Abstract
Eighty-two percent of sexually active women aged 15–44 have used oral contraceptive pills (OCP) in the United States. The OCP, an exogenous source of synthetic forms of steroid hormones, prevents ovulation. Hormone changes during the menstrual cycle (MC) are believed to have an impact on anterior cruciate ligament (ACL) laxity due to estrogen. Because the estrogen receptor β resides on human connective tissue, OCP may have potential impact on tendon and ligament synthesis, structure, and biomechanical properties. Temperature has also been known to have an effect on tissue elasticity. Therefore, the purpose of this study was to investigate the differences in ACL elasticity, force to flex the knee (FFK), and knee flexion–extension hysteresis (KFEH) between OCP users and non-OCP users. To investigate these changes, two different knee temperatures were measured. Nineteen young females were divided into two groups: OCP users and non-OCP users. Blood for estradiol serum concentration (E2) was taken before beginning the tests. ACL elasticity, FFK, and KFEH were assessed both at ambient temperature (22 °C) and after 38 °C warming of the leg to stabilize tissue temperature. Assessments were performed four times during the MC. Throughout the MC, ACL elasticity, FFK, and KFEH fluctuated in non-OCP users, but not in OCP users. At ambient temperature, ACL elasticity was significantly lower and FFK and KFEH were significantly higher in OCP users than non-OCP users (p < 0.05). But, no significant differences in FFK and KFEH between the two groups were found after warming to 38 °C.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Women have a greater incidence of Anterior Cruciate Ligament (ACL) injury than men (Vauhnik et al. 2008; Zazulak et al. 2006; Arendt et al. 1999; Griffin et al. 2000). This gender difference is commonly assumed to be due to anatomical, neuromuscular, movement patterns in women as well as hormonal influences (Griffin et al. 2000; Barber-Westin et al. 2009). Regarding hormonal factors, numerous studies have found a correlation between reproductive hormones and ACL injury risk (Vauhnik et al. 2008; Zazulak et al. 2006; Arendt et al. 1999; Griffin et al. 2000). The role of estrogen in possibly causing ACL injuries has recently been studied at the cellular level and the presence of 17-beta estradiol receptors in human ACL and muscle has been investigated (Yu et al. 1999; Liu et al. 1997; Hansen et al. 2009); Shultz et al. 2004). Previous studies have examined the changes in the levels of estrogen in blood as related to ACL laxity during the menstrual cycle and a correlation between ACL laxity and estrogen was detected (Yu et al. 1999; Liu et al. 1997; Hansen et al. 2009; Shultz et al. 2004).
The number of women using OCP has constantly increased. Eighty-two percent of sexually active women aged 15–44 have used the oral contraceptive pill (OCP) in the United States and 14 % of women have used OCP for non-contraceptive purposes such as cycle regulation, treatment of dysmenorrhea and amenorrhea (Kenny et al. 2008). OCP consists of combined estrogen and progesterone as synthetic steroids and it plays a role in suppressing pituitary Follicle-stimulating hormone (FSH) and Luteinizing hormone (LH) production and preventing ovulation from occurring (Kenny et al. 2008; Pokorny et al. 2000). This exogenous source of synthetic forms of the hormone prevents ovulation by maintaining more consistent hormone levels (Krishnan and Kiley 2010). The 17-beta estradiol receptors on human connective tissue are well known and, therefore, the OCP may have an impact on tendon and ligament synthesis, structure, and biomechanical properties. Also, Martineau and colleagues have shown that OCP users have less ACL laxity than non-OCP users (Martineau et al. 2004).
