Abstract
Background
The open abdomen has become an accepted treatment option of critically ill patients with severe intra-abdominal conditions. Fascial closure is a particular challenge in patients with peritonitis. This study investigates whether fascial closure rates can be increased in peritonitis patients by using an algorithm that combines vacuum-assisted wound closure and mesh-mediated fascial traction. Moreover, fascial closure rates for patients with peritonitis, trauma or abdominal compartment system (ACS) are compared.
Methods
Data were collected prospectively from all patients who underwent open abdomen management at our institution from 2006 to 2012. All patients were treated under a standardised algorithm that combines vacuum-assisted closure and mesh placement at the fascial level.
Results
During the study period, 53 patients (mean age 53 years) underwent open abdomen management for a mean duration of 15 days. Indications for leaving the abdomen open were peritonitis (51 %), trauma (26 %), and ACS or abdominal wall dehiscence (23 %). The fascial closure rate was 79 % in an intention-to-treat analysis and 89 % in a per-protocol analysis. Mortality was 13 %. No patient developed an enteroatmospheric fistula or abdominal wall dehiscence after closure. The mean duration of treatment was significantly longer in peritonitis patients (20 days) than in patients without peritonitis (10 days) (p = 0.03). There were no significant differences in fascial closure rates between patients with peritonitis (87 %), trauma (85 %), and ACS or abdominal wall dehiscence (100 %) (p = 0.647).
Conclusions
Regardless of the underlying pathology, high fascial closure rates can be achieved using a combination of vacuum-assisted closure and mesh-mediated fascial traction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Open abdominal treatment has become an accepted treatment option of critically ill patients with severe intra-abdominal conditions [1–3]. The most frequent indications for leaving the abdomen open are abdominal trauma, peritonitis, acute pancreatitis and abdominal compartment syndrome (ACS) [4–6].
In recent years, laparostomy management has gone through various evolutions, and a wide variety of technical modifications have been introduced [7–10]. The focus of attention is on optimising factors of critical importance for the success of open abdomen management and on preventing complications and long-term adverse effects [3, 9, 11].
In the past, planned ventral hernia was good clinical practice [12]. More recently, however, the focus of treatment has shifted towards achieving delayed primary fascial closure as early as possible during hospitalisation [13].
The reasons for this are twofold. First, fascial closure during the hospital stay was found to reduce treatment complications [14, 15]. For this reason, Scott et al. advocate an early aggressive closure of the open abdomen [3]. Second, delayed primary fascial closure has the advantage that patients do not have to experience a temporary loss of physical integrity and do not have to undergo abdominal wall reconstruction, which involves a number of risks that should not be underestimated [10, 16, 17].
Fascial retraction was found to start as early as about 3 days after surgery and results in a progressively larger gap in the fascia [12, 18]. The recent literature suggests that early fascial closure should ideally be achieved within 10 days [19, 20].
Since the introduction of vacuum techniques for the management of an open abdomen, the application of negative pressure for this purpose has been gaining in popularity and has led to a paradigm shift. Today, vacuum techniques are most widely used for temporary abdominal closure not only in Germany but in other countries as well [7, 21, 22]. Negative pressure therapy leads to continuous exudate removal, prevents the accumulation of fluid in the abdomen and reduces the rate of abscess formation [20, 23]. In addition, it progressively reduces oedema, improves intestinal perfusion and shows a low fistula rate when used in combination with an inert plastic sheet that is placed in contact with the viscera [11, 20, 24].
Vacuum-assisted closure systems alone, however, cannot prevent fascial retraction [25]. The literature reports substantial differences in fascial closure rates that can be achieved with vacuum techniques alone. These rates range between 30 % [26] and 72 % [27] with an average of 60 % [21] (Table 1). Especially in the case of patients with peritonitis and patients requiring long treatment courses, negative pressure applications alone cannot achieve satisfactory fascial closure rates [20, 25]. In patients with peritonitis and difficult or delayed control of infection, the fascial closure rate was found to decrease significantly when the open abdomen was managed only by vacuum-assisted closure [28].
For this reason, the application of negative pressure and its undisputed advantages must be combined with another technique that facilitates approximation of the fascia in an attempt to achieve synergistic effects of oedema reduction and fascial traction and to increase the rate of delayed primary fascial closure [13, 29].
