Abstract
Background
Abdominal Vacuum-Assisted Closure (V.A.C.) systems for treatment of open abdomens have been predominantly used for trauma patients with a high primary fascial closure rate. Use of the V.A.C. technique in abdominal sepsis is less well established.
Methods
All patients with abdominal sepsis and treatment with the abdominal V.A.C. system between 2004 and 2007 were prospectively assessed. End points were fascial closure, V.A.C.-related morbidity, and quality of life score (SF-36) at follow-up.
Results
Thirty patients with abdominal sepsis were included in the study. Primary fascial closure was feasible in 10, partial closure in 4, and no closure in 16 patients. Median number of V.A.C. changes was 3 (range, 1–10). Nine patients died. V.A.C.-related morbidity was as follows: two fistulas, three fascial edge necroses, one skin blister, and four prolapses of small bowel between the fascia and foam. Univariate analysis showed no variables influencing primary closure rate or V.A.C.-related morbidity. Mortality was significantly influenced by age (P < 0.001), respiratory failure (P = 0.01), and pneumonia (P = 0.03). At follow-up, V.A.C. patients scored lower in the physical health scores and similar in the mental health scores compared with the normal population.
Conclusions
Treatment of the open abdomen in patients with abdominal sepsis with the abdominal V.A.C. system is safe with good long-term quality of life. Primary closure rate in these patients is substantially lower than in trauma patients. Stepwise closure of the fascia during V.A.C. changes should be attempted to avoid additional lateral retraction of fascial edges. V.A.C.-related complications may be avoided with careful surgical technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In patients with abdominal sepsis delayed abdominal closure is sometimes necessary, creating an open abdomen or laparostomy. Massive contamination with the necessity of repeated abdominal lavage or edema of the bowel due to high volume fluid therapy in septic patients are common reasons for delayed abdominal closure [1]. The major principles in the management of an open abdomen are: easy access to the peritoneal cavity, prevention of desiccation of bowel, minimal further damage to the abdominal wall and low method-specific morbidity [2–4]. Many different techniques have been described previously, such as the Bogotá bag, towel packing with or without suction, mesh, synthetic patches, or a combination of different techniques [5–8]. Vacuum-assisted closure (V.A.C.) systems have been predominantly used for treatment of the open abdomen in trauma patients, especially in abdominal compartment syndrome [4, 9–13]. Simple and easy application, low system-related morbidity, and a high rate of primary fascial closure are the described main advantages.
The use of V.A.C. in abdominal sepsis not related to trauma has been less well established. Because trauma patients tend to be younger with less comorbidities, the promising results seen in an injured patient might not be reproducible in patients with abdominal sepsis caused by a hollow viscus perforation or pancreatitis [1]. Different studies have evaluated the use of different types of V.A.C. systems in patients with nontraumatic open abdomens with promising results [2, 3, 14–16]. In these studies, primary fascial closure rates were between 70 and 100 percent, but the frequency of enterocutaneous fistula development ranged from 4 to 20 percent. To our knowledge, only two studies had the strict inclusion criteria of abdominal sepsis; all others included also abdominal compartment syndrome, which could have biased the results [3, 17].
This study was designed to evaluate the objective and subjective outcome of the commercially available V.A.C.® Abdominal Dressing System (KCI International, San Antonio, TX) in patients with abdominal sepsis. The V.A.C. Abdominal Dressing System is specifically designed for the temporary closure of the open abdomen. It consists of polyurethane foam encapsulated in a perforated, nonadherent polyethylene sheet and a second, separate foam with adhesive sheets and a suction device.
Patients and methods
Data of all patients with abdominal sepsis and V.A.C.® Abdominal Dressing System treatment between 2004 and 2007 were prospectively entered into a database. The criteria to establish the diagnosis of abdominal sepsis were secondary peritonitis as defined in the 2005 International Sepsis Forum Consensus Conference with systemic inflammatory reaction [18–20]. Indication for V.A.C. System use was massive intra-abdominal contamination with planned revisional laparotomy and/or inability of primary closure due to intestinal edema. If feasible, primary fascial closure was performed and these patients were not included in the study. No other techniques of abdominal closure were used during that time period. All surviving patients were planned for a follow-up examination with quality of life assessment. The study was approved by the local ethics committee.
