Abstract
Purpose
The present study was designed to evaluate the relationship between the preoperative C-reactive protein levels and the incidence of postoperative infectious complications in patients undergoing colorectal surgery.
Methods
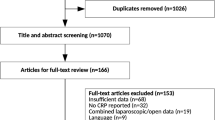
This study was a retrospective cohort study of a consecutive series of 464 patients who underwent elective colorectal resection between April 2010 and March 2012. We evaluated the patients’ preoperative conditions, including the preoperative C-reactive protein levels, surgical content, and incidence of postoperative infectious complications.
Results
Postoperative infectious complications occurred in 133 patients (28.7 %). In the univariate analysis, male gender, rectal surgery, open surgery, elevated preoperative white blood cell counts, elevated preoperative C-reactive protein levels, extended operative times, large amounts of blood loss during surgery, and ostomy formation were found to be significantly associated with the incidence of postoperative infectious complications. In the multivariate analysis, elevated preoperative C-reactive protein levels (OR per mg/dl = 1.17, 95 % CI = 1.02–1.37, P = 0.02) and large amounts of blood loss during surgery (OR per 100 g = 1.13, 95 % CI = 1.06–1.23, P < 0.01) were found to be independently associated with the incidence of postoperative infectious complications.
Conclusions
This study provides evidence of an association between the preoperative C-reactive protein level and the incidence of postoperative infectious complications following colorectal surgery, which should be further confirmed in prospective and appropriately designed studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite advances in operative techniques and perioperative care, postoperative infectious complications are the most frequent complications that occur following colorectal surgery, which belongs to the category of clean–contaminated operations. For instance, anastomotic leakage occurs in 1–39 % [1] of cases and surgical site infection occurs in 3–30 % [2] of cases.
Postoperative infectious complications prolong hospital stays, increase medical costs, and occasionally lead to mortality [3, 4]. Moreover, it has been recently reported that postoperative infectious complications, typically caused by anastomotic leakage, in patients undergoing gastrointestinal surgery lead to poor cancer-specific survival rates [5–8]. Therefore, colorectal surgeons are concerned with preventing postoperative infectious complications such as surgical site infection and pneumonia following colorectal surgery.
It has been reported that preoperative conditions and surgical factors might be associated with the incidence of postoperative infectious complications in patients undergoing colorectal surgery [9]. Preoperative conditions include nutritional status, age, smoking, and coexisting morbidities, such as diabetes mellitus, heart disease, and liver cirrhosis. Surgical factors include the degree of contamination, operative time, volume of blood loss, use of blood transfusions, and the need for emergency surgery.
C-reactive protein is known to be an indicator of infectious or inflammatory conditions [10]. It has been reported that the postoperative C-reactive protein levels predict the incidence of postoperative infectious complications in patients undergoing colorectal surgery [11, 12]. However, to our knowledge, it is not known whether the preoperative C-reactive protein levels relate to the incidence of postoperative infectious complications. For this reason, we conducted this study to investigate the predictive value of the preoperative C-reactive protein levels for the incidence of postoperative infectious complications following colorectal surgery.
Materials and methods
This study was a retrospective cohort study of a consecutive series of 464 patients who underwent elective colorectal resection via laparotomy at the National Defense Medical College Hospital between April 2010 and March 2012. Patients with preoperative clinical evidence of infection or other inflammatory conditions, such as inflammatory bowel disease or diverticulitis, were excluded from this study. In addition, patients who had developed minor postoperative infections, such as phlebitis or cholecystitis, were also excluded. The mean age of the patients was 67 years, and there were 289 males and 175 females. The stage of colorectal cancer was assigned according to the Japanese Classification of Colorectal Carcinoma, seventh edition [13]. Only three patients received chemoradiation therapy, and only four patients received corticoid therapy. The characteristics of the patients in this study are presented in Table 1.
Five surgeons participated in the majority of cases as either operator or supervisor. All patients in this study underwent routine preoperative blood test, chest X-rays, and urinalysis after admission. Before surgery, most patients received bowel preparation with an oral laxative. After surgery, oral intake was basically started on the third postoperative day after colonic surgery or was started on the fifth postoperative day after rectal surgery. We typically used epidural catheters for analgesia. With regard to the regimen of surgical antimicrobial prophylaxis, the administration of cefmetazole (1 g) was started just before the skin incision was made, was repeated every 3 h during surgery, and was performed in the morning and evening on the first postoperative day.