A number of promising techniques have been described in the literature which combine the application of negative pressure with fascial sutures, alloplastic mesh, the Wittmann patch or the Abdominal Reapproximation Anchor System (ABRA) [7–9, 13, 30]. In the absence of randomised controlled studies, further clinical observational studies are required in order to provide a high level of evidence for the effectiveness of the various techniques [31].
Our algorithm for managing the open abdomen combines vacuum-assisted closure and mesh-mediated fascial traction (VAWCM). When the first reoperation (second-look procedure) is performed, Vicryl mesh is placed over the visceral protective layer at the fascial level. This mesh prevents fascial retraction and facilitates the gradual approximation of the fascial edges at each reoperation until a direct suture can be performed. In this study, we evaluate this technique for the open abdomen in terms of fascial closure rates and possible complications. Since the management of young trauma patients is usually associated with high fascial closure rates [22, 29, 32], we were particularly interested in assessing whether a satisfactory fascial closure rate can also be achieved in elderly patients who present with marked peritonitis and require a long period of treatment [33]. Peritonitis patients were reported to have considerably lower fascial closure rates than trauma patients [21, 28, 33–35]. In addition, the duration of the open abdomen was found to be an independent risk factor influencing fascial closure [8, 20, 28, 29].
Material and methods
Patients and data collection
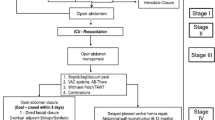
Data were collected prospectively from consecutively enrolled patients who underwent open abdomen management from 2006 to 2012 at the Department of General, Visceral and Thoracic Surgery of the German Armed Forces Central Hospital of Koblenz. All patients or their legal representatives gave their written informed consent. Patients whose treatment had been initiated at another hospital were excluded. Accordingly, the only patients who were included had been treated in accordance with the Koblenz algorithm for managing the open abdomen [11] (Fig. 1) from initial laparotomy until abdominal closure. Data for each patient were collected in a standardised manner including the following variables:
-
Biometric data (age, gender, height, weight)
-
Admission diagnosis
-
Additional diagnoses
-
Risk factors (use of anticoagulants, use of immunosuppressant medication, smoking)
-
Indication for open abdomen management
-
Number of surgical procedures/number of dressing changes from initial operation to abdominal closure
-
Duration of the open abdomen
-
Delayed primary fascial closure
-
Mortality during open abdomen treatment/hospital mortality
-
Complications associated with the procedure (formation of abscesses, enteroatmospheric fistulas and hernias) according to the Clavien-Dindo classification [36–38]
-
Systemic complications (pneumonia, respiratory tract infections, urinary tract infections, pulmonary embolism, myocardial infarction, acute renal insufficiency)
Technique for the open abdomen
All patients had been treated in accordance with the Koblenz algorithm for managing the open abdomen [11] (Fig. 1). This algorithm was implemented in January 2006. From 2006 to 2011, the VAC® abdominal dressing system from KCI (Kinetic Concepts Inc., San Antonio, TX, USA) was placed at the initial laparotomy. In 2012, KCI replaced this dressing system with the ABThera® Sensa T.R.A.C.® system, which has been applied at our institution since then. When the dressing is changed for the first time, i.e. within the first 48 to 72 h, the operating surgeon makes the decision whether to close the abdomen or to continue the open abdomen treatment based on the criteria edema reduction, lack of infection and tension.