Primary outcome was the rate of total or partial primary fascial closure and the detection of factors predicting nonclosure. The following variables were analysed: age, sex, American Society of Anaesthesiology (ASA) score, body mass index (BMI), origin of abdominal sepsis (colorectal, small bowel, stomach, unknown), maximal Mannheim Peritonitis Index (MPI) [21, 22], number of V.A.C. changes, time after initial operation when abdominal sepsis was under control, and medical morbidity (pneumonia, respiratory insufficiency, renal insufficiency, cardiac insufficiency). Secondary endpoints were V.A.C.-specific morbidity and factors influencing its frequency. Overall morbidity and mortality also was noted. Quality of life was assessed with a SF-36 questionnaire. The reference population were 375 German medical students [23].
Surgical technique
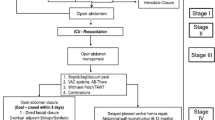
After completing the intra-abdominal part of the operation, the polyethylene sheet with the encapsulated foam was shaped into appropriate size. The sheet was designed to cover the intestine and reach out as far laterally as possible to envelop the bowel completely. The second polyurethane foam was cut moderately smaller than the fascial dehiscence (1–2 cm less in diameter) to ensure adequate traction on the fascial and wound edges. The foam, including the surrounding skin, was then covered with the adhesive tapes to ensure complete sealing. A 2-cm hole was cut in the middle of the foam to position the TRAC-PAD® (KCI International) suction device. After connection to the canister of the vacuum pump, a continuous negative pressure between 75 and 125 mmHg was established. The amount of negative pressure was determined by the responsible surgeon. As a standard, an interval of 48 hours was determined for revisional surgery with change of the abdominal V.A.C. If granulation tissue reaction was very slow and abdominal sepsis under control, abdominal V.A.C. change intervals up to 72 hours were possible. The treating surgeon made the decision. Staged closure of the fascia was performed when feasible, resulting in a smaller abdominal V.A.C.
When primary closure was deemed not feasible because of fascial retraction and prolapsing bowel with no further intra-abdominal revision necessary, an absorbable mesh (Vicryl®, Ethicon Inc.) was implanted directly on the greater omentum or the bowel (inlay technique). The mesh was covered with conventional V.A.C. foam with 50 to 75 mmHg negative pressure. As soon as granulation tissue was present on the mesh, split skin grafting was performed.
Statistical analysis
Results are expressed as mean ± standard deviation (SD) or median with range. The influence of the following variables on primary closure, V.A.C.-specific morbidity, and mortality was conducted: age, sex, ASA score, BMI, origin of abdominal sepsis (colorectal, small bowel, stomach, unknown), MPI index, number of V.A.C. changes, time after initial operation when abdominal sepsis was under control, and medical morbidity. Univariate regression using Fisher’s exact test and χ2 test for dichotomous data and Mann-Whitney U test for continuous data was performed. Results are shown as odds ratio (OR) with 95% confidence interval (CI). Statistical analysis was performed by using SPSS®, Version 13 (SPSS Inc., Chicago, IL). Regardless of the statistical tests selected, the level of significance was defined as P ≤ 0.05.
Results
Between April 2004 and September 2007, 30 patients with an open abdomen caused by abdominal sepsis were treated with the V.A.C. Abdominal Dressing System. The descriptive characteristics of the patients are shown in Table 1. Nine patients died in the hospital, resulting in a mortality of 30%. Origin of sepsis in these patients was as follows: seven colorectal, one stomach, and one small bowel. In 16 patients (53%), no closure of the facial defect was possible, in 4 patients (13%) the fascia was closed partially, and in 10 (30%) patients a full closure was feasible. In the 16 patients without fascial closure, 11 had inlay absorbable mesh placement and subsequent skin grafting. Five patients died before closure of the fascia was possible. Median duration of antibiotic therapy was 23 (range, 8–63) days.
The median number of V.A.C. Abdominal Dressing System changes in all patients was 3 (range, 1–10). In patients with primary closure, the median interval between the first revisional surgery and the complete closure of the abdomen was 32 (range, 5–81) days. These patients needed a median of 4 (range, 1–6) V.A.C. changes. In patients for whom no definite closure was possible, the median interval between revisional surgery and inlay mesh implantation was 20 (range, 7–52) days, or 3 (range, 1–5) V.A.C. changes. V.A.C.-specific morbidity is shown in Table 2.
