Abstract
Purpose
To compare the effectiveness of abdominal wall closure using the vacuum-assisted closure (NPC) as described by Barker et al. with an institutional protocol using a double polyvinyl bag in the first surgery, which is changed in subsequent surgeries to a polyvinyl bag placed over the bowel loops and a prolene mesh attached to the abdominal fascia (MMFC).
Methods
Randomized controlled trial. Patients with open abdomen (OA) due to a traumatic or a medical cause were included in the study. Variables studied included demographics, indication for surgery, number of interventions, hospital length of stay (HLOS), ICU length of stay, abdominal wound care costs, complication rates, and method and time to definitive fascial closure.
Results
From June 2011 to April 2013, 75 patients were enrolled in the study. Patients who died within 48 h were excluded; therefore, 53 patients in total were assessed. NPC achieved fascial closure in 75 % of patients, and MMFC achieved closure in 71.9 % of patients. The closure rates in patients with OA secondary to medical causes (80 % by NPC vs. 71.4 % by MMFC) or traumatic causes (70 % by NPC vs. 73.7 % by MMFC) were similar in both treatment groups. There were no differences between the groups with respect to cause of OA, complications, length of hospital stay, or the length of stay in the intensive care unit.
Conclusion
MMFC is a method comparable to NPC for the temporary management of OA that results in similar closure and complication rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Open abdomen (OA) is a validated and accepted surgical strategy that is useful for the management of surgical and traumatic pathologies [1–3]. Multiple temporary abdominal closure (TAC) techniques are described in the literature for OA management: Bogota bag [4], absorbable meshes, and the negative pressure wound therapy system [5]. However, these systems are not without risks; Infections, gastrointestinal fistulae, intra-abdominal abscesses, and multiple organ failure are among the most common complications.
However, the evidence that defines NPC as the best technique to achieve primary fascial closure is based on comparative studies with historical cohorts [5–10] and only two randomized studies [11, 12]. There have been recent additions to the NPC technique as originally described by Barker et al. [5, 8], such as the addition of fascial retention [12, 13] sutures or a mesh anchored to the fascia underneath the NPC dressing [10, 14], all of them with high closure rates.
Patients in whom primary closure is achieved during their hospitalization have shorter stays in the intensive care unit (ICU), in the hospital and a better quality of life than patients who are discharged with a ventral hernia [15, 16]. Thus, it is important to achieve primary closure during hospitalization and to employ strategies that allow a higher closure rate of the abdominal wall.
At the San Vicente Foundation University Hospital, Medellín, Colombia, a protocol with a polyvinyl double bag that is subsequently replaced by a Polypropylene mesh over another polyvinyl bag has been used for several years (mesh-mediated fascial closure or MMFC); the latter bag prevents visceral adhesions to the abdominal wall and allows fascia traction with serial approximations of the mesh. The present study aims to compare this system with the NPC as described by Barker et al. [5, 8] to determine which of the two is related to a higher rate of fascial closure. Additionally, the incidence of complications associated with OA management in both groups is compared.
Materials and methods
This is a randomized clinical trial (ClinicalTrials.gov Identifier: NCT01864590). Patients were divided into two groups, one of traumatic OA and the other of OA of a medical cause, with an allocation sequence in groups of four generated by a computer program. Patients over 15 years who required OA management according to the attending surgeon were entered in the study. An operating room nurse then took a sealed envelope from the box that corresponded to the patient group (traumatic or medical) and read aloud the corresponding assignment (MMFC or NPC).
The patient was required to continue the assigned temporary OA management technique until wall closure was achieved or for at least 21 days after the initial intervention. If at any time the patient was considered fit for abdominal wall closure, the patient was scheduled for surgery. This decision was left up to the treating surgeon, who also had the option of performing a standard abdominal wall closure or a components separation technique.