If it becomes apparent that early primary closure is inadvisable or impossible, a Vicryl® (polyglactin 910) mesh (Ethicon, Norderstedt, Germany) is placed on the viscera as a temporary inlay in order to facilitate the gradual approximation of the fascial edges (mesh-mediated fascial traction). When we introduced our algorithm in January 2006, we used the term “mesh-induced fascial approximation” (MIFA) to describe this technique. The technique is similar to what is known as vacuum-assisted wound closure and mesh-mediated fascial traction (VAWCM), which was described for the first time by Petersson et al. in 2007 [39]. The objective of mesh placement is to prevent fascial retraction and to achieve high rates of delayed primary closure. In a first step, a polyethylene sheet, which is one of the components of the KCI dressing systems and serves as a protective layer, is cut to size and inserted into the abdominal cavity in such a way that the intestines are completely covered. The purpose of this layer is to completely prevent contact between the mesh and the viscera and to minimise contact between the viscera and the abdominal wall. A piece of Vicryl® mesh is then divided into two halves that are sutured to the fascial edges with running #0 Vicryl® sutures on each side and sutured together in the middle (Fig. 2). Subcutaneous foam is placed on the Vicryl® mesh and continuous negative pressure of 75–100 mmHg is applied. The level of negative pressure is reduced in patients with an increased risk of bleeding and can be as low as 25 mmHg. At the second dressing change, the Vicryl® mesh is opened in the middle. The protective layer is removed through the opening and the revision is performed. As far as the volume of the intra-abdominal contents and intra-abdominal pressure permit, the edges of the mesh are excised and the mesh is resutured with a running #0 Vicryl® suture under moderate tension. This technique enables the surgeon to progressively reduce the fascial gap (Figs. 3 and 4). When the fascial edges can be reapproximated during a revision procedure and open abdominal management can be completed, the mesh is removed and delayed primary fascial closure is performed. In the case of unfavourable fascial conditions, strips of mesh may be left in place in order to augment the fascia and support the suture line. If there is macroscopic evidence of compromised local wound healing, a subcutaneous vacuum-assisted closure system should be placed. If there is objective evidence of a clean wound, the skin can be closed.
Data analysis
Data on fascial closure, open abdomen duration, the number of dressing changes, the incidence of fistula formation and mortality were collected for all patients in this study and analysed in a descriptive manner. Depending on the indication for open abdomen management, three groups of patients were formed (peritonitis patients, trauma patients, and patients with abdominal compartment syndrome or abdominal wall dehiscence). These groups were analysed separately and assessed for significant differences in the aforementioned variables. The peritonitis group included all patients with secondary peritonitis resulting from the perforation of a hollow organ, postoperative anastomotic insufficiency or necrotising pancreatitis. The trauma group consisted of patients who underwent open abdomen management for abdominal trauma. Abdominal compartment syndrome was classified in accordance with the World Society of the Abdominal Compartment Syndrome consensus definitions [40]. Intra-abdominal pressure was measured intermittently in fully relaxed patients using a urinary catheter and the Foley manometer technique [41]. All patients with a clinically relevant postoperative fascial dehiscence were included in the group of patients with ACS or abdominal wall dehiscence.
The Wilcoxon-Mann-Whitney test was used for comparing two groups. The Kruskal-Wallis test was used for comparing three groups. Primary fascial closure rates were analysed on the basis of intention to treat and per protocol since the failure to achieve delayed primary closure was, of course, closely associated with mortality before fascial closure. The level of significance was set at p < 0.05. Statistical analyses were performed using SPSS Statistics 22.0® (SPSS Inc., Chicago, IL, USA).
Results
Biometry
During the study period, 53 patients underwent open abdomen management in the Department of General, Visceral and Thoracic Surgery at the German Armed Forces Central Hospital in accordance with our algorithm, which includes a combination of vacuum-assisted wound closure and mesh-mediated fascial traction (VAWCM). These patients included 16 women (30.2 %) and 37 men (69.8 %) with a mean age of 53 years (±16.9 years) at the beginning of treatment. The youngest patient was 20 years old; the oldest patient was 85 years old.
Underlying conditions
The most common underlying conditions necessitating hospital treatment were malignancies and trauma, which were noted in more than 50 % of the patients, followed by diverticulitis, mechanical bowel obstruction and chronic inflammatory bowel diseases. All underlying diagnoses are shown in Table 2.
Indications for open abdomen management
The initial indication for open abdomen management was secondary peritonitis and necrotizing pancreatitis in 27 patients (51 %). In 14 patients with trauma (26.4 %), the abdomen was left open for damage control and second-look procedures. In the remaining 12 patients (22.6 %), laparostomy was indicated for abdominal compartment syndrome (7 patients) or postoperative abdominal wall dehiscence (5 patients).
