Abstract
Purpose
Near infrared cholangiography (NIRC) with indocyanine green (ICG) directly injected into the gallbladder is a novel technique to outline biliary anatomy. The purpose of this article is to analyze the usefulness and feasibility of NIRC as a safety method during laparoscopic cholecystectomies.
Material and methods
A case-controlled study comparing 20 patients undergoing laparoscopic cholecystectomies with NIRC with direct injection of ICG into the gallbladder to 20 consecutive standard cholecystectomies. Operative time, length of stay, complications, conversion rates, and biliary injury were analyzed.
Results
Both groups were comparable in epidemiological characteristics. In the ICG group fluorescent visualization of the junction of the Hartmann pouch and the whole cystic duct was achieved in 16 (80%) patients. Median surgical time was 65 (50–76) and 55 (45–71) min for the ICG and the control group, respectively (p = 0.113). There were no postoperative complications and no biliary duct injuries in any of the groups, and a patient from both groups underwent conversion to open surgery.
Conclusion
NIRC with direct injection of ICG into the gallbladder is a feasible method that is not time-consuming; it does not require a different learning curve from standard laparoscopic cholecystectomies and has no major complications described so far.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic cholecystectomies are one of the most frequently performed surgeries in a General and Digestive Surgery Department worldwide. Over 750,000 cholecystectomies are performed each year in the USA [1]. According to the CMBD (Conjunto Mínimo Básico de Datos) of the Spanish National Health system in 2017, 78,567 cholecystectomies were performed in Spain, of which 86.4% were laparoscopic cholecystectomies [2].
Bile duct injury remains one of the most feared complications related to cholecystectomies. With varying severity, total incidence of iatrogenic biliary lesions ranges from 0.08 to 1.5% [3]. Since laparoscopic cholecystectomies are so common, there are thousands of patients every year that suffer these complications, making it essential to keep on putting efforts into minimizing biliary lesions. Iatrogenic bile duct injuries are mostly due to a false identification of the common bile duct (CBD) or the common hepatic duct (CHD), mistaking it for the cystic duct (CD). These lesions are influenced by the learning curve, volume, technical pitfalls, and by patient variations of the biliary tree and vascularization that lead to misinterpretations of the anatomy [4].
In order to reduce iatrogenic biliary lesions, the critical view of safety, described in 2002 by Strasberg [5], has been implemented as an almost mandatory step when performing a laparoscopic cholecystectomy. It consists in the visualization of the triangle formed by the cystic duct, the common hepatic duct, and the inferior edge of the liver, as well as identification of the cystic plate and two tubular structures (the cystic duct and the cystic artery) entering the gallbladder [6].
To further ensure the correct identification of the biliary anatomy, several cholangiographic methods have been used. Traditionally intraoperative cholangiography (IOC), based on series of X-rays taken after the injection of radiopaque-contrast into the cystic duct (CD), has been used in demanding cases. There is still controversy about using IOC routinely as some reviews have pointed out there is no benefit in reducing bile duct injury. However, retrospective databases showed lower incidence when using IOC [7]. Probably, this technique has never gained a wide support to be used on a daily basis due to its time-consuming set up, irradiation of the patient and staff, and most of all due to its complexity in technique as it requires expertise to canalize the cystic duct.
Recently, with the advance of new generation laparoscopic cameras that have integrated near infrared vision, near-infrared cholangiography (NIRC) has gained popularity. This technique enables the visualization of the biliary structures using the fluorescent properties of indocyanine green (ICG), and it is useful to identify unexpected anatomical variations.
ICG is a non-toxic dye with fluorescent properties when excited with light of near infrared wavelength (750–950 nm). The ICG was discovered by the photographic industry and introduced into clinical practice in 1959 as a method to assess liver function, cardiac output, and retinal angiography [8]. ICG is metabolized by microsomes in the liver and is excreted via the liver and bile ducts, allowing it to be used as a cholangiographic method. There are two methods described for cholangiography with fluorescence with ICG: intravenous injection and direct injection into the gallbladder/cystic duct [8]. ICG has a good safety profile; side effects are reported in less than 1 out of 40,000 patients. There have been described some very rare cases of allergy (adverse reactions to ICG given intravenously are around 0.003%) in patients with allergy to iodine as it is manufactured with a small amount of sodium iodide [9].