The NPC system was used as described by Barker et al. [5, 8] and was changed every 3 days in the operating room as per protocol. MMFC uses two polyvinyl bags: one intra-abdominal and subfascial that prevents the formation of adhesions and the other attached to the skin with 2–0 polypropylene (Fig. 1). Once the patient’s abdomen is macroscopically clean after consecutive washings and the infection focus is controlled (if it ever existed), one subfascial polyvinyl bag is inserted and tucked under the abdominal wall, and a polypropylene mesh is then fixed to the fascia. Every day, the mesh was “pinched” (Figs. 2, 3) and if it was loose, it was tightened with a continuous suture, without opening the mesh or changing the polyvinyl bag, the procedure was performed on the patient’s bedside, the excess mesh was usually trimmed down, and we do not require to open the mesh to tighten it. When the patient was considered ready for an abdominal wall closure, both the polyvinyl bag and the mesh were removed.
Patients who died within 48 h were excluded. Patients with penetrating trauma wounds on admission were assessed using the penetrating abdominal trauma index (PATI), revised trauma score (RTS), and APACHE II score. If the patient suffered blunt trauma, only the RTS and APACHE II scores were used. In patients with OA secondary to medical causes, APACHE II scores were recorded.
The following patient data were recorded: intrahospital mortality, number of surgical interventions, OA-related complications, abdominal wall closure, procedures used in fascial closure, length of stay in the ICU, and length of stay in the hospital general wards. The study was approved by the ethics committee of San Vicente Foundation University Hospital (Medellin, Colombia).
One patient was finally treated by MMFC after having been initially assigned to NPC and is the only protocol violation we had.
Statistical analysis
Sample size According to the available literature, 30 % of patients who were managed for an OA with MMFC could be later treated with delayed primary fascial closure, and a system of negative pressure suction could increase the number of closures up to 60 %. With a power of 80 % and a confidence level of 95 %, 42 patients were required per group.
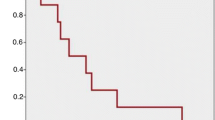
Kaplan–Meier survival analysis was used to calculate the cumulative probability of wall closure. The log-rank test was performed with the null hypothesis of no difference between the groups.
During the protocol’s development, we observed that primary closure could be achieved in a great number of patients with the MMFC. Therefore, an interim analysis was performed by a group external to the research project, and patient recruitment was suspended due to the results obtained.
Analyses were performed with SPSS version 21. The data were analyzed by “intention to treat” using nonparametric tests. Continuous variables were analyzed with the Mann–Whitney U test, and categorical variables were analyzed with Fisher’s test. Statistical significance was defined as p < 0.05.
Results
During the period of June 1st 2011 to April 30th 2013, 75 patients entered the study (Table 1) at the San Vicente Foundation University Hospital, a reference center in the city of Medellin (Colombia). Thirty-seven patients entered the NPC group, 18 with OA secondary to medical causes and 19 with OA secondary to trauma. Of the Thirty-eight patients included in the MMFC group, there were 18 and 20 cases of OA secondary to medical causes and trauma, respectively (Fig. 4). The mean age of the patients was 47 years (SD 19). In the first 48 h, the mortality rate was 45.9 % in patients with NPC and 13.2 % in patients with MMFC, and these patients were excluded from subsequent analyses (Fig. 4), leaving a total of 53 patients for further analysis.
The causes for OA in the trauma group were gun-shot wounds (GSW) with multivisceral intra-abdominal (IA) injuries in 11 patients, GSW with thoracoabdominal injuries in four, GSW with neck and thoracoabdominal injuries in two, and stab wounds (SW) with multiple IA lesions in two patients, SW with thoracoabdominal injuries in one, seven patients with Blunt traumatic injuries, and two patients with other mechanisms of trauma. In the group with Medical causes for OA Peritonitis was the cause in 16 patients, Aortic aneurysm repair in two, mesenteric ischemia in one, severe necrotizing pancreatitis in one and other causes in four patients.
Table 2 presents the APACHE, RTS, and PATI severity indices. Additional prognostic variables were measured upon admission to the ICU, including pH, excess base, and lactate levels.