Fascial closure
The algorithm described in this study enabled us to achieve delayed primary fascial closure in 42 of the 47 survivors. This corresponds to a fascial closure rate of 89.4 % in a per-protocol analysis. When the patients who died during their hospital stay were included, the rate was 79.3 % (42 of 53 patients) in an intention-to-treat analysis. The fascias were successfully closed in all surviving patients with abdominal compartment syndrome or abdominal wall dehiscence. The closure rates were lower in the other two groups, i.e. 87 % (20 of 23 patients) in the peritonitis group and 85 % (11 of 13 patients) in the trauma group (Fig. 5). The differences in fascial closure rates were not significant (p = 0.647). The initial fascial gap was 16.3 ± 4.6 cm. The fascial closure rate was not affected by the size of the initial defect (p > 0.05).
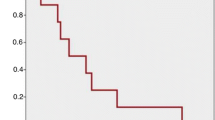
Duration of the open abdomen
The mean duration of open abdomen management was 15 days (Table 3 and Fig. 6). There were considerable differences in the duration of treatment when the different indications for open abdomen management with vacuum-assisted wound closure and mesh-mediated fascial traction were analysed. The mean duration of treatment in the peritonitis group and was thus twice as long as in the groups that required open abdomen management for trauma, ACS or abdominal wall dehiscence (p = 0.03).
The duration of the open abdomen had no significant influence on the success or failure of fascial closure. In the groups of patients whose abdomen was left open for a maximum period of 10 days, the fascial closure rate was 96 % in the per-protocol analysis and 82.7 % in the intention-to-treat analysis. In the group of patients who required open abdomen treatment for more than 10 days, the fascial closure rate was 81.8 % in the per-protocol analysis and 75 % in the intention-to-treat analysis (p > 0.05 for both types of analysis).
Number of procedures
The mean number of procedures (placement of a dressing, dressing changes and operation for abdominal closure) until completion of open abdomen management was 6.2 for all patients (Table 3). Similar to the analysis of the three groups by the duration of treatment, the peritonitis group required a significantly higher mean number of procedures (7.9) than the trauma group (4.8) and the group of patients with ACS or abdominal wall dehiscence (4.2) (p = 0.038).
The interval between procedures was 2.8 days for the total patient population. There was no major difference between the groups. The interval was 2.8 days in the peritonitis group, 2.6 days in the trauma group and 3.1 days in the group of patients with ACS or abdominal wall dehiscence (p > 0.05).
Complication rates and mortality
Seven (13 %) of the 53 patients died during hospitalisation, six of whom (11 %) died during open abdomen management. The cause of death was sepsis and multi-organ failure as a result of peritonitis in five cases and cardiopulmonary insufficiency that was not associated with a septic process in the other cases. No enteroatmospheric fistulas were seen. One patient required reopening of the abdomen for recurrent ACS after initial fascial closure and again underwent open abdomen management. Fascial closure was achieved in this case after two further dressing changes. No patient developed fascial dehiscence or intra-abdominal abscess during hospitalisation. Wound healing problems were noted in nine patients (17 %). Five of these patients (9.4 %) experienced Clavien-Dindo grade I complications and underwent open-wound treatment without secondary suture. The other 4 patients (7.5 %) developed Clavien-Dindo Grade IIIb complications and were managed by secondary suture after open-wound treatment.
Discussion
The techniques that are currently available for managing the open abdomen are continuously being improved. In recent years, the literature has shown that a standardised approach with a focus on two key objectives, i.e. to reduce the rate of fistulas and to achieve fascial closure, can apparently minimise the risks and optimise the benefits of the technique used [1, 6, 8, 11]. The objectives of treatment are to achieve high fascial closure rates and at the same time to prevent the formation of small bowel fistulas and large ventral hernias [31]. Small bowel fistulas can be reduced, if not completely eliminated, by protecting the intestinal serosa and covering the viscera with an inert plastic sheet and by using an atraumatic surgical technique [11, 20, 42]. The highest fascial closure rates can be achieved with combinations of a vacuum technique and mechanical approximation of the fascias [1]. Whereas vacuum techniques alone can achieve mean delayed primary fascial closure rates of 60 % (Table 1), a combination of vacuum-assisted closure and alloplastic mesh or sutures leads to considerably higher closure rates [8, 15, 32, 43, 44]. Our algorithm includes the placement of Vicryl® mesh at the fascial level as a temporary inlay. During every reoperation, the size of the mesh can be reduced and the fascial edges can be approximated until a direct fascial suture is possible (Fig. 1). This technique allows for early fascial closure, as advocated by Scott et al. [3] because the rate of complications increases with the duration of treatment [12, 23, 45, 46]. Moreover, delayed primary fascial closure prevents the formation of large or even giant ventral hernias that require complex reconstructive procedures and are associated with considerable risks [17, 47].
