Abstract
Purpose
Previously, we conducted a nationwide survey of primary central nervous system lymphoma (PCNSL) treated between 1985 and 1994 in Japan. In the present study, we conducted further investigations of PCNSL patients treated between 1995 and 1999 to clarify possible changes with time in the clinical features, treatment, and outcome of this disease.
Methods
Thirteen Japanese institutions were surveyed, and data on 101 patients with histologically-confirmed PCNSL were collected. These data were compared with those of 167 patients treated at the same institutions between 1985 and 1994.
Results
Regarding patient and tumor characteristics, the proportion of patients with good performance status (PS) was significantly higher in the group treated during 1995–1999 than in that treated during 1985–1994, but other characteristics were not significantly different. Regarding treatment, more patients in the more recent period (66%) received systemic chemotherapy than those in the preceding period (53%, P = 0.049). For all patients, including those who did not complete radiotherapy, the median survival time was 17 months and 30 months in patients treated between 1985 and 1994 and those treated between 1995 and 1999, respectively, and the 5-year survival rate was 15% versus 31% (P = 0.0003). In both patient groups, higher age and tumor multiplicity were associated with poor prognosis in multivariate analysis. In patients treated between 1995 and 1999, those who received systemic chemotherapy showed significantly better prognosis than those who did not (P = 0.0049), but the difference was not significant in multivariate analysis (P = 0.23).
Conclusions
The high survival rates observed in the present survey are comparable with those of recent prospective studies employing intensive chemoradiotherapy. The improvement in prognosis appeared to result, at least in part, from the increase in the proportion of patients with better PS. Since the clinical feature and treatment outcome of patients with PCNSL can thus change with the era, historical control data should not be used in comparing different treatment modalities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary central nervous system lymphoma (PCNSL) is increasing and is becoming one of the most important tumors in neuro-oncology. Radiation therapy has been the standard treatment for PCNSL until recently, but the outcome of patients treated by radiation alone has not necessarily been satisfactory (Shibamoto et al. 1990; Reni et al. 1997; Hayabuchi et al. 1998; Nelson 1999). More recently, the use of high-dose methotrexate (MTX)-containing chemotherapy before radiation appeared to have gained some success in obtaining long-term survival (Glass et al. 1994; Blay et al. 1998; Brada et al. 1998; Abrey et al. 2000; Ferreri et al. 2000; O’Brien et al. 2000; Reni et al. 2001; Bessel et al. 2001; Caldoni & Aebi 2002; DeAngelis et al. 2002). However, there has been no randomized trial suggesting the superiority of the combined modality treatment over radiation therapy alone, and a recent study by a German group suggested a high rate of progressive disease during treatment with 6 courses of 8 g/m2 of MTX (Herrlinger et al. 2002). Therefore, the benefit of high-dose MTX appears to remain uncertain. Since the clinical features of PCNSL appear to be changing with time, it may not be reasonable to consider that combined MTX-containing chemotherapy and radiation is superior to radiation alone, by comparing the results of combined treatment with the historical control data in patients treated by radiation therapy alone.
Previously, Hayabuchi et al. (Hayabuchi et al. 1998) conducted a nationwide survey of PCNSL in Japan treated between 1985 and 1994. The findings on 466 patients were previously published. Considering the increasing importance of this disease, we organized a research group consisting of 13 institutions to carry out both retrospective and prospective studies on PCNSL. As a first study of this group, we collected data on PCNSL patients treated between 1995 and 1999 at these institutions. In addition to analyzing these data on 101 patients, we compared the data with those on 167 patients from the previous survey treated between 1985 and 1994 at the same institutions, to investigate changes in the clinical feature, treatment modality, and outcome between these eras.