Seven patients died after the initial 48 h, for a late mortality of 13.5 %. Two of these deaths were in the NPC group and five in the MMFC. The two deaths in the NPC were a patient with an abdominal GSW with a severe pancreatico-duodenal injury that developed a duodenal fistula, persistent sepsis, and died secondary to multiple organ failure (MOF), and the other patient had an abdominal GSW who developed an enterocutaneous fistula (ECF) and died due to sepsis. Out of the five deaths in the MMFC group, one was not related to the OA as it was a patient with multiple thoracoabdominal SW that later developed acute respiratory distress syndrome (ARDS); one was a patient with a gastric pull-up that developed gastric remnant necrosis and a small bowel fistula; two patients had GSW with multiple intra-abdominal injuries with ECF and died secondary to sepsis; and the last patient had a ruptured hepatic abscess and died secondary to sepsis from recurrent intra-abdominal collections. No difference was found when comparing the risk of death with NPC 0.867 (CI 0.71–1.05) and MMFC 0.19 (CI 95 % 0.26–1.41).
Fascial closure was possible in 15 patients treated with NPC (75 %) and in 24 (72.7 %) treated with MMFC; Table 3 presents the type of closure according to the cause of the OA. NPC patients underwent 4 surgical washings on average (median = 3; range 1–10), whereas MMFC patients underwent an average of three procedures (median = 2; range 0–8). It is important to clarify that these surgical procedures did not include the mesh “plication” that was done at the bedside for the patients in the MMC group.
The mean number of days with OA was 14 for the NPC group (median = 12) and 10 for MMFC (median = 6). The probability of not achieving fascial closure [NPC = 17 (CI 10.4–23.6), MMFC = 12 CI 9.9–18] was similar in both groups (p = 0.742) (Fig. 5).
With respect to the definitive management of OA, 39 patients had fascial closure, including 45.3 % by primary fascial closure and 28.3 % by the separation of components technique (Table 4) [17]. ICU and hospital length of stay, and mortality were similar among both groups (Table 5). Patients randomized to the MMFC had the mesh placed on the second surgical wash on average, median 2 (min 1–max 8).
Two patients in the NPC group and three in the MMFC developed fistulas, the rates (10.0 % in the NPC versus 9.4 % in the MMFC) did not reach significance (Table 6). We had four cases of evisceration of abdominal contents with the MMFC, all of them in the initial resuscitation phase with the double silo bags, all patients had to be taken back the OR to correct the problem and new double silo bags were placed. We analyzed complications of closure as a separate result and found no difference among both groups (Table 7).
Discussion
OA is a strategy that has proven useful in the management of critically ill patients. However, it has been associated with complications such as abscesses, fistulas, and impaired quality of life [3, 18–21]. Fascial closure during hospitalization has been associated with a shorter stay in the ICU, shorter overall hospital stay, and a decreased incidence of complications [9], as well as a better quality of life during the first year following discharge [15].
This study includes patients with OA secondary to traumatic and medical causes. This is a prospective study where the highest proportion of patients in the trauma subgroup had suffered penetrating injuries (84.2 % in NPC and 80 % in MMFC).
The study by Bee et al. [11] proposed the ninth day as the deadline for abdominal wall closure. Given that some authors report that up to 48 % of their cohorts had achieved closure between the ninth and twenty-first day, this study conducted follow-up through at least day 21 [22].
The closure rate achieved in this group with NPC is comparable to what has been reported in the literature, 68–100 % [6, 7, 10, 13, 22–25]. The highest rates of abdominal wall closure reported have been achieved using NPC and the Wittman patch according to some studies [18, 26]. However, there are several reports of NPC with closure rates that are comparable or even lower [11, 19, 20, 27]. Nonetheless, there are no previous reports of the similarities in the closure rates achieved with NPC and MMFC.
Patients with OA of medical cause treated with NPC tend to have lower closure rates than those with trauma-related OA [19, 26, 28]. In the patients in our study with OA of medical cause, we observed a high percentage of fascial closure with both temporary techniques for OA management, and this closure rate was similar to that of patients with OA of traumatic cause. There was no difference in time to closure if the abdomen was left open due to trauma or due to a medical cause. We did find a statistical trend toward earlier closure in the MMFC group (mean day 10 vs. 14 in NPC, p = 0.191), possibly in a trial with more patients this could have reached statistical significance.