In the literature, fascial closure rates are usually evaluated using per-protocol data since mortality is closely associated with the failure to achieve fascial closure. We deliberately provide both rates. In recent years, a variety of promising techniques have been described in the literature which is based on mechanical fascial traction [2, 6, 15, 32, 39, 43]. The fascial closure rates that we achieved in our patient population (89.4 % in the per-protocol analysis and 79.3 % in the intention-to-treat analysis) are in the upper range of rates reported in the literature [8, 15, 32, 43, 44] and are thus considerably higher than those achieved with vacuum techniques alone [25, 26].
A subgroup analysis shows that there is no difference in fascial closure rates between peritonitis patients and patients with trauma or ACS. Contrary to what has been reported in previous publications, satisfactory fascial closure rates can thus be achieved with the technique described here even in the complex group of peritonitis patients [20, 25, 28]. Moreover, the duration of open abdomen management was not a significant risk factor for failure to achieve fascial closure. We did not observe a significant decrease in the fascial closure rates for peritonitis patients since our treatment approach prevented fascial retraction, which is associated with longer durations of treatment. Padalino et al. reported that vacuum-assisted closure alone had a positive effect on fascial closure in patients with peritonitis [28].
In contrast to the techniques described by Koss et al. and Pliakos et al., who closed the fascias with sutures, the algorithm presented here provides maximum protection to the vulnerable fascia [13, 48]. The mesh is sutured to the fascia only once and is reduced in size in the middle so that the fascia is spared until definitive closure.
The fascial closure rates reported here are comparable to those that can be achieved with similar techniques using VAWCM [6, 8]. Comparability is, however, limited by differences in patient populations. Acosta et al., for example, studied a group of patients including vascular surgery patients (40 %) and only few trauma patients (8 %) [8].
Unlike Petersson et al. who described the VAWCM [39] technique for the first time in 2007 and who use polypropylene mesh, we place polyglactin 910 (Vicryl®) mesh on the viscera. Our technique allows us to leave a strip of mesh in place and thus to augment the fascial edges during delayed primary closure in order to support the suture line and prevent sutures from tearing through tissue. If the protective layer becomes dislodged, this type of mesh is also associated with a lower risk of the formation of small bowel fistulas at the site where the mesh comes into contact with the viscera [26, 49]. Vicryl® mesh is one of the least expensive alloplastic materials and is relatively cost-effective especially when early or delayed primary closure can be achieved, and thus, further procedures and the costs of possible complications can be reduced or avoided.
In contrast to other authors who report fistula rates as high as 21 %, we did not observe any enteroatmospheric fistulas, which can be regarded as the most severe complication of the open abdomen [6, 8, 26].
Compared with the existing literature, the mean duration of open abdomen management was relatively short in our patient groups [28, 39, 44]. For example, the mean duration of treatment was 32 days in a study by Petersson et al. and only 15 days in our patient population [39]. The median was as low as 10 days in our study. Hospital mortality in our patient population (13 %) was in the lower range of rates reported in other studies [6, 8, 13, 26]. In a study by Rasilainen et al., 35.6 % of patients died during hospitalisation [6].