It is not surprising that many people do a warm-up exercise before sports activities to increase muscle and tendon extensibility to prevent injuries (Pasanen et al. 2009). Temperature is another factor that influences tendon and ligament of collagen synthesis. In healthy young adults, core temperature changes approximately 0.5 °C throughout the day. In women with a regular menstrual cycle, their core temperature fluctuates not only throughout the day but also during the menstrual cycle (Petrofsky et al. 2007). It peaks during the luteal phase while in the follicular and at ovulation it is relatively low (Petrofsky et al. 1976, 2007; Janse et al. 2012). The elevated thermoregulatory set point during the luteal phase is the most accepted explanation for the observed change in core temperature (Carpenter and Nunneley 1988; Cunningham and Cabanac 1971). Since soft tissue extensibility changes with different levels of tissue temperature, the menstrual cycle has dramatic effects on tissue extensibility. However, because hormones do not change in OCP users, their core temperature may change little during the menstrual cycle. In addition, Rogers and Baker have shown that OCP users have higher core temperature compared to non-OCP users due to exogenous forms of progesterone in OCPs (Rogers and Baker 1997).
Thus, the effect of estrogen on ACL elasticity and muscle and tendon flexibility is probably a complex interaction between the hormone and tissue temperature. Therefore, the purpose of this study was to investigate the differences in ACL elasticity, force to flex the knee (FFK), and knee flexion–extension hysteresis (KFEH) between OCP users and non-OCP users. To investigate these changes, two different knee temperatures were measured.
Methods
Subjects
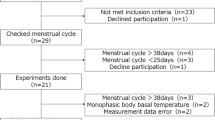
Nineteen non-athletic young healthy females volunteered to participate in this study. Subjects were divided into two groups: subjects with a regular menstrual cycle and those who are taking OCP according to their self-reporting. Subjects were 18–30 years of age with a Body Mass Index (BMI) between 15 and 30 who had a regular menstrual cycle or currently using low-dose OCP (<50 μg-ethinyl estradiol) for at least 6 months. Subjects had no history of pregnancy, neuropathy, myopathy or knee injury, and were not taking any medication that would affect sex hormones other than OCPs. All procedures and protocols were approved by Institutional Review Board of Loma Linda University and all subjects signed an informed consent.
Procedures
Subjects performed a total of four different tests throughout one full menstrual cycle. In the non-OCP group, testing occurred at menstruation (1–3 days after onset of menstruation), follicular phase (9–11 days after onset of menstruation), ovulation (13–16 days after onset of menstruation), and luteal phase (21–24 days after onset of menstruation). Since these phases do not occur in the OCP group, testing occurred at menstruation and match days with non-OCP group for OCP group. Subjects were asked to report the days of their cycle at the beginning of the study. OCP users were screened by questionnaire, which included questions regarding brand name, type, and the length of taking OCP. At the beginning of the study, subjects signed an informed consent before they participated in the study. Since the estradiol serum concentration in blood and body temperature fluctuates during the day, the various tests were performed at the same time each day.
On the first day, before beginning the experiment, height, weight, BMI, and self-reported menstrual cycle were measured. Upon arriving at the laboratory, subjects rested comfortably in a regulated temperature room at 22 °C for 20 min to stabilize their body temperature in a neutral environment. Blood samples (4 cc) were taken to analyze estradiol serum concentration before measuring leg skin temperature. Next, ACL elasticity, FFK, and KFEH were measured. After this, two 38 °C heat pads were placed on the subject’s quadriceps and knee for 20 min to stabilize their leg temperature. Skin temperature, ACL elasticity, FFK, and KFEH measurements were repeated.
Measurements
All measurements were performed by a trained researcher. The outcome variables assessed were ACL elasticity, force to flex the knee (FFK), knee flexion–extension hysteresis (KFEH), leg skin temperature, and estradiol serum concentration.
Estradiol (E2) serum concentration
Estradiol serum concentration was analyzed using the TOHSO E2 ST AIA assay (Fisher Healthcare, Inc., Houston, TX, USA). Four ml of blood was obtained from an antecubital vein with a 23-guage needle and centrifuged for separating serum from the whole blood. The centrifuge rotated at 3,000 rpm for 10 min (Beckman Coulter Inc., Brea, CA, USA). Once serum was separated, it was stored at −80 °C until all samples of serum were collected for the hormone analysis. The mean (SD) intra-assay concentration was 94.9 (9.0) with a coefficient variation percent (CV %) of 9.5. On the other hand, the mean (SD) inter-assay concentration was 100.5 (5.3) with a CV % of 5.3.