Materials and methods
Subjects of the present survey were patients with histologically-proven PCNSL who received radiation therapy between 1995 and 1999. Those who did not complete the planned radiotherapy were included. Clinical characteristics, treatment and prognosis of each patient shown in the Results section were asked using a detailed questionnaire. Data on 101 patients were collected from 13 institutions. For comparison, data on 167 patients treated in the preceding 10 years, i.e., between 1985 and 1994, at the same institutions were obtained from the data source of the previous nationwide survey (Hayabuchi et al. 1998) and were analyzed. Data regarding tumor size (maximum diameter at diagnosis and before radiation therapy) was asked for in the present survey, which had not been done in the previous survey. As often happens with such a survey, a number of the items were unanswered by the investigators. Various chemotherapy regimens had been used, and were categorized as follows: (A) cyclophosphamide, vincristine, and prednisolone (COP) or COP plus doxorubicin (CHOP/VEPA); (B) intravenous methotrexate (MTX) alone or MTX-containing regimens. The drugs included in regimen A had often been used in combination with MTX, and such regimens were categorized into this group; (C) cytarabine plus procarbazine; (D) nitrosourea-containing regimens. Some of the drugs in regimen A had been used in combination with nitrosoureas, and such regimens were included in this group. When MTX had been used in combination, the regimen was categorized into group B; (E) cisplatin plus etoposide; and (F) Single use or combination of miscellaneous other agents not included in the above groups. For analysis of treatment results, regimens C–F were grouped together. Differences in patient, tumor, and treatment characteristics between groups were examined by Fisher’s exact test.
Survival rates were calculated from the date of starting radiotherapy using the Kaplan-Meier method, and differences in pairs of survival curves were examined by the log-rank test. Multivariate analysis of prognostic factors was carried out using the Cox proportional hazards model. In doing multivariate analysis, patients were divided into two groups, and all the parameters were entered as dichotomous variables. All statistical analyses were carried out using a computer program, Stat View Version 5 (SAS institute, Cary, NC, USA).
Results
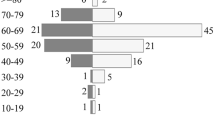
Table 1 shows patient, tumor, and treatment characteristics in the two groups treated between 1985 and 1994 and between 1995 and 1999. There were more patients with better WHO performance status (PS) score in the group treated between 1995 and 1999 than in the group treated in the preceding 10 years, but the other patient and tumor characteristics did not differ significantly between the two groups. Radiotherapy characteristics were similar between the two groups. During both study periods, more than 85% of the patients were treated with whole-brain irradiation with or without focal boost, and the median total and whole brain doses were 50 Gy and 40 Gy, respectively. Whole spinal irradiation was employed in less than 10% of the patients. On the other hand, more patients seen between 1995 and 1999 received systemic chemotherapy than those seen between 1985 and 1994 (66% vs 53%, P = 0.049). Table 2 shows chemotherapy regimens used in the two groups. The use of MTX-containing regimens appeared to be increasing recently. However, a high dose of MTX (>2 g/m2 per administration) was used in only 14 patients (14% of all patients) treated between 1995 and 1999.
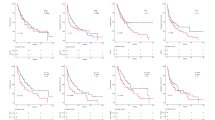
Figure 1 shows overall survival curves for all patients in the two groups. Patients in the present survey had significantly better survival rates than those in the previous survey (P = 0.0003); median survival time was 30 vs 17 months, and the 3-year survival rate was 46% vs 24%. The 5-year survival was 31% and 15%, respectively. Table 3 summarizes survival data in the two groups according to potential prognostic factors. In both study periods, patients with ages <60 years, PS 0–2, or a single tumor showed significantly higher survival rates. Patients with normal lactate dehydrogenase (LDH) levels or without B symptom had better prognoses than those with high LDH level or with B symptom, respectively, in the group treated between 1995 and 1999, but not in those treated during 1985–1994.
To analyze the influence of treatment-related factors on outcome, patients who did not complete radiotherapy (and died soon) were excluded. In patients treated between 1985 and 1994, those who received partial-brain radiation, spinal radiation, or whole-brain dose <40 Gy showed better prognoses, but these phenomena were not observed in patients treated between 1995 and 1999. Figure 2 shows survival curves according to the treatment modality, i.e., radiation alone vs radiation plus chemotherapy. In patients treated between 1985 and 1994, the two groups showed similar prognoses. In patients treated between 1995 and 1999, however, those who received radiation plus chemotherapy showed significantly better survival than those who received radiation alone. Among these patients, 61% of the patients who received radiochemotherapy were younger than 60 years, but 39% of those treated with radiation alone were younger than 60 years (P = 0.050). Similarly, 64% of the patients who received radiochemotherapy had a PS 0–2, but 55% of those treated with radiation had a PS 0–2 (P = 0.50). Figure 3 shows survival curves according to the chemotherapy regimens. In patients treated between 1985 and 1994, there was no significant difference in survival curves according to the regimens. On the other hand, there was an overall difference in those treated between 1995 and 1999 (P = 0.018). Patients receiving MTX-containing regimens showed better survival than those treated with CHOP/VEPA or COP (P = 0.0071).