The intravenous injection of ICG is the most frequently performed method as it is easy to perform. Already in 1992, Araki et al. described the visualization of the biliary anatomy during a laparoscopic cholecystectomy using intravenous ICG [10]. Currently, fluorescence cholangiography with ICG injected intravenously has gained acceptance as an established technique [11]. Vlek et al. in their recent systematic review conclude that fluorescence cholangiography with intravenous ICG and radiological cholangiography were equivalent for biliary tract visualization [12].
The direct injection of ICG into the gallbladder was described initially in animal models [13], and it was only performed in humans for the first time in 2017 [8]. This NIRC technique is less widely used at the present, but, as exposed further in this article, it provides some relevant advantages compared with intravenous NIRC, like direct visualization of the biliary anatomy with no interference of the background liver fluorescence [13].
Aim
The aim of this study is to evaluate the feasibility and usefulness of NIRC with direct injection of ICG into the gallbladder during laparoscopic cholecystectomies.
Methods
Study design
Since January 2019, 20 successive laparoscopic cholecystectomies with direct ICG injection into the gallbladder were followed. Informed consent was obtained for all the procedures. Epidemiological data, gender, age, American Society of Anesthesiologists score (ASA), and body mass index (BMI), were systematically collected. Also, the duration of the surgery (min), length of hospital stay (days) and complications according to Clavien Dindo, and visualization (Y/N) of biliary structures such as cystic duct (CD) and common bile duct (CBD) were registered. The data from this group were compared with a group of 20 consecutive laparoscopic cholecystectomies that had been previously performed by retrospectively retrieving the information from medical charts.
Prospectively collected data of patients undergoing laparoscopic cholecystectomy with ICG from January 2019 till December 2019 were compared with the metrics of a retrospective group undergoing laparoscopic cholecystectomy without ICG operated between October 2018 and January 2019. Only patients undergoing laparoscopic cholecystectomy were included for analysis.
The lead surgeon F.P. was present in all surgeries, but the procedures were often performed by residents as it is usual in our center, given that is a teaching hospital.
Primary outcomes included the duration of surgery, conversion following attempted laparoscopic cholecystectomy, and bile duct injury. The length of stay and postoperative complications constituted our secondary outcome measures.
The technique
Laparoscopic cholecystectomy in our center is performed using the three port technique (with occasional 4th assisting port located in the epigastrium). Surgery begins with an infraumbilical incision, and peritoneum is instilled via a Veress needle.
For the ICG group, the ICG solution is prepared on the surgical back table. A 25-mg vial of ICG powder is dissolved in 10 mL sterile water to create a 2.5-mg/mL solution;
After the correct exposure of the right hypochondrium, the gallbladder fundus is grasped with no prior dissection of the triangle of Calot and a Veress needle is inserted into the gallbladder’s fundus and bile is aspirated to empty the gallbladder.
Then 1 mL of the 2.5-mg/mL solution is mixed with 9 mL of bile that we have kept while aspirating. This creates a final 10-mL ICG-bile solution with a concentration approximately of 0.25 mg/mL). This solution is then re-injected into the gallbladder until initial fluorescent glow is evidenced; usually, we require the injection of just 2–3 mL. Using an Olympus EndoEye 3D camera, fluorescent glow is immediate and delimitation of the biliary tree structures is observed within seconds.
The Veress needle is then removed, and the puncture site pinched closed with a grasper/suture or clip.
In both groups a classical laparoscopic cholecystectomy is then performed. It is made sure to obtain the critical view of safety. In the ICG group, during dissection of Calot’s triangle, standard light and NIR light modes are toggled back and forth to take advantage of both modes of visualization. The NIR light is also applied to help in the dissection of the gallbladder from the liver bed.
Statistical analysis
The continuous quantitative variables are presented with absolute numbers, median and interquartile ranges, and the categorical variables with absolute numbers and/or percentages. The quantitative data were compared with Mann–Whitney U test and the categorical variables with the chi-square test.
Statistical significance is considered if it is less than 0.05. The statistical analysis was carried out with the SPSS® version 21.0 program.
Results
The patient characteristics are shown in Table 1. There were no statistically significant differences in epidemiological characteristics between the two groups in terms of age, sex, ASA, or BMI.
As shown in Table 2, there were also no significant differences neither in the operative time nor in the length of stay. No postoperative complications were observed in any group as well as no bile duct injuries. In the control group there was a case of conversion due to Mirizzi syndrome requiring a hepaticojejunostomy. In the ICG group there was also one conversion to open surgery because of an acute necro-hemorrhagic cholecystitis that precluded safe dissection.