Leg skin temperature
Leg skin temperature was measured using the forward looking infrared 660 IR Camera (FLIR systems, Danderyd, Sweden). This device has been validated to deliver accurate temperature measurements (Al-Nakhli et al. 2012). To acquire best images, the readings were done at a perpendicular angle and at a distance of 1 m away from the skin. Measurements were performed in the room illuminated with light emitting diode (LED) lights to minimize any infrared interference (Al-Nakhli et al. 2012). The IR camera was calibrated in a water bath prior to the experiments and checked against a standard thermometer. Skin blood Baseline leg skin temperature was taken after stabilizing leg temperature at a neutral environment for 20 min and after applying 38 °C heat immediately when the heat pads were removed.
Anterior cruciate ligament elasticity
KT-2000 knee arthrometer (MEDmetric Corp, San Diego, California) was used to measure knee laxity of the anterior cruciate ligament. The measurement of the anterior knee ligament laxness was performed by one experienced examiner for consistency. The measurement tool was shown to be reliable over time, with an ICC of 0.92 (p = 0.0001) (Van Lunen et al. 2003). Subjects were asked to lay supine in a predetermined position. A strain gauge bridge arranged in a load cell was used to measure the force necessary to generate an anterior glide of the proximal end of the tibia on the femoral condyles. This generated a force versus displacement curve for the anterior cruciate ligaments. The process was accomplished by supporting both limbs with a firm, comfortable platform placed proximal to the popliteal space. This helped keep the subject’s knee flexion angle constant for the duration of the test. Along with this device, a foot support accessory supplied with the ARTHROMETER® positioned the feet symmetrically allowing the leg position to be optimal for the test while reducing external rotation. For the most comfortable position during the flexion angle test, knee flexion angle was initially at 25° and the only movement was the tibia in relation to the patella (Fig. 1). A thigh strap controlled hip external rotation while offering support to help relax the subject. Force used for the experiment was applied at 30 lbs (133 N) of force. The force displacement data were shown on an X–Y plotter. The vernier caliper was used to measure anterior tibial displacement (ATD) graph.
Muscle and tendon flexibility
The force measured to extend the knee from 90° to 125° was recorded. Elevated off the floor and in a seated position, the subject’s leg hung at an initial angle of 90°. To passively move the knee through 35° of flexion and extension, an ankle strap was connected to a linear actuator (Fig. 2). The measurement was recorded at a rate of movement of 45° in 7.5 s. The force in flexion and extension was measured with a strain gage bridge arranged as a load cell. The bridge was excited by 5 V. The output amplified with a gain of 500 (DAC 100, Bio Pac Systems, Goleta California). The output was then digitized at 2,000 Hz with a resolution of 24 bits on an MP150 Bio Pac data acquisition system (Bio Pac Systems, Goleta California). The knee goniometer, using a ruby bearing 360° 5,000 ohm potentiometer, measured the angle of the knee to calculate the force needed per degree moved. The previous study used by this CPM machine showed data were very constant. Overall, measurement errors from day to day did not exceed 1 %.
The difference between the FFK and force to extend the knee (FEK), called KFEH, was then calculated. Potential elastic energy stored during the loading (flexion) is greater than that of unloading (extension); thus, flexing the knee required greater force than extending the knee (Nordez et al. 2009). A lower elastic hysteresis value means more elasticity of the muscle and tendon (Fig. 3).