Patients were retrospectively evaluated for preoperative factors, surgical factors, and postoperative status on the basis of their medical and nursing charts. The preoperative factors included age, gender, tumor site, diseases, body mass index, presence of diabetes mellitus or heart disease, smoking status, and preoperative laboratory data (the white blood cell count, the neutrophil count, the lymphocyte count, the albumin level, and the C-reactive protein level). The surgical factors included operative time, volume of blood loss, procedure, and ostomy formation.
The occurrence of postoperative infectious complications was defined according to a combination of clinical findings, and the results of laboratory and other tests recorded in the patients’ medical records. The postoperative infectious complications included incisional surgical site infection (SSI), organ/space SSI, enterocolitis, urinary tract infection, and pneumonia. Incisional and organ/space SSI were diagnosed according to the definitions stated in the guidelines issued by the Center for Disease Control and Prevention [14]. Incisional SSI, including superficial and deep incisional SSI, are infections at the incision site characterized by the presence of a purulent discharge or local signs of infection or wound opening. Organ/space SSI, including anastomotic leakage and intra-abdominal abscess formation, is characterized by the presence of purulent discharge from a drain placed into the organ/space or an abscess found on direct or radiological examination. Enterocolitis was diagnosed on the basis of clinical symptoms, such as diarrhea with pyrexia, and fecal culture. Urinary tract infections were diagnosed based on positive urine cultures with pyrexia. Pneumonia was diagnosed based on the clinical symptoms and the findings of radiological examinations. The grade of postoperative infectious complications was assigned according to the Clavien–Dindo Classification [15].
The statistical analysis was performed using JMP software (SAS Institute Inc., Cary, NC). The univariate relationships between the variables and the occurrence of postoperative infection were evaluated using a logistic model for continuous variables and Pearson’s χ 2 test for categorical variables. The variables with a P value <0.05 in the univariate analysis were entered into the multivariate logistic regression model using the forced entry method. P values <0.05 were considered to be statistically significant.
Results
Table 2 shows the frequency of postoperative infectious complications and the grade of complications in this study. In total, postoperative infectious complications occurred in 133 (28.7 %) of the 464 patients. Incisional SSI occurred in 62 (13.4 %) patients, and organ/space SSI occurred in 53 (11.4 %) patients. Type of morbidity occurred in 161 (34.7 %) patients, and three patients (0.6 %) died in this study. Two patients died after sigmoidectomy because of a myocardial infarction that developed from severe pneumonia and because of severe MRSA enterocolitis, respectively. One patient died after abdominoperineal resection and a second surgery for ostomy necrosis, after which, severe pseudomembranous colitis occurred. Ostomy formation was performed in 81 (42.6 %) of the 190 patients with rectal tumors and 10 (2.2 %) of the 266 patients with colonic tumors.
Table 3 shows the associations between preoperative factors and the incidence of postoperative infectious complications. According to a univariate analysis, male gender (P = 0.03), rectal surgery (P < 0.01), elevated preoperative white blood cell counts (P = 0.02), and elevated preoperative C-reactive protein levels (P = 0.01) were each found to be associated with an increased risk of developing postoperative infectious complications. Table 4 shows the associations between surgical factors and the incidence of postoperative infectious complications. In the univariate analysis, extended operative times (P < 0.01), large amounts of blood loss (P < 0.01), open surgery (P < 0.01), and ostomy formation (P < 0.01) were each found to be associated with an increased risk of developing postoperative infectious complications.
The variables with a P value <0.05 in the univariate analysis were entered into the multivariate logistic regression model using the forced entry method. Thereafter, large amounts of blood loss during surgery (P < 0.01) and elevated preoperative C-reactive protein levels (P = 0.02) were both found to be independently associated with an increased risk of developing postoperative infectious complications (Table 5).