Survival curves according to the treatment modality. _____○_____ : patients treated with radiation alone, - - -●- - - : patients treated with radiation and chemotherapy. The difference was significant in the group of patients treated between 1995 and 1999 (upper panel, P = 0.63; lower panel, P = 0.0049)
Survival curves according to chemotherapy regimens. _____○_____ : cyclophosphamide, vincristine, prednisolone ± doxorubicin, - - -●- - - : methotrexate-containing regimens, - - -△- - - : other regimens. The difference among the curves was significant in the group of patients treated between 1995 and 1999 (upper panel, P = 0.32; lower panel, P = 0.018)
Multivariate analyses were performed for potential prognostic factors, which were significant in univariate analyses (Table 4). Factors concerning the radiation field and spinal radiation were not included because of the small number of patients in one of the groups. In both patient groups treated during 1985–1994 and 1995–1999, age and tumor number were suggested to be significant prognostic factors. PS and LDH level did not reach statistical significance. The radiation dose to the whole brain and chemotherapy did not prove significant in patients treated between 1985 and 1994, and in those treated between 1995 and 1999, respectively.
Discussion
The most significant finding of this study appears to be that patients treated between 1995 and 1999 showed a significantly better prognosis than those treated between 1985 and 1994. Comparison of the patient and tumor characteristics revealed that there were more patients with better PS between 1995 and 1999 than between 1985 and 1994. This may be due to the earlier diagnosis of the disease in recent years and improvement in general care including corticosteroid therapy and less aggressive surgery. Since PS was a significant prognostic factor in univariate analysis, it is suggested that the increase in the proportion of better PS patients may, at least in part, have contributed to the improvement in prognosis in patients treated between 1995 and 1999.
Age, PS, and tumor multiplicity are well-known prognostic factors for PCNSL (Corry et al. 1998; Hayabuchi et al. 1998; O’Brien et al. 2000). The present results of univariate analyses agree with these previous observations, although the influence of PS did not reach a significant level in multivariate analysis. Patients with a high LDH level treated between 1995 and 1999 showed a poorer prognosis than those with a normal LDH level in univariate analysis. However, LDH was not a significant factor in patients treated between 1985 and 1994, as also shown in the multivariate analysis of patients treated between 1995 and 1999. The previous analysis of 466 patients in the nationwide survey suggested an association of high LDH level and poor prognosis in both univariate and multivariate analyses (Hayabuchi et al. 1998), so LDH may be a potential prognostic factor which is certainly weaker than age, PS, and tumor multiplicity. A similar finding was obtained regarding B symptom. In the newer survey, we investigated the influence of tumor size, but it did not appear to have a significant influence on patient outcome.
Regarding the method of radiation therapy, patients who were treated with a partial-brain field showed a better prognosis than those treated with a whole-brain field in the group treated between 1985 and 1994. Shibamoto et al. (Shibamoto et al. 2003) recently discussed the possible benefit of using partial-brain irradiation, especially in patients with a single lesion. Due to the retrospective nature of the present study and the small number of patients who received partial-brain irradiation, no conclusion should be drawn regarding radiation field, but avoiding whole-brain radiation may be a future topic in the treatment of PCNSL. The observation in the earlier period that patients who received spinal radiation and those who received whole-brain doses of less than 40 Gy had a better prognosis are paradoxical, and it is suggested that these observations would represent patient selection bias, which is often seen in retrospective analysis. As has been suggested by previous findings (Nelson et al. 1992; Hayabuchi et al. 1998), a higher dose of radiation did not appear to be associated with survival improvement.
In patients treated between 1985 and 1994, those who received radiation alone and those who received radiation plus chemotherapy showed a similar prognosis. On the other hand, in patients treated between 1995 and 1999, those who received radiation plus chemotherapy had a significantly better prognosis than those who received radiation alone. However, the effect of chemotherapy was not significant in multivariate analysis. Since younger patients were more often treated with combined radiation and chemotherapy, this may be one of the reasons why the effect of chemotherapy was not supported by multivariate analysis. Analysis according to chemotherapy regimens suggested a possible advantage of MTX-containing regimens over conventional CHOP or similar regimens. Several studies have suggested the ineffectiveness of CHOP or similar regimens, especially when given before radiation (Schultz et al. 1996; O’Neill 1999; Mead et al. 2000), although post-radiation CHOP requires further investigation (Shibamoto et al. 1999). The present findings suggest that systemic chemotherapy with weak or moderate intensity may not be beneficial in PCNSL.