Control of quadriceps and knee temperature
Quadriceps and knee temperature were controlled with a Berg’s polar care therapy heat exchange unit (Berg Inc. East Carlsbad, CA, USA) maintained at 40 °C by a water bath. On the water bath, a heating water bath circulator (Fisher scientific Inc. Pittsburgh, PA, USA) was attached to control temperature. Since water temperature dropped about 2 °C throughout the unit, water temperature was kept at 40 °C to give 38 °C heat on subject’s knee and quadriceps.
Data analysis
Data were summarized using means and standard deviation (SD). An independent t test was conducted to compare general characteristics between OCP users and non-OCP users. One-way repeated measures analysis of variance (ANOVA) was used to examine changes in mean estradiol serum concentration, leg skin temperature, ACL elasticity, FFK, and KFEH at four different phases of the menstrual cycle. For significant findings, LSD pairwise comparisons test for multiple comparisons was used to compare means of variables between any two different phases. For all data collected over the phases within each test, a mixed factorial ANOVA was conducted to compare cycle phases with respect to the effect of estradiol concentration on ligament elasticity, FFK, and KFEH at room temperature and 38 °C in each group. The level of significance was set at p < 0.05.
Results
Nineteen subjects were enrolled in the study. However, one subject from the OCP group was excluded because the estradiol level was similar to that of a normal menstrual cycle subject. There were no significant differences in mean age, weight (kg), height (cm), BMI (kg/m2), and length of cycle (p > 0.05, Table 1). The subject’s menstrual phase was determined by their self-reporting and estradiol serum concentrations. Mean (SD) of the ATD, FFK, and KFEH at ambient temperature and 38 °C warming in four different phases during the menstrual cycle is shown in Tables 3, 4, 5.
Estradiol (E2) serum concentration
Mean and SD of estradiol serum concentrations in four different phases during the menstrual cycle is displayed in Table 2. There were significant changes in estradiol serum concentration across the menstrual cycle in the OCP user group (p < 0.001), but not in OCP group (Fig. 4; Table 2). The lowest estradiol concentration was found during menstruation (51.4 ± 9.0 pg/ml) and the highest estradiol concentration was found during ovulation (175.8 ± 45.9 pg/ml) in non-OCP user group (Table 2).
Leg skin temperature
Both knee and quadriceps skin temperatures were significantly lower during ovulation compared to luteal phase in non-OCP users (31.5 ± 0.8 vs. 31.8 ± 0.5, p = 0.04, 31.6 ± 0.7 vs. 31.9 ± 0.7, p = 0.04, Table 2).
Also, no significant differences in temperature were detected between OCP users and non-OCP users in all phases (p > 0.05),when two heat pads were applied on the knee, and quadriceps skin temperature significantly increased and held at 38 °C warming.
Anterior knee ligament elasticity
Anterior knee ligament elasticity was measured by ATD. The results of the ATD changes in four different phases during the menstrual cycle at ambient temperature and after 38 °C warming in non-OCP and OCP users are shown in Fig. 5. Among non-OCP users, the effect size within subjects was 0.23 for menstrual phase and 0.02 for OCP users. When comparing ATD in four different phases of the menstrual cycle, ATD was significantly lower in OCP users compared to non-OCP at both temperatures (Fig. 5). The greatest ATD was found at ovulation and the least ATD was found at menstruation in non-OCP users (Table 3). At ambient temperature, the ATD decreased by 10 % from ovulation to menstruation and the ATD differences between ovulation and menstruation were not significant in OCP users (p > 0.05, Table 3). After applying 38 °C warming, there were significant differences in ATD between OCP users and non-OCP users (p > 0.05). There was a significant difference in ATD between ovulation and menstruation in OCP users (6.0 ± 1.8 mm versus 5.6 ± 1.6 mm, p = 0.01, Table 3; Fig. 5).