Finally, although we analyzed the data by constructing ROC curves regarding postoperative infectious complications for the different preoperative C-reactive protein levels, the AUC was 0.53 (data not shown). Therefore, we could not obtain a useful cutoff value for the preoperative C-reactive protein level to predict postoperative infectious complications.
Discussion
The present study revealed that the preoperative C-reactive protein levels and the volume of blood loss during surgery are both independent risk factors for the development of postoperative infectious complications following colorectal surgery.
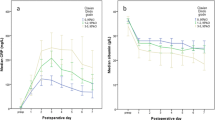
The C-reactive protein level is known as a widely available and routinely used marker for the diagnosis and follow-up of patients affected by various inflammatory diseases. There have been several attempts to use the postoperative C-reactive protein level to predict the occurrence of postoperative infectious complications after colorectal surgery. Recently, a meta-analysis which was performed for diagnostic studies including a total of 1,832 patients evaluating the C-reactive protein level as a predictor of postoperative infectious complications on days 1 to 5 after colorectal surgery revealed that the C-reactive protein level should be measured on POD 4 to best predict the risk of postoperative infectious complications [16].
In contrast, there have been few reports on the relationship between the preoperative C-reactive protein levels and the incidence of postoperative infectious complications. Fransen et al. previously reported that the patients with elevated preoperative C-reactive protein levels are at an increased risk for developing postoperative infections during cardiac surgery [17]. Moyes et al. recently reported that the preoperative Glasgow prognostic score, determined according to the combination of the C-reactive protein and albumin levels, predicts the occurrence of postoperative infection in patients with colorectal cancer [18]. However, the reason why the preoperative C-reactive protein levels are a risk factor for the development of postoperative infectious disease is not fully understood.
On the other hand, it has often been reported that preoperative elevation of C-reactive protein predicts poor survival in patients with colorectal cancer [19, 20]. Alexandrakis et al. reported that the C-reactive protein levels in cancer patients may result from tissue inflammation or immune responses to tumor growth [21]. Interestingly, there are also reports that, in patients with esophageal cancer, cancer itself produces C-reactive protein [22, 23]. However, the mechanisms underlying the elevation of C-reactive protein in cancer patients remain unclear.
C-reactive protein was first identified in 1930 and subsequently presumed to be an early indicator of infectious or inflammatory conditions [10]. Although the function of C-reactive protein is not fully understood, there are several reports that elevation of C-reactive protein reflects mediated immunity. Nozoe et al. and Leitch et al. reported that elevation of C-reactive protein is associated with lymphopenia [24, 25]. Canna et al. reported that elevation of C-reactive protein impairs the T lymphocytic response; in other words, the serum C-reactive protein level is inversely correlated with the level of tumor CD4+ T lymphocytes in patients with colorectal cancer [26]. Additionally, Mold et al. reported that in vitro, in the presence of lipopolysaccharide, C-reactive protein enhances IL-10 synthesis and inhibits IL-12 synthesis by interacting with FcγR [27]. Accordingly, we hypothesize the existence of a relationship between postoperative infectious complications and compromised immunity in patients with elevated C-reactive protein levels. More studies are needed to analyze the relationship between the C-reactive protein levels and the postoperative infectious complications.
Nevertheless, there have been several reports indicating that perioperative blood loss is an independent risk factor for the development of postoperative infectious complications [28–30]. As a plausible explanation, it is believed that hypovolemia and reductions in tissue oxygenation caused by the loss of red blood cells are detrimental to healing and increase the risk of infection and tissue dehiscence [31, 32].
In our study, we recognize several limitations. First, we cannot deny the existence of occult infection in patients with elevated preoperative C-reactive protein levels. However, in this study, no patients became feverish or exhibited signs of infection or other clinical symptoms on diagnosis. Second, this study was a retrospective study not a prospective study. There were no standardized procedures of surgical techniques or perioperative care. Third, there are other reported risk factors for the development of postoperative infectious complications, such as intraoperative hypotension, hypothermia, and the postoperative glucose levels, which we did not include in the database.