The findings of the present study revealed that the treatment outcome for PCNSL varies greatly with the era. Although most of the chemotherapy regimens used were of mild or moderate intensity and only 14% of the patients received high-dose-MTX-containing chemotherapy, the 5-year survival rate of 31% for all patients treated between 1995 and 1999 (including those who did not complete radiotherapy) were equal to that recently reported by the Radiation Therapy Oncology Group (DeAngelis et al. 2002) or those of other series using intensive combined modality treatment including high-dose MTX (Brada 1998; Bessell et al. 2001). Therefore, it appears to be inappropriate to discuss the usefulness of treatment modality by comparing with the historical control data. There have been no major randomized studies, except for a small one (Mead et al. 2000), regarding the benefit of combining chemotherapy with radiation, but to confirm the efficacy of chemotherapy, randomized studies appear to be necessary.
References
Abrey LE, Yahalom J, DeAngelis LM (2000) Treatment for primary CNS lymphoma: the next step. J Clin Oncol 18:3144–3150
Bessell EM, Graus F, Lopez-Guillermo A, Villa S, Verger E, Petit J, Holland I, Byrne P (2001) CHOD/BVAM regimen plus radiotherapy in patients with primary CNS non-Hodgkin’s lymphoma. Int J Radiat Oncol Biol Phys 50:457–464
Blay JY, Conroy T, Chevreau C, Thyss A, Quesnel N, Eghbali H, Bouabdallah R, Coiffier B, Wagner JP, Le Mevel A, Dramais-Marcel D, Baumelou E, Chauvin F, Biron P (1998) High-dose MTX for the treatment of primary cerebral lymphomas: analysis of survival and late neurologic toxicity in a retrospective series. J Clin Oncol 16:864–871
Brada M, Hjiyiannakis D, Hines F, Traish D, Ashley S (1998) Short intensive primary chemotherapy and radiotherapy in sporadic primary CNS lymphoma. Int J Radiat Oncol Biol Phys 40:1157–1162
Calderoni A, Aebi S (2002) Combination chemotherapy with high-dose MTX and cytarabine with or without brain irradiation for primary central nervous system lymphomas. J Neurooncol 59:227–230
Corry J, Smith JG, Wirth A, Quong G, Liew KH (1998) Primary central nervous system lymphoma: age and performance status are more important than treatment modality. Int J Radiat Oncol Biol Phys 41:615–620
DeAngelis LM, Seiferheld W, Schold SC, Fisher B, Schultz CJ (2002) Combination chemotherapy and radiotherapy for primary central nervous system lymphoma: Radiation Therapy Oncology Group Study 93–10. J Clin Oncol 20:4643–4648
Ferreri AJM, Reni M, Villa E (2000) Therapeutic management of primary central nervous system lymphoma: lessons from prospective trials. Ann Oncol 11:927–937
Glass J, Gruber ML, Chef L, Hochberg FH (1994) Preirradiation MTX chemotherapy of primary central nervous system lymphoma: long-term outcome. J Neurosurg 81:188–195
Hayabuchi N, Shibamoto Y, Onizuka Y, JASTRO CNS Lymphoma Study Group members (1999) Primary central nervous system lymphoma in Japan: a nationwide survey. Int J Radial Oncol Biol Phys 44:265–272
Herrlinger U, Schabet M, Brugger W, Kortmann RD, Kuker W, Deckert M, Engel C, Schmeck-Lindenau HJ, Mergenthaler HG, Krauseneck P, Benohr C, Meisner C, Wiestler OD, Dichgans J, Kanz L, Bamberg M, Weller M (2002) German Cancer Society Neuro-Oncology Working Group NOA-03 multi-center trial of single-agent high-dose MTX for primary central nervous system lymphoma. Ann Neurol 51:247–252
Mead GM, Bleehen NM, Gregor A, Bullimore J, Shirley D, Rampling RP, Trevor J, Glaser MG, Lantos P, Ironside JW, Moss TH, Brada M, Whaley JB, Stenning SP (2000) A Medical Research Council randomized trial in patients with primary central non-Hodgkin’s lymphoma. Cerebral radiotherapy with and without cyclophosphamide, doxorubicin, vincristine, and prednisone chemotherapy. Cancer 89:1359–1370