Measurement of quadriceps muscle and tendon flexibility
Force to flex the knee (FFK)
The effect size for menstrual phase within subjects was 0.13 for non-OCP users and 0.03 for non-OCP users. The FFK decreased by 15 % from menstruation to ovulation at ambient temperature in non-OCP users (p = 0.04, Table 4). However, there were no significant changes in the FFK across the phases at 38 °C warming (p > 0.05). Also, a significant difference was found in the FFK between the ambient temperature and 38 °C warming in all phases except ovulation in which estradiol concentrations were relatively higher than those in other phases (Table 4). Both at ambient temperature and 38 °C warming, the FFK of OCP users was greater than non-OCP users in all phases (Table 4; Fig. 6). There was no significant difference in the FFK between pre and post heat in OCP users. On average, 9.5 % decrease was shown in OCP users versus 5.4 % decrease in non-OCP users (Table 4).
Knee flexion–extension hysteresis (KFEH)
The effect size for menstrual phase within subjects was 0.37 for non-OCP users and 0.04 for OCP users. At ambient temperature, the KFEH was significantly lower in OCP users than in non-OCP users. During ovulation, the KFEH was significantly lower in non-OCP users than in OCP users (27.0 ± 6.0 N versus 34.9 ± 11.2 N, p < 0.01, Table 5). Across phases, there were no significant changes in the KFEH in non-OCP users (p = 0.01) but not in OCP users (p = 0.72). The KFEH increased by 24 % from ovulation to menstruation at ambient temperature in non-OCP users. In addition, there were no significant changes in the KFEH across the menstrual cycle at 38 °C warming in OCP users (p > 0.05). In both groups, the KFEH was significantly lower at 38 °C warming when compared to ambient temperature in all phases except ovulation. After 38 °C warming the KFEH decreased 21.1 % in OCP users and 14.0 % in non-OCP users (Fig. 7; Table 5).
Discussion
ACL elasticity and muscle and tendon flexibility are major risk factors for knee injuries during sports (Eastlack et al. 1999; Musahl et al. 2012). Women have fluctuating estrogen during the menstrual cycle and are more susceptible to have injuries (Chaudhari et al. 2007). In previous studies, women had greater knee laxity during ovulation at a time when estrogen level peaks (Park et al. 2009a, b; Heitz et al. 1999). These results are supported by the finding that estrogen receptors are found in connective tissue and thus it changes the mechanical properties of its tendons and ligaments (Liu et al. 1997; Heitz et al. 1999). However, OCP makes women’s hormone level more consistent during the menstrual cycle. If it is true that female reproductive hormones cause connective tissue laxness, female OCP users should show more stable tissue extensibility. Therefore, it is of no surprise that the few studies addressing the effects of OCP on knee injury prevention show little change in ligament elasticity during the menstrual cycle (Ruedl et al. 2009; Bell et al. 2011). Researchers, however, have reached different conclusions on the relationship between OCP and knee laxity (Martineau et al. 2004; Bell et al. 2011).
In the present investigation, ACL elasticity, FFK, and KFEH were measured during four different phases of the menstrual cycle with subjects exposed to ambient temperatures. In addition, to stabilize temperature fluctuation from the day, the experiments were repeated by warming the leg to 38 °C in both young healthy OCP and non-OCP users. We have found that non-OCP users have a greater ACL elasticity, less FFK, and KFEH in all phases compared to OCP users at ambient temperature. We further found that non-OCP users’ biomechanical outcome variables were altered throughout the menstrual cycle, but not in OCP users during the menstrual cycle. When comparing estradiol serum concentration between the two groups, OCP users’ estradiol levels were lower in all phases and did not alter during the menstrual cycle. These results imply that estradiol serum concentration has an impact on human ligament, muscle, and tendon. In other words, more knee stiffness was found in women on OCP. Here estradiol was lower in blood.