In the literature, two groups of patients are distinguished, i.e. patients in whom fascial closure is achieved and open abdomen management can be completed within the first 10 days, and patients in whom fascial closure cannot be obtained within this period of time for a variety of reasons [20]. Whereas an early closure and high fascial closure rates can usually be achieved in trauma patients, peritonitis patients often require longer durations of treatment [6, 33, 50]. In several studies, the duration of open abdomen treatment was identified as a risk factor for failure to achieve fascial closure [8, 20, 29]. In keeping with the existing literature, our patients with peritonitis needed a significantly longer duration of treatment than patients with trauma or ACS. In addition, they required a significantly higher number of procedures. Unlike the previous literature, however, the use of mesh-mediated fascial traction enabled us to achieve a fascial closure rate similar to that obtained for the other patients in spite of different aetiologies and significantly different durations of treatment [6]. There were only a few failures in our patient groups. Future studies should further investigate these failures and identify risk factors that prevent delayed primary closure from being achieved despite the use of both a vacuum technique and fascial traction. At our institution, these patients are discharged with a ventral hernia and return after 9 to 12 months for secondary abdominal wall reconstruction, which usually consists of mesh-augmented hernia repair using the sublay technique with or without component separation according to Ramirez et al. [51]. The literature describes a variety of promising procedures that can be used to prevent the formation of large or even giant ventral hernias in patients in whom mesh-mediated fascial traction failed. Dietz et al., for example, proposed a four-stage procedure including the placement of a two-component mesh in an intraperitoneal only position (IPOM) for bridging fascial defects and reported low rates of complications [10]. Ferguson et al. managed these patients with a components separation technique in order to achieve delayed primary closure during initial hospitalisation [52].
The discussion above shows that the direct comparability of the various techniques and modifications is currently limited by the heterogeneity of study populations, technical variations and results.
Conclusion
The results of our study show that the open abdomen management technique presented here prevents fascial retraction and at the same time decreases oedema with vacuum-assisted wound closure so that the size of the mesh can be reduced and the fascial edges can be approximated during every reoperation until direct fascial closure is obtained. Synergistic effects of vacuum-induced oedema reduction and mesh-mediated fascial traction are thus achieved in an ideal manner.
Regardless of the underlying aetiology and the duration of open abdomen management, delayed primary fascial closure is possible in a large number of cases. A high rate of fascial closure can be achieved especially in the complex group of peritonitis patients who usually require relatively long durations of treatment.
A follow-up study of these patients is necessary in order to assess long-term results and in particular hernia rates.
The comparability of available studies on techniques for managing the open abdomen is usually limited by the heterogeneity of patient populations, techniques and study designs. For this reason, the level of evidence currently available makes it impossible to provide recommendations and guidelines for the management of the open abdomen [53]. In the medium term, the implementation of an Open Abdomen Registry, which will prospectively collect data about open abdomens, is likely to provide a valuable source of evidence-based information.
References
Open Abdomen Advisory Panel, Campbell A, Chang M et al (2009) Management of the open abdomen: from initial operation to definitive closure. Am Surg 75(11 Suppl):S1–S22
Burlew CC (2012) The open abdomen: practical implications for the practicing surgeon. Am J Surg 204(6):826–835
Scott BG, Welsh FJ, Pham HQ et al (2006) Early aggressive closure of the open abdomen. J Trauma 60(1):17–22
Diaz JJ, Cullinane DC, Dutton WD et al (2010) The management of the open abdomen in trauma and emergency general surgery: part 1—damage control. J Trauma 68(6):1425–1438