We recognize several weak points of our study. First, Moyes et al. reported that the preoperative C-reactive protein levels were not an independent risk factor in a similar multivariate analysis [18]. However, that study slightly differed from our study in terms of the analyzed patients. Specifically, that study included emergency operations. In addition, postoperative infectious complications in that study occurred in 15.3 % patients, which was lower than the rate in our study. Second, we could not obtain a useful cutoff value for the preoperative C-reactive protein level with regard to predicting the development of postoperative infectious complications.
Nonetheless, it is very interesting that preoperative elevation of the C-reactive protein level has been associated with both the incidence of postoperative infectious complications and poor survival in patients with colorectal cancer. Therefore, we are planning to analyze the relationship between the elevation of the C-reactive protein level and preoperative compromised immunity. We would consider less invasive surgery or providing more intensive perioperative care to patients with elevated preoperative C-reactive protein levels.
Conclusions
This study provides evidence of an association between the preoperative C-reactive protein levels and the incidence of postoperative infectious complications following colorectal surgery, which should be confirmed in prospective and appropriately designed studies. To prevent postoperative infectious complications or the worsening of infections, colorectal surgeons should carefully observe patients who show elevated preoperative C-reactive protein levels.
References
Bruce J, Krukowski ZH, Al-Khairy G, Russell EM, Park KG (2001) Systematic review of the definition and measurement of anastomotic leak after gastrointestinal surgery. Br J Surg 88:1157–1168
Smith RL, Bohl JK, McElearney ST, Friel CM, Barclay MM, Sawyer RG et al (2004) Wound infection after elective colorectal resection. Ann Surg 239:599–605
Collins TC, Daley J, Henderson WH, Khuri SF (1999) Risk factors for prolonged length of stay after major elective surgery. Ann Surg 230:251–259
Buchs NC, Gervaz P, Secic M, Bucher P, Mugnier-Konrad B, Morel P (2008) Incidence, consequences, and risk factors for anastomotic dehiscence after colorectal surgery: a prospective monocentric study. Int J Color Dis 23:265–270
McArdle CS, McMillan DC, Hole DJ (2005) Impact of anastomotic leakage on long-term survival of patients undergoing curative resection for colorectal cancer. Br J Surg 92:1150–1154
Nespoli A, Gianotti L, Bovo G, Brivio F, Nespoli L, Totis M (2006) Impact of postoperative infections on survival in colon cancer patients. Surg Infect (Larchmt) 7(Suppl 2):S41–S43
Law WL, Choi HK, Lee YM, Ho JW (2007) The impact of postoperative complications on long-term outcomes following curative resection for colorectal cancer. Ann Surg Oncol 14:2559–2566
Tsujimoto H, Ichikura T, Ono S, Sugasawa H, Hiraki S, Sakamoto N et al (2009) Impact of postoperative infection on long-term survival after potentially curative resection for gastric cancer. Ann Surg Oncol 16:311–318
Rovera F, Dionigi G, Boni L, Piscopo C, Masciocchi P, Alberio MG et al (2007) Infectious complications in colorectal surgery. Surg Oncol 16:S121–S124
Clyne B, Olshaker JS (1999) The C-reactive protein. J Emerg Med 17:1019–1025
Welsch T, Muller SA, Ulrich A, Kischlat A, Hinz U, Kienle P et al (2007) C-reactive protein as early predictor for infectious postoperative complications in rectal surgery. Int J Color Dis 22:1499–1507
Matthiessen P, Henriksson M, Hallbook O, Grunditz E, Noren B, Arbman G (2008) Increase of serum C-reactive protein is an early indicator of subsequent symptomatic anastomotic leakage after anterior resection. Color Dis 10:75–80
Japanese Society for Cancer of the Colon and Rectum (2009) Japanese Classification of Colorectal Carcinoma (second English edition). Kanehara & Co Ltd, Tokyo
Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG (1992) CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol 13:606–608