Acosta et al. [10] and Rasilainen et al. [14] have performed studies in which they combined mesh-mediated closure with negative pressure technique and obtained a fascial closure rate of 76 and 78 %. These closure rates are extremely good; we think it would be interesting to compare the MMFC and their technique, to determine if the fascial closure rate is increased with the addition of the negative pressure dressing.
One of the difficulties that we encountered with the MMFC is that during the initial resuscitation of critically ill patients, if there is a considerable increase in the intra-abdominal pressure, the patients might eviscerate and require an urgent take-back to surgery. To prevent this from happening during the initial procedure, we recommend using a loose double silo bag that once the patient has been adequately resuscitated can be changed to the MMFC and traction to the fascia can be applied.
The incidence of deep surgical site infection (SSI) ranges from 4 to 19.7 % [6, 9, 11, 22, 28]. One of the theoretical advantages of NPC is the management of secretions, which could help reduce intra-abdominal collections. However, no difference in intra-abdominal collections has been observed in the previous randomized study [11] or in our study.
Some authors cautioned the use of the NPC because it can increase the rate or severity of gastrointestinal fistulas. A higher risk of gastrointestinal fistulas is observed in patients with OA due to peritonitis [21, 29]. In our study, there were no differences in the complications between groups despite long-term follow-up. The systematic review of the extensive literature on OA demonstrates a fistula rate of 15.6 % in patients with NPC and peritonitis compared with 7.3 % in patients with NPC due to trauma [26]. According to Carlson [27], a study of 2000 patients would be required to detect a difference of 3 % in the fistula rate, which does not appear to be feasible.
No difference was observed between the groups with respect to complications associated with abdominal wall closure. Most studies do not report these sets of complications. Kafka-Ritsch [13] reported superficial, deep, and organ/space SSI in 19, 4, and 10.75 % of the patients in their study, which is similar to what we have observed.
Pliakos et al. [12] reported a decrease of 5.6 days in the length of hospital stay with the use of VAC® (VAC, KCI) with retention sutures. Battacchi et al. reported shorter hospital stays (6.4 days less) and shorter ICU stays (5.9 days less) in patients treated with NPC compared with those treated with the Bogota bag [30]. We observed no difference in the length of hospital stay, the length of ICU stay, or in the duration of OA between the groups. It is worth noting that one case of abdominal wall closure was achieved on day 44 in one patient with MMFC.
The management of the OA can be a challenging task, especially if expensive commercially available assisted closure devices are not readily available [28, 30]. We did not use any commercially available NPC system but instead we used the technique originally described by Barker [8]. Some authors have suggested a higher closure rate of the OA with the commercially available system, possibly related to a better distribution of the negative pressure, and there is even data that argue its use will have long-term economic gain due to the prevention of a subsequent ventral hernias [25].
On the other hand, the MMFC approach permits the management of an OA in a cost-effective manner. It consists of simple materials that are readily available in an operating room. The MMFC approach represents another feasible and inexpensive surgical option in the management of the OA.
This study has several limitations, especially the observed higher early mortality in patients randomly assigned to NPC, which caused an imbalance in the patient groups. Randomization was performed during the surgery in which the abdomen was left open; we believe that it was wrong to exclude a priori patients at high risk of early death because it could introduce bias by excluding severely ill patients. There were no statistical differences in the different severity indexes between the two groups that could attribute this to a randomization failure, and upon a case-by-case review, we found no explanation for the mortality disparity.
The high mortality rate reported in our study is similar to the rate of up to 44 % that have been reported by other authors [9, 31]. There are several studies that demonstrate that NPC therapy does not increase mortality rates [27]; no association between NPC and early death was observed in this study.
Another limitation for this study is the fact that it is a single center study, and it would be better to test the novel technique in a multi-institutional setting. Also, including a larger number of patients could have lead to finding different outcomes between both TAC techniques.
The greatest strength of this study is that it suggests that the most relevant factor for fascial closure is not negative pressure suction but any system that would maintain constant tension on the fascia, preventing the loss of the abdominal wall domain.