No variables had a significant influence on V.A.C.-specific morbidity or primary closure rate in the univariate analysis. Three variables showed a significant influence on mortality: age (P < 0.001), respiratory failure (P = 0.01), and pneumonia (P = 0.03).
Sixteen patients (53%) had clinical follow-up (median follow-up interval, 20.1 (range, 5–40) months). Of the remaining 14 patients, 8 died in the hospital, 1 died during the follow-up period, 2 refused to attend the follow-up assessment, and 3 were not assessed because their initial hospitalization was less than 3 months before follow-up. Of the assessed patients, 6 had complete primary closure, 4 had partial closure, and 6 underwent no facial closure. Of the 6 patients with primary closure, 1 developed an incisional hernia. All patients with inlay absorbable mesh and split skin graft developed incisional hernias. In 7 patients, incisional hernia repair was performed at time of follow-up, whereas the remaining 3 were planned for surgery in the near future. The results of the SF–36 questionnaire are outlined in Fig. 1. Overall, V.A.C. patients scored in the four physical health scores, whereas the values in mental health scores were similar compared with the normal population.
Results of the SF-36 questionnaire with comparison to a standardized population [23]
Discussion
This study was designed to evaluate the primary fascial closure rate in patients with abdominal sepsis treated with the V.A.C. Abdominal Dressing System. The overall primary fascial closure rate was 30%, which is substantially lower than previously described rates of as much as 100% [2, 6, 9, 12, 24, 25]. However, all of these studies included patients with different aetiologies, such as peritonitis, pancreatitis, trauma, and abdominal compartment syndrome. To our knowledge, only two studies assessed exclusively patients with abdominal sepsis, unfortunately without any data on primary fascial closure rates [3, 17]. The underlying etiology of the abdominal sepsis correlates with the primary fascial closure rate with trauma patients more likely to have the fascia closed [1, 26]. There might be different reasons for the discrepancy in the fascial closure results between trauma patients and peritonitis patients. One might be substantially higher age in abdominal sepsis, which was median 63 years in this collective, compared with trauma series with a median age generally younger than 40 years [7, 10, 12]. The lower age corresponds to less comorbidity, resulting in a higher potential for a rapid resolution of bowel edema.
Another important reason is the differences in time until primary closure is feasible. The main indication for abdominal V.A.C. system in trauma patients is abdominal compartment syndrome or a damage control situation with early relaparotomy and definitive repair. In contrast, patients with severe contamination associated with abdominal sepsis are likely to require repeated lavages [1, 4, 16, 17]. Ongoing intra-abdominal infection with repeated abdominal washouts prolongs the recovery and delays definite fascial closure. This results in lateral retraction of the fascial edges despite the negative pressure of the V.A.C. system. Primary closure is difficult if treatment with the open abdomen exceeds 2 weeks [27]. We found it difficult to avoid the retraction, even if the margins of the V.A.C. foam were perfectly matched to the fascial margins. To prevent the retraction, an early closure of the fascia should be attempted, beginning at the cranial and caudal ends of the incision, even if ongoing contamination is present intra-abdominally.
In patients for whom primary closure after V.A.C. treatment was not feasible, an inlay resorbable mesh was used to cover the fascial defect. After growth of granulation tissue, split skin grafting was performed. A major disadvantage of this technique is the development of a ventral hernia. However, in these severely sick patients we consider it inappropriate to attempt any primary closure of the fascial defect with flap or release techniques.
No variables showed any influence on primary fascial closure rate or V.A.C.-related morbidity. Navsaria et al. [7] showed a higher rate of primary closure rate in patients with non-frozen abdomen. Our experience supports this finding. Patients with delayed closure developed tense adhesions between small-bowel loops combined with retraction of the fascial edges.
V.A.C.-specific morbidity was rather low. Two patients (7%) developed fistulas, which is comparable to the rate in the literature of 0–20% [7, 10, 11, 14]. The rate of fistulation might be higher in patients with abdominal sepsis compared with trauma patients. Rao et al [14] described an enterocutaneous fistula rate of 20% in a group of patients with predominantly abdominal sepsis and concluded that V.A.C. dressings should be used with caution in patients with abdominal sepsis. Other authors supported this conclusion [28]. However, the fistulas might not have been caused by the V.A.C. system or the negative pressure itself but rather by manipulation of the surgeon during dressing changes. V.A.C. system changes in patients with abdominal sepsis and associated fragile bowel should be performed by an experienced surgeon.