Smith BP, Adams RC, Doraiswamy VA et al (2010) Review of abdominal damage control and open abdomens: focus on gastrointestinal complications. J Gastrointest Liver Dis 19(4):425–435
Rasilainen SK, Mentula PJ, Leppäniemi AK (2012) Vacuum and mesh-mediated fascial traction for primary closure of the open abdomen in critically ill surgical patients. Br J Surg 99(12):1725–1732
Quyn AJ, Johnston C, Hall D et al (2012) The open abdomen and temporary abdominal closure systems—historical evolution and systematic review. Colorectal Dis 14(8):e429–e438
Acosta S, Bjarnason T, Petersson U et al (2011) Multicentre prospective study of fascial closure rate after open abdomen with vacuum and mesh-mediated fascial traction. Br J Surg 98(5):735–743
Verdam FJ, Dolmans DE, Loos MJ et al (2011) Delayed primary closure of the septic open abdomen with a dynamic closure system. World J Surg 35(10):2348–2355
Dietz UA, Wichelmann C, Wunder C et al (2012) Early repair of open abdomen with a tailored two-component mesh and conditioning vacuum packing: a safe alternative to the planned giant ventral hernia. Hernia 16(4):451–460
Willms A, Güsgen C, Schreyer C, Becker HP, Schwab R (2011) Prevention of small bowel fistulas during open abdominal treatment: lessons learned. Zentralbl Chir 136(6):592–597
Scott BG, Feanny MA, Hirshberg A (2005) Early definitive closure of the open abdomen: a quiet revolution. Scand J Surg 94(1):9–14
Pliakos I, Papavramidis TS, Mihalopoulos N et al (2010) Vacuum-assisted closure in severe abdominal sepsis with or without retention sutured sequential fascial closure: a clinical trial. Surgery 148(5):947–953
Hatch QM, Osterhout LM, Podbielski J et al (2011) Impact of closure at the first take back: complication burden and potential overutilization of damage control laparotomy. J Trauma 71(6):1503–1511
Miller RS, Morris JA, Diaz JJ, Herring MB, May AK (2005) Complications after 344 damage-control open celiotomies. J Trauma 59(6):1365–1371, discussion 1371–4
Joels CS, Vanderveer AS, Newcomb WL et al (2006) Abdominal wall reconstruction after temporary abdominal closure: a ten-year review. Surg Innov 13(4):223–230
Pantelis D, Jafari A, Vilz TO et al (2012) Abdominal wall components separation method for closure of complicated abdominal hernias. Chirurg 83(6):555–560
Smith LA, Barker DE, Chase CW et al (1997) Vacuum pack technique of temporary abdominal closure: a four-year experience. Am Surg 63(12):1102–1107, discussion 1107–8
López-Cano M, Pereira JA, Armengol-Carrasco M (2013) “Acute postoperative open abdominal wall”: nosological concept and treatment implications. World J Gastrointest Surg 5(12):314–320
Regner JL, Kobayashi L, Coimbra R (2012) Surgical strategies for management of the open abdomen. World J Surg 36(3):497–510
van Hensbroek BP, Wind J, Dijkgraaf MG et al (2009) Temporary closure of the open abdomen: a systematic review on delayed primary fascial closure in patients with an open abdomen. World J Surg 33(2):199–207
Barker DE, Green JM, Maxwell RA et al (2007) Experience with vacuum-pack temporary abdominal wound closure in 258 trauma and general and vascular surgical patients. J Am Coll Surg 204(5):784–792, discussion 792–3
Stevens P (2009) Vacuum-assisted closure of laparostomy wounds: a critical review of the literature. Int Wound J 6(4):259–266
Banwell PE, Musgrave M (2004) Topical negative pressure therapy: mechanisms and indications. Int Wound J 1(2):95–106
Wondberg D, Larusson HJ, Metzger U, Platz A, Zingg U (2008) Treatment of the open abdomen with the commercially available vacuum-assisted closure system in patients with abdominal sepsis: low primary closure rate. World J Surg 32(12):2724–2729
Bee TK, Croce MA, Magnotti LJ et al (2008) Temporary abdominal closure techniques: a prospective randomized trial comparing polyglactin 910 mesh and vacuum-assisted closure. J Trauma 65(2):337–342, discussion 342–4
Oetting P, Rau B, Schlag PM (2006) Abdominal vacuum device with open abdomen. Chirurg 77(7):586, 588–93
Padalino P, Dionigi G, Minoja G et al (2010) Fascia-to-fascia closure with abdominal topical negative pressure for severe abdominal infections: preliminary results in a department of general surgery and intensive care unit. Surg Infect (Larchmt) 11(6):523–528
Dubose JJ, Scalea TM, Holcomb JB et al (2013) Open abdominal management after damage-control laparotomy for trauma: a prospective observational American Association for the Surgery of Trauma multicenter study. J Trauma Acute Care Surg 74(1):113–120, discussion 1120–2