Nelson DF (1999) Radiotherapy in the treatment of primary central nervous system lymphoma (PCNSL). J Neuro-Oncol 43:241–247
Nelson DF, Martz KL, Bonner H, Nelson JS, Newall J, Kerman HD, Thomson JW, Murray KJ (1992) Non-Hodgkin’s lymphoma of the brain: can high dose, large volume radiation therapy improve survival? Report on a prospective trial by the Radiation Therapy Oncology Group (RTOG): RTOG 8315. Int J Radial Oncol Biol Phys 23:9–17
O’Brien P, Roos D, Pratt G, Liew K, Barton M, Poulsen M, Olver I, Trotter G (2000) Phase II multicenter study of brief single-agent MTX followed by irradiation in primary CNS lymphoma. J Clin Oncol 18:519–526
O’Neill BP, O’Fallon JR, Earle JD, Colgan JD, Earle JD, Krigel RL, Brown LD, McGinnis WL (1999) Primary central nervous system non-Hodgkin’s lymphoma (PCNSL): survival advantages with combined initial therapy? A final report of the North Central Cancer Treatment Group (NCCTG) study 86–72–52. Int J Radiat Oncol Biol Phys 43:559–563
Reni M, Ferreri AJM, Garancini MP, Villa E (1997) Therapeutic management of primary central nervous system lymphoma in immunocompetent patients: results of a critical review of the literature. Ann Onco1 8:227–234
Reni M, Ferreri AJ, Guha-Thakurta N, Blay JY, Dell’Oro S, Biron P, Hochberg FH (2001) Clinical relevance of consolidation radiotherapy and other main therapeutic issues in primary central nervous system lymphomas treated with upfront high-dose MTX. Int J Radiat Oncol Biol Phys 51:419–425
Schultz C, Scott C, Sherman W, Donahue B, Fields J, Murray K, Fisher B, Abrams R, Meis-Kindblom J (1996) Preirradiation chemotherapy with cyclophosphamide doxorubicin, vincristine, and dexamethazone for primary CNS lymphomas: initial report of Radiation Therapy Oncology Group protocol 88–06. J Clin Oncol 14:556–564
Shibamoto Y, Tsutsui K, Dodo Y, Yamabe H, Shima N, Abe M (1990) Improved survival rate in primary intracranial lymphoma treated by high-dose radiation and systemic vincristine-doxorubicin-cyclophosphamide-prednisolone chemotherapy. Cancer 65:1907–1912
Shibamoto Y, Sasai K, Oya N, Hiraoka M (1999) Systemic chemotherapy with vincristine, cyclophosphamide, doxorubicin and prednisolone following radiotherapy for primary central nervous system lymphoma: a phase II study. J Neurooncol 42:161–167
Shibamoto Y, Hayabuchi N, Hiratsuka J, Tokumaru S, Shirato H, Sougawa M, Oya N, Uematsu Y, Hiraoka M (2003) Is whole-brain irradiation necessary for primary central nervous system lymphoma? Patterns of recurrence following partial-brain irradiation. Cancer 97:128–133
Acknowledgements
This study was supported in part by Grants-in-Aid for Scientific Research from the Japanese Ministry of Education, Culture, Sports, Science and Technology (14030042, 14370276, 14657214). The authors wish to thank Drs. Kumiko Karasawa, Atsushi Nishikawa, Naoto Shikama, Koichi Isobe, and Kuniaki Katsui for valuable help in collecting data.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author affiliations are: Niigata University (ET), Tokyo Women’s Medical University (KS), Kyoto University (NO), Gunma University (M Hasegawa), Kurume University (YT, NH), Okayama University (MT), National Cancer Center (M Sumi), Kawasaki Medical School (JH), Cancer Research Institute (MO), Osaka City University (M Hosono), Chiba University (SY), Kansai Medical University (M Sougawa), and Tohoku University (YK)
Rights and permissions
About this article
Cite this article
Shibamoto, Y., Tsuchida, E., Seki, K. et al. Primary central nervous system lymphoma in Japan 1995–1999: changes from the preceding 10 years. J Cancer Res Clin Oncol 130, 351–356 (2004). https://doi.org/10.1007/s00432-004-0547-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-004-0547-x