Tissue temperature is one of the factors that alter knee elasticity (Jarosch 2011) and heat is commonly used to reduce soft tissue stiffness (LaBella et al. 2011). Since basal body temperature fluctuates during the menstrual cycle, it is used to accurately detect if women are ovulating. This change is also influenced by progesterone and estrogen during the menstrual cycle (Buxton and Atkinson 1948; Devi and Reddy 1956) but not in OCP users. Previous research found that muscle temperature increased on ovulation and it continuously remaind elevated during the luteal phase (Petrofsky et al. 1976, 2007). Please check and confirm the edit in the following sentence: To increase central core temperature, the skin removes less heat to reduce body temperature. In non-OCP users, muscle and shell tissue temperature fluctuate during the menstrual cycle; thus playing an important role in knee elasticity.
In addition, there were heat effects on muscle and tendon flexibility both in non-OCP and OCP users. The FFK and KFEH significantly decreased after 38 °C warming of the leg in all phases in OCP users. In a similar manner, knee flexibility was significantly reduced after using heat in all phases of the menstrual cycle except ovulation, where estradiol serum concentration was relatively higher in non-OCP users. These results imply that muscle and tendon flexibility is more affected by temperature than estrogen. Interestingly, we found that FFK and KFEH decreased more after 38 °C warming in OCP users compared to non-OCP users during the menstrual cycle. This indicated more effect of heat on FFK and KFEH in OCP users. Thus, using heat increases knee flexibility in OCP users and is still beneficial to non-OCP users during menstruation where estradiol levels are relatively low. However, for the ACL, the effects of estradiol were different. The ATD did not significantly decrease after 38 °C warming in both groups of subjects. Also, it was significantly higher during ovulation than menstruation after heat.
ACL elasticity, muscle and tendon flexibility are related to knee injuries (Li et al. 2002). Women who are taking OCP have less knee laxity due to estradiol effects during menstruation. Previous studies have examined the association between ACL injuries and use of oral contraceptives (Ruedl et al. 2009; Bennell et al. 1999). However, results from these studies were perhaps inconclusive because they did not examine the effect of both knee elasticity and tissue temperature. It is not easy to examine the effects of OCP on ACL injuries only with ACL elasticity. Other factors should be considered such as tissue temperature. Thus, in further investigation, both estrogen and tissue temperature should be considered as key risk factors that can cause ACL injuries during menstrual cycle in both OCP and non-OCP users.
In addition, interestingly, it is common to do a warm up prior to exercise to reduce injuries since less elasticity is related to tissue tears. However, in women, the reverse seems to be true. Perhaps, the structure strength (e.g. collagen cross bridges) is also altered by estrogen. This may explain differences in the results of some studies on women versus men. These knee injuries may be caused by changes in collagen strength not just elasticity. Estrogen may not only alter ACL elasticity, but may cause a change in the breaking strength of the ACL. Just as bone can fracture due to glycogen crosslinking even when it is dense, there may be a similar relationship with collagen in ligaments whereby they may tear even if elastic. This would involve a shift in the force–stress curve for the ACL making the elastic region shorter and the plastic region larger due to estrogen. There are no studies on structural strength of the ACL in relation to estrogen, only elasticity. It will be interesting to see if there are collagen structure strength changes during the menstrual cycle and its relationship to incidence of knee injuries in OCP users and non-OCP users.
Conclusion
Throughout the MC, ACL elasticity, FFK, and KFEH fluctuated in non-OCP users but not in OCP users. At ambient temperature, ACL elasticity was significantly lower and FFK and KFEH were significantly higher in OCP users than in non-OCP users. However, no significant differences in FFK and KFEH between the two groups were found after warming to 38 °C. These imply that muscle and tendon flexibility is more affected by temperature than estrogen. Also, we found that FFK and KFEH decreased more after 38 °C warming in OCP users and it indicated more effect of heat on FFK and KFEH in OCP users but no ACL elasticity changes after 38 °C warming in both groups of subjects. Thus, using heat increases knee muscle and tendon flexibility in OCP users and is still beneficial to non-OCP users during menstruation where estradiol levels are relatively low.