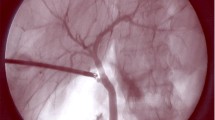
The visualization of the biliary anatomy among the ICG group is summarized in Table 3. In 80% of the patients the junction of the Hartmann pouch and the whole cystic duct was visualized (see Fig. 1) and of those more than half showed enough progression of the ICG to clearly identify the junction of the cystic duct and the CBD. In one patient the gallbladder was punctured through with the veress needle, causing ICG spillage. In three patients the dye did not progress from the Hartmann’s pouch to the cystic duct, probably due to stone obstruction of the cystic duct (see Fig. 2).
Discussion
In the recent years we have witnessed an exponential growth of the uses and applications of ICG, making it nowadays a widespread intraoperative navigation tool. With this series of patients we describe the feasibility and easy application of this novel approach to NIRC using ICG injected directly into the gallbladder to visualize the biliary anatomy. Although previously performed in a porcine model [13] and in short human series [8], we believe it is still a fairly new technique with a great potential (Fig. 3).
This approach confers several advantages compared with traditional IOC: it avoids the use of radiation; it does not extend operative time, allows real-time visualization of the anatomy while operating, and can be performed entirely by the lead surgeon without additional staff [8]. Moreover, the direct injection of ICG into the gallbladder has also the advantage that the technique is performed easily even by trainees; it allows a immediate and real-time visualization of how the gallbladder is filled, then the CD is delimited and in occasions the biliary tract is visualized. Most of biliary duct lesions occur during dissection of the CD area, because of a misinterpretation of the anatomy [4]. For IOC, CD dissection is mandatory to correctly perform the technique, whereas ICG is injected prior to any dissection, making it hypothetically less likely to cause a biliary lesion. Direct injection of ICG into the cystic duct would be also feasible, using the traditional approach of IOC, but it would be technically as demanding, and probably injuries or spillage of ICG would be more frequent. With these short series of cholecystectomies in a planned setting it is not possible to demonstrate any changes of incidence of biliary lesions; further research in the future is needed to assess it. On the other hand, IOC enables to visualize the entire biliary tree anatomy, which we have not achieved with the ICG technique.
Direct gallbladder injection provides two important advantages compared with intravascular injection: it provides immediate visualization of the biliary anatomy and clarifies the dissection plane between the gallbladder and the liver bed. Thus, puncturing the gallbladder with a veress needle offers the best balance between technical simplicity and usefulness, only requiring closing the defect of the puncture site with a suture or clip. Moreover, when the gallbladder is too full to be managed properly, partial emptying of the gallbladder’s bile is not infrequent; injecting at this point ICG is completely integrated into the surgical act. By improving visualization of the extrahepatic biliary structures, a possible bile duct injury could be avoided without compromising the efficiency of the procedure.
A problem related to the intravenous ICG NIRC method is determining the dose and the timing when it should be administered. The time to excrete ICG into the bile may vary from patient to patient. According to the literature, the usual technique consists of diluting a 25-mg bottle of ICG with 10 mL of sterile water. In a planned cholecystectomy, 6 mL are injected of the ICG solution, between 6 and 10 h before the surgery (8). There are studies proposing different doses like 2.5 mg, 5 mg, or 10 mg administered within 1 h before imaging and up to 25 h before the procedure [4]. The disparity in timing and ideal dosage is so big that actually, a European registry about NIRC has been created [14]. Moreover, this technique is difficult to be used in emergency settings due to lack of foresight of the surgery timings as procedures are not scheduled. This is also a difficulty encountered by planned cholecystectomies that are carried out without admission; where it can be challenging to organize the ICG administration with enough time in advance. Another, disadvantage of intravenous ICG NIRC, apart from the previously mentioned, is that liver fluorescence in the background can distort or difficult the correct visualization of the biliary anatomy.
On the other hand, one disadvantage encountered for NIRC with direct injection into the gallbladder is that in the case of puncturing the gallbladder through/or spilling the ICG the visualization of the anatomic structures was affected. Also, the dye did not progress into the cystic duct due to abundant cholelithiasis, but this would have been a problem in intravenous ICG injection as well. The penetration of the light with a wavelength near the infrared makes it possible to see structures stained by ICG up to 1 cm in depth, but in our series we have not seen any influence by BMI.