Conclusion
To date, no single TAC technique has proven to be appropriate for all OAs and each strategy is associated with major shortcomings. Our study results suggests that the most relevant and cost-effective factor for abdominal wall fascial closure is probably not dependant solely on the use of negative pressure but instead on the application of any system that can provide constant tension to the opposing abdominal fascial edges and thus regain abdominal wall domain. The MMFC technique is easy to perform and can be accomplished with routine operating room supplies at a very reasonable cost.
References
William PS, Rao RI, Michael FR, Asher H (2006) Open abdomen after trauma and abdominal sepsis: a strategy for management. J Am Coll Surg 203(3):390–396
Kaplan MBP, Orgill DP, Ivatury RR, Demetriades D, Moore FA, Miller P, Nicholas J, Henry S (2005) Guidelines for the management of the open abdomen. Wounds 17(Suppl 1):1–24
Open Abdomen Advisory P, Campbell A, Chang M, Fabian T, Franz M, Kaplan M et al (2009) Management of the open abdomen: from initial operation to definitive closure. Am Surg 75(11 Suppl):S1–S22
Borraez O (2001) Abdomen Abierto, utilización del polivinilo. Rev Colombiana de Cirugia 16(1):39–43
Brock WB, Barker DE, Burns RP (1995) Temporary closure of open abdominal wounds: the vacuum pack. Am Surg 61(1):30–35
Barker DE, Green JM, Maxwell RA, Smith PW, Mejia VA, Dart BW et al (2007) Experience with vacuum-pack temporary abdominal wound closure in 258 trauma and general and vascular surgical patients. J Am Coll Surg 204(5):784–792
Roberts DJ, Zygun DA, Grendar J, Ball CG, Robertson HL, Ouellet JF et al (2012) Negative-pressure wound therapy for critically ill adults with open abdominal wounds: a systematic review. J Trauma Acute Care Surg 73(3):629–639
Barker DE, Kaufman HJ, Smith LA, Ciraulo DL, Richart CL, Burns RP (2000) Vacuum pack technique of temporary abdominal closure: a 7-year experience with 112 patients. J Trauma 48(2):201–206 (discussion 6–7)
Dubose JJ, Scalea TM, Holcomb JB, Shrestha B, Okoye O, Inaba K et al (2013) Open abdominal management after damage-control laparotomy for trauma: a prospective observational American Association for the Surgery of Trauma multicenter study. J Trauma Acute Care Surg 74(1):113–120 (discussion 1120–1122)
Acosta S, Bjarnason T, Petersson U, Palsson B, Wanhainen A, Svensson M et al (2011) Multicentre prospective study of fascial closure rate after open abdomen with vacuum and mesh-mediated fascial traction. Br J Surg 98:735–743
Bee TK, Croce MA, Magnotti LJ, Zarzaur BL, Maish GO III, Minard GM et al (2008) Temporary abdominal closure techniques: a prospective randomized trial comparing polyglactin 910 mesh and vacuum-assisted closure. J Trauma Inj Infect Crit Care 65(2):337–344
Pliakos I, Papavramidis TS, Mihalopoulos N, Koulouris H, Kesisoglou I, Sapalidis K et al (2010) Vacuum-assisted closure in severe abdominal sepsis with or without retention sutured sequential fascial closure: a clinical trial. Surgery 148(5):947–953
Kafka-Ritsch R, Zitt M, Schorn N, Stroemmer S, Schneeberger S, Pratschke J et al (2012) Open abdomen treatment with dynamic sutures and topical negative pressure resulting in a high primary fascia closure rate. World J Surg 36(8):1765–1771
Rasilainen SK, Mentula PJ, Leppaniemi AK (2012) Vacuum and mesh-mediated fascial traction for primary closure of the open abdomen in critically ill surgical patients. Br J Surg 99(12):1725–1732
Cheatham ML, Safcsak K (2008) Longterm impact of abdominal decompression: a prospective comparative analysis. J Am Coll Surg 207(4):573–579
Cheatham ML, Safcsak K, Llerena LE, Morrow CE Jr, Block EF (2004) Long-term physical, mental, and functional consequences of abdominal decompression. J Trauma 56(2):237–241 (discussion 41–42)