Other V.A.C.-related complications were necrosis at the fascial edges, blister under the adhesive tape, and prolapsing small bowel between the V.A.C. edge and the fascial/skin edge. Necrosis needing debridement might not be related to the V.A.C. itself but rather caused by ischemia or ongoing infection of the fascial edges. Blisters occurred in one patient and might be related to tension between the skin and the adhesive tape. Prolapsing small bowel might be caused by technical error or increasing abdominal pressure. This condition made it mandatory to perform the V.A.C. change earlier than planned. Although the V.A.C. foam should be cut a little smaller than the wound size to ensure adequate traction of the fascial edges, having foam that is too small might allow the bowel to prolapse between the foam and the fascial edges. Prolapse also can be caused by a too small polyethylene sheet, which happens especially in a frozen abdomen where tense adhesions between bowel loops and the abdominal wall make it difficult to cover the entire bowel. In our view, the majority of the mentioned V.A.C.-related complications may be avoided by correct surgical technique.
At the time of follow-up, the majority of patients were surprisingly satisfied with the result. Although physical health was still impaired, mental health scores were similar compared with the reference population. These findings correlate with Perez et al. [15], which to our knowledge is the only other study to assess quality of life after treatment of left open abdomen with the abdominal V.A.C. system. One possible explanation for the high SF-36 scores may be the fact that these patients were grateful to survive their severe illness. Because overall numbers at time of follow-up were small, we did not compare quality of life scores between patients with primary closure and patients with mesh/skin graft closure. All patients with mesh/skin graft closure had incisional hernias, forcing them to undergo elective hernia repair. Only one of six patients with primary closure developed an incisional hernia. Primary closure at the time of initial treatment should be the major goal in these patients.
All seven patients with incisional hernia underwent repair using a VIPRO™ (Ethicon, Switzerland) mesh in sublay position. We chose an interval between the primary hospitalization and the hernia repair of 6 months or more to ensure that all inflammatory changes had settled and the patient had recovered fully. Hernia repair was feasible in all patients. Dissection of the skin graft from the bowel or intra-abdominal adhesions did not cause any technical problems.
Some limitations need to be mentioned. The primary aim was the evaluation of the commercially available V.A.C. Abdominal Dressing. When primary fascial closure was not possible, the V.A.C. system was used. This is not a comparative study with other closure techniques in the setting of abdominal sepsis. Therefore, no conclusions concerning the superiority of the system in comparison to other techniques can be made. To answer the question about which of the different techniques is optimal in patients with abdominal sepsis, a prospective randomized trial is warranted.
Conclusions
Treatment of the open abdomen in patients with abdominal sepsis with the abdominal V.A.C. system is safe with good long-term quality of life results. Primary closure rate in these patients is substantially lower than reported in trauma patients. Stepwise closure of the fascia during V.A.C. changes should be attempted to avoid additional lateral retraction of fascial edges. V.A.C.-related complications may be avoided with careful surgical technique.