References
Al-Nakhli HH, Petrofsky JS, Laymon MS, Berk LS (2012) The use of thermal infra-red imaging to detect delayed onset muscle soreness. J Vis Exp (59). doi:10.3791/3551
Arendt EA, Agel J, Dick R (1999) Anterior cruciate ligament injury patterns among collegiate men and women. J Athl Train 34:86–92
Barber-Westin SD, Noyes FR, Smith ST, Campbell TM (2009) Reducing the risk of noncontact anterior cruciate ligament injuries in the female athlete. Phys Sportsmed 37:49–61
Bell DR, Blackburn JT, Ondrak KS et al (2011) The effects of oral contraceptive use on muscle stiffness across the menstrual cycle. Clin J Sport Med 21:467–473
Bennell K, White S, Crossley K (1999) The oral contraceptive pill: a revolution for sportswomen? Br J Sports Med 33:231–238
Buxton CL, Atkinson WB (1948) Hormonal factors involved in the regulation of basal body temperature during the menstrual cycle and pregnancy. J Clin Endocrinol Metab 8:544–549
Carpenter AJ, Nunneley SA (1988) Endogenous hormones subtly alter women’s response to heat stress. J Appl Physiol 65:2313–2317
Chaudhari AM, Lindenfeld TN, Andriacchi TP et al (2007) Knee and hip loading patterns at different phases in the menstrual cycle: implications for the gender difference in anterior cruciate ligament injury rates. Am J Sports Med 35:793–800
Cunningham DJ, Cabanac M (1971) Evidence form behavioral thermoregulatory responses of a shift in setpoint temperature related to the menstrual cycle. J de physiologie 63:236–238
Devi SP, Reddy DV (1956) Basal body temperature during the menstrual cycle in young women. J Indian Med Assoc 27:313–316
Eastlack ME, Axe MJ, Snyder-Mackler L (1999) Laxity, instability, and functional outcome after ACL injury: copers versus noncopers. Med Sci Sports Exerc 31:210–215
Griffin LY, Agel J, Albohm MJ et al (2000) Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg 8:141–150
Hansen M, Kongsgaard M, Holm L et al (2009) Effect of estrogen on tendon collagen synthesis, tendon structural characteristics, and biomechanical properties in postmenopausal women. J Appl Physiol 106:1385–1393
Heitz NA, Eisenman PA, Beck CL, Walker JA (1999) Hormonal changes throughout the menstrual cycle and increased anterior cruciate ligament laxity in females. J Athl Train 34:144–149
Janse DEJXA, Thompson MW, Chuter VH, Silk LN, Thom JM (2012) Exercise performance over the menstrual cycle in temperate and hot, humid conditions. Med Sci Sports Exerc 44:2190–2198
Jarosch R (2011) The different muscle-energetics during shortening and stretch. Int J Mol Sci 12:2891–2900
Kenny GP, Leclair E, Sigal RJ et al (2008) Menstrual cycle and oral contraceptive use do not modify postexercise heat loss responses. J Appl Physiol 105:1156–1165
Krishnan S, Kiley J (2010) The lowest-dose, extended-cycle combined oral contraceptive pill with continuous ethinyl estradiol in the United States: a review of the literature on ethinyl estradiol 20 mug/levonorgestrel 100 mug + ethinyl estradiol 10 mug. Int J Womens Health 2:235–239
LaBella CR, Huxford MR, Grissom J, Kim KY, Peng J, Christoffel KK (2011) Effect of neuromuscular warm-up on injuries in female soccer and basketball athletes in urban public high schools: cluster randomized controlled trial. Arch Pediatr Adolesc Med 165(11):1033–1040
Li G, Suggs J, Gill T (2002) The effect of anterior cruciate ligament injury on knee joint function under a simulated muscle load: a three-dimensional computational simulation. Ann Biomed Eng 30:713–720