Although special equipment is required for this procedure, NIR light mode is nowadays integrated into most of the laparoscopy towers. Because our technique confines the ICG to the biliary system a dilute solution of the ICG should be used. Studies suggest that an ICG solution of 0.025 mg/mL is ideal for biliary imaging [15, 16]. We used bile to make a final solution of ICG because it binds to the bile proteins conferring a better dissolution rate and better optical results [17, 18].
Changing back and forth standard light and NIR light modes was not a major issue; thus, changing of visualization modes is almost immediate. Moreover, new cameras are coming up in the market that integrate the two vision modes simultaneously, so we hypothesize that in the near future it can become even more comfortable to operate with the guidance of ICG. Fluorescence of the cystic duct and common bile duct gives an extra level of confidence to the surgeon dissecting the critical view of safety, especially in the case of inflammation or aberrant anatomy. The cystic artery is not illuminated by this technique, but the contrast between it and the fluorescent gallbladder is usually enough to identify it.
The cost of implementation of this method has not been analyzed in this paper, but so far, some studies indicate it is not expensive. One powdered vial of ICG costs $25 [19]. To this we should add the cost of the NIR tower, but as mentioned before, most of the laparoscopic towers have this light mode integrated already. This supports the idea that this method can be performed on a routine of daily basis given that the cost of the dye is low. We do not believe NIRC with ICG can fully substitute the IOC or other techniques to avoid biliary lesions, but it can be performed routinely as we have found it to have no major complications and it does not consume extra-time. Its implementation on a daily basis, we believe, outweighs by far the cost when it can help us avoid a feared biliary injury.
In conclusion, NIRC is a feasible method that is not time-consuming; it does not require a different learning curve from standard laparoscopic cholecystectomies and has no major complications described so far. We strongly believe that it could be of interest for the scientific community to further research in this field in order to investigate and prove the role of routine NIRC with direct injection of ICG into the gallbladder in laparoscopic cholecystectomies.
References
Pucher PH, Brunt LM, Fanelli RD, Asbun HJ, Aggarwal R (2015) SAGES expert Delphi consensus: critical factors for safe surgical practice in laparoscopic cholecystectomy. Surg Endosc 29:3074–3085. https://doi.org/10.1007/s00464-015-4079-z
Ministerio de Sanidad Servicios Sociales e Igualdad. Actividad y Calidad de los Servicios Sanitarios, informe anual del SNS 2017. 2018;1–77. Available from: https://www.mscbs.gob.es/estadEstudios/estadisticas/sisInfSanSNS/tablasEstadisticas/InfAnualSNS2017/5_CAP_17.pdf
Hogan NM, Dorcaratto D, Hogan AM, Nasirawan F, McEntee P, Maguire D, Geoghegan J, Traynor O, Winter DC, Hoti E (2016) Iatrogenic common bile duct injuries: increasing complexity in the laparoscopic era: a prospective cohort study. Int J Surg 33:151–156. https://doi.org/10.1016/j.ijsu.2016.08.004
Boogerd LSF, Handgraaf HJM, Huurman VAL, Lam HD, Mieog JSD, Van Der Made WJ et al (2017) The best approach for laparoscopic fluorescence cholangiography: overview of the literature and optimization of dose and dosing time. Surg Innov 24:386–396. https://doi.org/10.1177/1553350617702311
Strasberg SM (2002) Avoidance of biliary injury during laparoscopic chelocystectomy. J Hepato-Biliary-Pancreat Surg 9:543–547. https://doi.org/10.1007/s005340200071
Conrad C, Wakabayashi G, Asbun HJ, Dallemagne B, Demartines N, Diana M, Fuks D, Giménez ME, Goumard C, Kaneko H, Memeo R, Resende A, Scatton O, Schneck AS, Soubrane O, Tanabe M, van den Bos J, Weiss H, Yamamoto M, Marescaux J, Pessaux P (2017) IRCAD recommendation on safe laparoscopic cholecystectomy. J Hepatobil Pancreat Sci 24:603–615. https://doi.org/10.1002/jhbp.491