Salman AE, Yetisir F, Aksoy M et al (2014) Use of dynamic wound closure system in conjunction with vacuum-assisted closure therapy in delayed closure of open abdomen. Hernia 18(1):99–104
Björck M (2012) Vacuum and mesh-mediated fascial traction for primary closure of open abdomen in critically ill surgical patients. Br J Surg 99(12):1732–1733
Suliburk JW, Ware DN, Balogh Z et al (2003) Vacuum-assisted wound closure achieves early fascial closure of open abdomens after severe trauma. J Trauma 55(6):1155–1160, discussion 1160–1
Tsuei BJ, Skinner JC, Bernard AC, Kearney PA, Boulanger BR (2004) The open peritoneal cavity: etiology correlates with the likelihood of fascial closure. Am Surg 70(7):652–656
Bosscha K, Hulstaert PF, Visser MR, van Vroonhoven TJ, van der Werken C (2000) Open management of the abdomen and planned reoperations in severe bacterial peritonitis. Eur J Surg 166(1):44–49
Perez D, Wildi S, Demartines N et al (2007) Prospective evaluation of vacuum-assisted closure in abdominal compartment syndrome and severe abdominal sepsis. J Am Coll Surg 205(4):586–592
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Clavien PA, Barkun J, de Oliveira ML et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196
Clavien PA, Sanabria JR, Strasberg SM (1992) Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery 111(5):518–526
Petersson U, Acosta S, Björck M (2007) Vacuum-assisted wound closure and mesh-mediated fascial traction—a novel technique for late closure of the open abdomen. World J Surg 31(11):2133–2137
Malbrain ML, Cheatham ML, Kirkpatrick A et al (2006) Results from the international conference of experts on intra-abdominal hypertension and abdominal compartment syndrome. I. Definitions. Intensive Care Med 32(11):1722–1732
De Potter TJ, Dits H, Malbrain ML (2005) Intra- and interobserver variability during in vitro validation of two novel methods for intra-abdominal pressure monitoring. Intensive Care Med 31(5):747–751
Becker HP, Willms A, Schwab R (2007) Small bowel fistulas and the open abdomen. Scand J Surg 96(4):263–271
Burlew CC, Moore EE, Biffl WL et al (2012) One hundred percent fascial approximation can be achieved in the postinjury open abdomen with a sequential closure protocol. J Trauma Acute Care Surg 72(1):235–241
Seternes A, Myhre HO, Dahl T (2010) Early results after treatment of open abdomen after aortic surgery with mesh traction and vacuum-assisted wound closure. Eur J Vasc Endovasc Surg 40(1):60–64
Demetriades D, Salim A (2014) Management of the open abdomen. Surg Clin N Am 94(1):131–153
Jannasch O, Tautenhahn J, Lippert H, Meyer F (2011) Temporary abdominal closure and early and late pathophysiological consequences of treating an open abdomen. Zentralbl Chir 136(6):575–584
Tukiainen E, Leppäniemi A (2011) Reconstruction of extensive abdominal wall defects with microvascular tensor fasciae latae flap. Br J Surg 98(6):880–884
Koss W, Ho HC, Yu M et al (2009) Preventing loss of domain: a management strategy for closure of the “open abdomen” during the initial hospitalization. J Surg Educ 66(2):89–95
Nagy KK, Fildes JJ, Mahr C et al (1996) Experience with three prosthetic materials in temporary abdominal wall closure. Am Surg 62(5):331–335
Garner GB, Ware DN, Cocanour CS et al (2001) Vacuum-assisted wound closure provides early fascial reapproximation in trauma patients with open abdomens. Am J Surg 182(6):630–638
Ramirez OM, Ruas E, Dellon AL (1990) “Components separation” method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg 86(3):519–526
Ferguson EJ, Oswanski MF, Stombaugh HA, Daniels RG (2011) Early definitive closure of abdomen using components separation technique after damage control surgery. Am Surg 77(4):E74–E75
Roberts DJ, Zygun DA, Grendar J et al (2012) Negative-pressure wound therapy for critically ill adults with open abdominal wounds: a systematic review. J Trauma Acute Care Surg 73(3):629–639
Acknowledgments
The authors would like to thank Barbara Isenberg (German Office of Languages) for her help and linguistic advice.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Willms, A., Güsgen, C., Schaaf, S. et al. Management of the open abdomen using vacuum-assisted wound closure and mesh-mediated fascial traction. Langenbecks Arch Surg 400, 91–99 (2015). https://doi.org/10.1007/s00423-014-1240-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-014-1240-4