Liu SH, Al-Shaikh RA, Panossian V, Finerman GA, Lane JM (1997) Estrogen affects the cellular metabolism of the anterior cruciate ligament. A potential explanation for female athletic injury. Am J Sports Med 25:704–709
Martineau PA, Al-Jassir F, Lenczner E, Burman ML (2004) Effect of the oral contraceptive pill on ligamentous laxity. Clin J Sport Med 14:281–286
Musahl V, Seil R, Zaffagnini S, Tashman S, Karlsson J (2012) The role of static and dynamic rotatory laxity testing in evaluating ACL injury. Knee Surg Sports Traumatol Arthrosc 20:603–612
Nordez A, McNair PJ, Casari P, Cornu C (2009) The effect of angular velocity and cycle on the dissipative properties of the knee during passive cyclic stretching: a matter of viscosity or solid friction. Clin Biomech (Bristol, Avon) 24:77–81
Park SK, Stefanyshyn DJ, Ramage B, Hart DA, Ronsky JL (2009a) Relationship between knee joint laxity and knee joint mechanics during the menstrual cycle. Br J Sports Med 43:174–179
Park SK, Stefanyshyn DJ, Loitz-Ramage B, Hart DA, Ronsky JL (2009b) Changing hormone levels during the menstrual cycle affect knee laxity and stiffness in healthy female subjects. Am J Sports Med 37:588–598
Pasanen K, Parkkari J, Pasanen M, Kannus P (2009) Effect of a neuromuscular warm-up programme on muscle power, balance, speed and agility: a randomised controlled study. Br J Sports Med 43:1073–1078
Petrofsky JS, LeDonne DM, Rinehart JS, Lind AR (1976) Isometric strength and endurance during the menstrual cycle. Eur J Appl Physiol Occup Physiol 35:1–10
Petrofsky J, Al Malty A, Suh HJ (2007) Isometric endurance, body and skin temperature and limb and skin blood flow during the menstrual cycle. Med Sci Monit 13:CR111–CR117
Pokorny MJ, Smith TD, Calus SA, Dennison EA (2000) Self-reported oral contraceptive use and peripheral joint laxity. J Orthop Sports Phys Ther 30:683–692
Rogers SM, Baker MA (1997) Thermoregulation during exercise in women who are taking oral contraceptives. Eur J Appl Physiol Occup Physiol 75:34–38
Ruedl G, Ploner P, Linortner I et al (2009) Are oral contraceptive use and menstrual cycle phase related to anterior cruciate ligament injury risk in female recreational skiers? Knee Surg Sports Traumatol Arthrosc 17:1065–1069
Shultz SJ, Kirk SE, Johnson ML, Sander TC, Perrin DH (2004) Relationship between sex hormones and anterior knee laxity across the menstrual cycle. Med Sci Sports Exerc 36:1165–1174
Van Lunen BL, Roberts J, Branch JD, Dowling EA (2003) Association of menstrual-cycle hormone changes with anterior cruciate ligament laxity measurements. J Athl Train 38:298–303
Vauhnik R, Morrissey MC, Rutherford OM, Turk Z, Pilih IA, Pohar M (2008) Knee anterior laxity: a risk factor for traumatic knee injury among sportswomen? Knee Surg Sports Traumatol Arthrosc 16:823–833
Yu WD, Liu SH, Hatch JD, Panossian V, Finerman GA (1999) Effect of estrogen on cellular metabolism of the human anterior cruciate ligament. Clin Orthop Relat Res 366:229–238
Zazulak BT, Paterno M, Myer GD, Romani WA, Hewett TE (2006) The effects of the menstrual cycle on anterior knee laxity: a systematic review. Sports Med 36:847–862
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Fabio Fischetti.
Rights and permissions
About this article
Cite this article
Lee, H., Petrofsky, J.S., Daher, N. et al. Differences in anterior cruciate ligament elasticity and force for knee flexion in women: oral contraceptive users versus non-oral contraceptive users. Eur J Appl Physiol 114, 285–294 (2014). https://doi.org/10.1007/s00421-013-2771-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-013-2771-z