Lammert F, Acalovschi M, Ercolani G, van Erpecum KJ, Gurusamy KS, van Laarhoven CJ et al (2016) EASL Clinical Practice Guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol 65:146–181. https://doi.org/10.1016/j.jhep.2016.03.005
Boni L, David G, Mangano A, Dionigi G, Rausei S, Spampatti S, Cassinotti E, Fingerhut A (2015) Clinical applications of indocyanine green (ICG) enhanced fluorescence in laparoscopic surgery. Surg Endosc 29:2046–2055. https://doi.org/10.1007/s00464-014-3895-x
Graves C, Ely S, Idowu O, Newton C, Kim S (2017) Direct gallbladder Indocyanine green injection fluorescence cholangiography during laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech 27:1069–1073. https://doi.org/10.1089/lap.2017.0070
Araki K, Namikawa K, Mizutani J, Doiguchi M, Yamamoto H, Arai H, Yamaguchi T, Ido Y, Uno K, Hayashi N (1992) Indocyanine green staining for visualization of the biliary system during laparoscopic cholecystectomy [3]. Endoscopy. 24:803. https://doi.org/10.1055/s-2007-1010592
Pesce A, Piccolo G, La Greca G, Puleo S (2015) Utility of fluorescent cholangiography during laparoscopic cholecystectomy: a systematic review. World J Gastroenterol 21:7877–7883. https://doi.org/10.3748/wjg.v21.i25.7877
Vlek SL, van Dam DA, Rubinstein SM, de Lange-de Klerk ESM, Schoonmade LJ, Tuynman JB, Meijerink WJHJ, Ankersmit M (2017) Biliary tract visualization using near-infrared imaging with indocyanine green during laparoscopic cholecystectomy: results of a systematic review. Surg Endosc 31:2731–2742. https://doi.org/10.1007/s00464-016-5318-7
Liu YY, Kong SH, Diana M, Lègner A, Wu CC, Kameyama N, Dallemagne B, Marescaux J (2016) Near-infrared cholecysto-cholangiography with indocyanine green may secure cholecystectomy in difficult clinical situations: proof of the concept in a porcine model. Surg Endosc 30:4115–4123. https://doi.org/10.1007/s00464-015-4608-9
Agnus V, Pesce A, Boni L, Van Den Bos J, Morales-Conde S, Paganini AM et al (2019) Fluorescence-based cholangiography: preliminary results from the IHU-IRCAD-EAES EURO-FIGS registry. Surg Endosc 34:3888–3896. https://doi.org/10.1007/s00464-019-07157-3
Mitsuhashi N, Kimura F, Shimizu H, Imamaki M, Yoshidome H, Ohtsuka M, Kato A, Yoshitomi H, Nozawa S, Furukawa K, Takeuchi D, Takayashiki T, Suda K, Igarashi T, Miyazaki M (2008) Usefulness of intraoperative fluorescence imaging to evaluate local anatomy in hepatobiliary surgery. J Hepato-Biliary-Pancreat Surg 15:508–514. https://doi.org/10.1007/s00534-007-1307-5
Liu YY, Liao CH, Diana M, Wang SY, Kong SH, Yeh CN, Dallemagne B, Marescaux J, Yeh TS (2018) Near-infrared cholecystocholangiography with direct intragallbladder indocyanine green injection: preliminary clinical results. Surg Endosc 32:1506–1514. https://doi.org/10.1007/s00464-017-5838-9
Ishizawa T, Fukushima N, Shibahara J, Masuda K, Tamura S, Aoki T, Hasegawa K, Beck Y, Fukayama M, Kokudo N (2009) Real-time identification of liver cancers by using indocyanine green fluorescent imaging. Cancer. 115:2491–2504. https://doi.org/10.1002/cncr.24291
Ishizawa T, Saiura A, Kokudo N (2016) Clinical application of indocyanine green-fluorescence imaging during hepatectomy. HepatoBiliary Surg Nutr. https://doi.org/10.21037/hbsn.2015.10.01
Dip F, Falco J, Montesinos MR, De La Fuente M, Rosenthal RJ (2016) Cost-effective analysis of near infrared (NIR) vs radiotracer for sentinel lymph node biopsy in breast cancer. J Am Coll Surg 223:e3. https://doi.org/10.1016/j.jamcollsurg.2016.08.010
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Clara Gené Škrabec and Fernando Pardo Aranda. The first draft of the manuscript was written by Clara Gené Škrabec, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
This prospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data and photographs.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(JPEG 383 kb)
Rights and permissions
About this article
Cite this article
Gené Škrabec, C., Pardo Aranda, F., Espín, F. et al. Fluorescent cholangiography with direct injection of indocyanine green (ICG) into the gallbladder: a safety method to outline biliary anatomy. Langenbecks Arch Surg 405, 827–832 (2020). https://doi.org/10.1007/s00423-020-01967-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-020-01967-z