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD et al (2009) The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Warschkow R, Beutner U, Steffen T, Muller SA, Schmied BM, Guller U et al (2012) Safe and early discharge after colorectal surgery due to C-reactive protein: a diagnostic meta-analysis of 1832 patients. Ann Surg 256:245–250
Fransen EJ, Maessen JG, Elenbaas TW, van Aarnhem EE, van Dieijen-Visser MP (1999) Enhanced preoperative C-reactive protein plasma levels as a risk factor for postoperative infections after cardiac surgery. Ann Thorac Surg 67:134–138
Moyes LH, Leitch EF, McKee RF, Anderson JH, Horgan PG, McMillan DC (2009) Preoperative systemic inflammation predicts postoperative infectious complications in patients undergoing curative resection for colorectal cancer. Br J Cancer 100:1236–1239
Nielsen HJ, Christensen IJ, Sorensen S, Moesgaard F, Brunner N (2000) Preoperative plasma plasminogen activator inhibitor type-1 and serum C-reactive protein levels in patients with colorectal cancer. The RANX05 Colorectal Cancer Study Group. Ann Surg Oncol 7:617–623
Crozier JE, McKee RF, McArdle CS, Angerson WJ, Anderson JH, Horgan PG et al (2007) Preoperative but not postoperative systemic inflammatory response correlates with survival in colorectal cancer. Br J Surg 94:1028–1032
Alexandrakis MG, Passam FH, Moschandrea IA, Christophoridou AV, Pappa CA, Coulocheri SA et al (2003) Levels of serum cytokines and acute phase proteins in patients with essential and cancer-related thrombocytosis. Am J Clin Oncol 26:135–140
Nozoe T, Korenaga D, Futatsugi M, Saeki H, Maehara Y, Sugimachi K (2003) Immunohistochemical expression of C-reactive protein in squamous cell carcinoma of the esophagus—significance as a tumor marker. Cancer Lett 192:89–95
Nakatsu T, Motoyama S, Maruyama K, Usami S, Sato Y, Miura M et al (2012) Tumoral CRP expression in thoracic esophageal squamous cell cancers is associated with poor outcomes. Surg Today 42:652–658
Nozoe T, Matsumata T, Sugimachi K (2000) Preoperative elevation of serum C-reactive protein is related to impaired immunity in patients with colorectal cancer. Am J Clin Oncol 23:263–266
Leitch EF, Chakrabarti M, Crozier JE, McKee RF, Anderson JH, Horgan PG et al (2007) Comparison of the prognostic value of selected markers of the systemic inflammatory response in patients with colorectal cancer. Br J Cancer 97:1266–1270
Canna K, McArdle PA, McMillan DC, McNicol AM, Smith GW, McKee RF et al (2005) The relationship between tumour T-lymphocyte infiltration, the systemic inflammatory response and survival in patients undergoing curative resection for colorectal cancer. Br J Cancer 92:651–654
Mold C, Rodriguez W, Rodic-Polic B, Du Clos TW (2002) C-reactive protein mediates protection from lipopolysaccharide through interactions with Fc gamma R. J Immunol 169:7019–7025
Sorensen LT, Hemmingsen U, Kallehave F, Wille-Jorgensen P, Kjaergaard J, Moller LN et al (2005) Risk factors for tissue and wound complications in gastrointestinal surgery. Ann Surg 241:654–658
Watanabe A, Kohnoe S, Shimabukuro R, Yamanaka T, Iso Y, Baba H et al (2008) Risk factors associated with surgical site infection in upper and lower gastrointestinal surgery. Surg Today 38:404–412
Kobayashi S, Gotohda N, Nakagohri T, Takahashi S, Konishi M, Kinoshita T (2009) Risk factors of surgical site infection after hepatectomy for liver cancers. World J Surg 33:312–317
Esrig BC, Frazee L, Stephenson SF, Polk HC Jr, Fulton RL, Jones CE (1977) The predisposition to infection following hemorrhagic shock. Surg Gynecol Obstet 144:915–917
Hartmann M, Jonsson K, Zederfeldt B (1992) Effect of tissue perfusion and oxygenation on accumulation of collagen in healing wounds. Randomized study in patients after major abdominal operations. Eur J Surg 158:521–526
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kubo, T., Ono, S., Ueno, H. et al. Elevated preoperative C-reactive protein levels are a risk factor for the development of postoperative infectious complications following elective colorectal surgery. Langenbecks Arch Surg 398, 965–971 (2013). https://doi.org/10.1007/s00423-013-1107-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-013-1107-0