Gynaecol Oncol 17(6):512–517
Pallardy A, Bodet-Milin C, Oudoux A (2010) Clinical and survival impact of FDG PET in patients with suspicion of recurrent cervical carcinoma. Eur J Nucl Med Mol Imaging 37(7):1270–1278 (Epub 2010 Mar 20)
Pan L, Gu P, Huang G, Xue H, Wu S (2009) Prognostic significance of SUV on PET/CT in patients with esophageal cancer: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol 21(9):1008–1015
Perez CA, Grigsby PW, Nene SM, Camel HM, Galakatos A, Kao MS, Lockett MA (1992) Effect of tumor size on the prognosis of carcinoma of the uterine cervix treated with irradiation alone. Cancer 69(11):2796–2806
Perez CA, Grigsby PW, Chao KS, Mutch DG, Lockett MA (1998) Tumor size, irradiation dose, and long-term outcome of carcinoma of uterine cervix. Int J Radiat Oncol Biol Phys 41(2):307–317
Sakuragi N, Satoh C, Takeda N, Hareyama H, Takeda M, Yamamoto R et al (1999) Incidence and distribution pattern of pelvic and paraaortic lymph node metastasis in patients with stages IB, IIA, and IIB cervical carcinoma treated with radical hysterectomy. Cancer 85(7):1547–1554
Sasaki R, Komaki R, Macapinlac H, Erasmus J, Allen P, Forster K, Putnam JB et al (2005) [18F]fluorodeoxyglucose uptake by positron emission tomography predicts outcome of non-small-cell lung cancer. J Clin Oncol 23(6):1136–1143
Schwarz JK, Siegel BA, Dehdashti F, Grigsby PW (2007) Association of posttherapy positron emission tomography with tumor response and survival in cervical carcinoma. JAMA 298(19):2289–2295
Son H, Kositwattanarerk A, Hayes MP, Chuang L, Rahaman J, Heiba S et al (2010) PET/CT evaluation of cervical cancer: spectrum of disease. Radiographics 30(5):1251–1268
Sproston AR, Roberts SA, Davidson SE, Hunter RD, West CM (1995) Serum tumour markers in carcinoma of the uterine cervix and outcome following radiotherapy. Br J Cancer 72(6):1536–1540
Takeda M, Sakuragi N, Okamoto K, Todo Y, Minobe S, Nomura E, Negishi H et al (2002) Preoperative serum SCC, CA125, and CA19-9 levels and lymph node status in squamous cell carcinoma of the uterine cervix. Acta Obstet Gynecol Scand 81(5):451–457
Waggoner SE (2003) Cervical cancer. Lancet 361(9376):2217–2225
Weissleder R (2006) Molecular imaging in cancer. Science 312:1168–1171
Werner-Wasik M, Schmid CH, Bornstein L, Ball HG, Smith DM et al (1995) Prognostic factors for local and distant recurrence in stage I and II cervical carcinoma. Int J Radiat Oncol Biol Phys 32(5):1309–1317
Xue F, Lin LL, Dehdashti F, Miller TR, Siegel BA, Grigsby PW (2006) F-18 fluorodeoxyglucose uptake in primary cervical cancer as an indicator of prognosis after radiation therapy. Gynecol Oncol 101(1):147–151
Yalman D, Aras AB, Ozkök S, Duransoy A (2003) Prognostic factors in definitive radiotherapy of uterine cervical cancer. Eur J Gynaecol Oncol 24(3–4):309–314
Yang WT, Lam WW, Yu MY, Cheung TH, Metreweli C (2000) Comparison of dynamic helical CT and dynamic MR imaging in the evaluation of pelvic lymph nodes in cervical carcinoma. AJR Am J Roentgenol 175(3):759–766
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pan, L., Cheng, J., Zhou, M. et al. The SUVmax (maximum standardized uptake value for F-18 fluorodeoxyglucose) and serum squamous cell carcinoma antigen (SCC-ag) function as prognostic biomarkers in patients with primary cervical cancer. J Cancer Res Clin Oncol 138, 239–246 (2012). https://doi.org/10.1007/s00432-011-1092-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-011-1092-z