References
Tsuei BJ, Skinner JC, Bernard AC et al (2004) The open peritoneal cavity: etiology correlates with the likelihood of fascial closure. Am Surg 70:652–656
Oetting P, Rau B, Schlag PM (2006) Abdominal vacuum device with open abdomen. Chirurg 77:586–593
Adkins AL, Robbins J, Villalba M et al (2004) Open management of intra-abdominal sepsis. Am Surg 70:137–140
Miller PR, Thompson JT, Faler BJ et al (2002) Late fascial closure in lieu of ventral hernia: the next step in open abdomen management. J Trauma 53:843–849
Fernandez L, Norwood S, Roettger R et al (1996) Temporary intravenous bag silo closure in severe abdominal trauma. J Trauma 40:258–260
Cothren CC, Moore EE, Johnson JL et al (2006) One hundred percent fascial approximation with sequential abdominal closure of the open abdomen. Am J Surg 192:238–242
Navsaria PH, Bunting M, Omoshoro-Jones J et al (2003) Temporary closure of abdominal wounds by the modified sandwich-vacuum pack technique. Br J Surg 90:718–722
Nagy KK, Fildes JJ, Mahr C et al (1996) Experience with three prosthetic materials in temporary abdominal wall closure. Am Surg 62:331–335
Stone PA, Hass SM, Flaherty SK et al (2004) Vacuum-assisted fascial closure for patients with abdominal trauma. J Trauma 57:1082–1086
Barker DE, Kaufman HJ, Smith LA et al (2000) Vacuum pack technique of temporary abdominal closure: a 7-year experience with 112 patients. J Trauma 48:201–207
Labler L, Zwingmann J, Mayer D et al (2005) V.A.C. abdominal dressing system. Eur J Trauma 5:488–494
Miller PR, Meredith JW, Johnson JC et al (2004) Prospective evaluation of vacuum-assisted fascial closure after open abdomen. Ann Surg 239:608–616
Cipolla J, Stawicki SP, Hoff WS et al (2005) A proposed algorithm for managing the open abdomen. Am Surg 71:202–207
Rao M, Burke D, Finan PJ et al (2007) The use of vacuum-assisted closure of abdominal wounds: a word of caution. Colorectal Dis 9:266–268
Perez D, Wildi S, Demartines N et al (2007) Prospective evaluation of vacuum-assisted closure in abdominal compartment syndrome and severe abdominal sepsis. J Am Coll Surg 205:586–592
Smith LA, Barker DE, Chase CW et al (1997) Vacuum pack technique of temporary abdominal closure: a four-year experience. Am Surg 63:1102–1108
Olejnik J, Sedlak I, Brychta I et al (2007) Vacuum supported laparostomy: an effective treatment of intra-abdominal infection. Bratisl Lek Listy 108:320–323
Calandra T, Cohne J (2005) The international sepsis forum consensus conference on definitions of infection in the intensive care unit. Crit Care Med 33:1538–1548
Ivancevic N, Radenkovic D, Bumbasirevic V et al (2008) Procalcitonin in preoperative diagnosis of abdominal sepsis. Langenbecks Arch Surg 393:3397–3403 Epub 2007 Oct 30
Maier S, Traeger T, Westerholt A et al (2005) Special aspects of abdominal sepsis. Chirurg 76:829–836
Wacha H, Linder MM, Feldmann U et al (1987) Mannheim peritonitis index–prediction of risk of death from peritonitis: construction of a statistical and validation of an empirically based index. Theo Surg 1:169–177
Linder MM, Wacha H, Feldmann U et al (1987) The Mannheim peritonitis index. An instrument for the intraoperative prognosis of peritonitis. Chirurg 58:84–92
Bullinger M (1995) German translation and psychometric testing of the SF-36 health survey: preliminary results from the IQOLA project. Soc Sci Med 41:1359–1366
Barker DE, Green JM, Maxwell RA et al (2007) Experience with vacuum-pack temporary abdominal wound closure in 258 trauma patients and general and vascular surgical patients. J A. Coll Surg 204:784–793
Suliburk JW, Ware DN, Balogh Z et al (2003) Vacuum-assisted wound closure achieves early fascial closure of open abdomens after severe trauma. J Trauma 55:1155–1160
Petersson U, Acosta S, Bjoerck M (2007) Vacuum-assisted wound closure and mesh-mediated fascial traction – a novel technique for late closure of the open abdomen. World J Surg 31:2133–2137
Stonerock CE, Bynoe RP, Yost MJ et al (2003) Use of a vacuum-assisted device to facilitate abdominal closure. Am Surg 69:1030–1034
Starr-Marshall K (2007) Vacuum-assisted closure of abdominal wounds and entero-cutaneous fistulae: the St Marks experience. Colorectal Dis 9:573
Acknowledgements
The authors thank Dr. C. Baughman and Dr. J. Chisholm for help in preparation of the manuscript in English.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wondberg, D., Larusson, H.J., Metzger, U. et al. Treatment of the Open Abdomen with the Commercially Available Vacuum-Assisted Closure System in Patients with Abdominal Sepsis. World J Surg 32, 2724–2729 (2008). https://doi.org/10.1007/s00268-008-9762-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-008-9762-y