Ramirez OM (2006) Inception and evolution of the components separation technique: personal recollections. Clin Plast Surg 33(2):241–246, vi
van Hensbroek PB, Wind J, Dijkgraaf MG, Busch OR, Carel Goslings J (2009) Temporary closure of the open abdomen: a systematic review on delayed primary fascial closure in patients with an open abdomen. World J Surg 33(2):199–207
Diaz JJ Jr, Dutton WD, Ott MM, Cullinane DC, Alouidor R, Armen SB et al (2011) Eastern Association for the Surgery of Trauma: a review of the management of the open abdomen—part 2 “management of the open abdomen”. J Trauma 71(2):502–512
Diaz JJJ, Cullinane DC, Dutton WD, Jerome R, Bagdonas R, Bilaniuk JO et al (2010) The management of the open abdomen in trauma and emergency general surgery: part 1-damage control. J Trauma Inj Infect Crit Care 68(6):1425–1438
Rao M, Burke D, Finan PJ, Sagar PM (2007) The use of vacuum-assisted closure of abdominal wounds: a word of caution. Colorectal Dis 9(3):266–268
Miller PR, Meredith JW, Johnson JC, Chang MC (2004) Prospective evaluation of vacuum-assisted fascial closure after open abdomen: planned ventral hernia rate is substantially reduced. Ann Surg 239(5):608–614 (discussion 14–16)
Perez D, Wildi S, Demartines N, Bramkamp M, Koehler C, Clavien PA (2007) Prospective evaluation of vacuum-assisted closure in abdominal compartment syndrome and severe abdominal sepsis. J Am Coll Surg 205(4):586–592
Patel NY, Cogbill TH, Kallies KJ, Mathiason MA (2011) Temporary abdominal closure: long-term outcomes. J Trauma 70(4):769–774
Cothren CC, Moore EE, Johnson JL, Moore JB, Burch JM (2006) One hundred percent fascial approximation with sequential abdominal closure of the open abdomen. Am J Surg 192(2):238–242
Quyn AJ, Johnston C, Hall D, Chambers A, Arapova N, Ogston S et al (2012) The open abdomen and temporary abdominal closure systems–historical evolution and systematic review. Colorectal Dis 14(8):e429–e438
Carlson GL, Patrick H, Amin AI, McPherson G, Maclennan G, Afolabi E et al (2013) Management of the open abdomen: a national study of clinical outcome and safety of negative pressure wound therapy. Ann Surg 257:1154–1159
Wondberg D, Larusson HJ, Metzger U, Platz A, Zingg U (2008) Treatment of the open abdomen with the commercially available vacuum-assisted closure system in patients with abdominal sepsis: low primary closure rate. World J Surg 32(12):2724–2729
Fischer JE (2008) A cautionary note: the use of vacuum-assisted closure systems in the treatment of gastrointestinal cutaneous fistula may be associated with higher mortality from subsequent fistula development. Am J Surg 196(1):1–2
Batacchi S, Matano S, Nella A, Zagli G, Bonizzoli M, Pasquini A et al (2009) Vacuum-assisted closure device enhances recovery of critically ill patients following emergency surgical procedures. Crit Care 13(6):R194
Miller PR, Thompson JT, Faler BJ, Meredith JW, Chang MC (2002) Late fascial closure in lieu of ventral hernia: the next step in open abdomen management. J Trauma Inj Infect Crit Care 53(5):843–849
Acknowledgments
JC, CM, DM, ND, and MM declare no conflict of interest related to the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
Nothing to declare.
Additional information
ClinicalTrials.gov Identifier: NCT01864590.
Rights and permissions
About this article
Cite this article
Correa, J.C., Mejía, D.A., Duque, N. et al. Managing the open abdomen: negative pressure closure versus mesh-mediated fascial traction closure: a randomized trial. Hernia 20, 221–229 (2016). https://doi.org/10.1007/s10029-016-1459-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-016-1459-9