Abstract
Purpose
To investigate the prevalence and characteristics of paravascular inner retinal abnormalities in healthy eyes.
Materials and methods
In this prospective observational case series, we included 178 healthy eyes (178 patients) with no ocular diseases. Eyes with co-existing ocular diseases, e.g., epiretinal membrane, glaucoma, or high myopia, were excluded from the current study. The posterior pole and paravascular areas of the temporal arcade vessels were comprehensively examined by dense radial scanning of optical coherence tomography (OCT) with the extended field imaging technique.
Results
On fundus photography, no inner retinal abnormalities were detected along the temporal arcade vessels. On OCT sections, paravascular inner retinal abnormalities were seen in 77 (43.3%) eyes. In 71 (39.9%) eyes, inner retinal cystoid or fissure-like spaces that had no connection to the vitreous cavity were seen adjacent to the temporal arcade vessels. Most of these lesions were detected only on several consecutive OCT sections. In four (2.2%) eyes, inner retinal cleavages with openings to the vitreous cavity were seen adjacent to the temporal arcade vessels. These lesions were more frequently detected in the inferior hemisphere and along the major retinal veins. No eyes showed typical broad defects of the inner retinal tissue. There were no significant differences in age, gender, visual acuity, refractive error, or axial length between eyes with or without paravascular inner retinal abnormalities.
Conclusions
Paravascular cystoid or fissure-like spaces were frequently seen in the inner retina of healthy eyes. However, we detected no typical paravascular inner retinal defects in healthy eyes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In a study using optical coherence tomography (OCT), Muraoka et al. [1] recently reported the characteristics and pathogenesis of inner retinal abnormalities along the major retinal vessels in eyes with high myopia and/or epiretinal membrane (ERM). These paravascular abnormalities are not simple inner retinal cleavages, but are inner retinal defects, often accompanied by a functional abnormality. Based on detailed observation of their cases, the authors designated these lesions as paravascular inner retinal defects (PIRDs) [1]. In eyes with high myopia, deviation of retinal vessels due to axial elongation would contribute to the development of PIRDs [2]. In eyes with ERM, the tractional force induced by ERM may cause deviation of the retinal vessels toward the central macula, leading to formation of PIRDs adjacent to the temporal arcade vessels [3, 4].
Recently, Miyoshi et al. [5] have reported that eyes with ERM were frequently accompanied by various types of inner retinal abnormalities along the temporal arcade vessels, such as cystoid or fissure-like spaces, cleavages, and broad defects. The authors have expanded the spectrum of PIRDs. Paravascular inner retinal cleavages with openings to the vitreous cavity were defined as grade 2 PIRDs, while inner retinal cleavages or cystoid spaces adjacent to the major retinal vessels were defined as grade 1 PIRDs. Original broad defects of the inner retinal tissue along the major retinal vessels were defined as grade 3 PIRDs. Similarly, on circumpapillary OCT sections of eyes of glaucoma patients and glaucoma-suspect patients, Hood et al. [6] and Xin et al. [7] reported paravascular defects (hypodense holes) as inner retinal abnormalities that could be observed adjacent to major retinal vessels. This glaucoma-associated feature overlaps with ERM-associated grade 1 PIRDs. However, these previous studies were performed mainly in eyes with specific ocular diseases.
Therefore, it remains unclear whether these paravascular abnormalities are absent from the inner retina of healthy eyes. In the current study, therefore, we prospectively examined consecutive healthy eyes without any ocular disease, using dense OCT sectioning, in order to elucidate the prevalence and characteristics of paravascular inner retinal abnormalities in healthy eyes.
Patients and methods
This prospective study was approved by the Ethics Committee of Kagawa University Faculty of Medicine and conducted in accordance with the tenets of the Declaration of Helsinki. Written informed consent was obtained from each subject before any study procedures or examinations were performed.
Patients
This prospective study consisted of 178 healthy eyes of 178 patients who were examined at the Department of Ophthalmology of Kagawa University Hospital between January 2015 and September 2016. The current study included only one eye of each subject. In the current study, eyes with any co-existing fundus disease (e.g., ERM, diabetic retinopathy, retinal vein or artery occlusion, hypertension retinopathy, age-related macular degeneration, or retinal degenerative diseases) were excluded. Eyes with high myopia (refractive error of less than −6 diopters or an axial length of more than 26.5 mm), glaucoma, or with a history of ocular surgery, except for cataract surgery, were also excluded from the current study.
Each patient underwent a comprehensive ophthalmic examination to measure the best-corrected visual acuity (BCVA) using a Landolt chart, refractive error, keratometry, intraocular pressure, and axial length measurement using partial coherence interferometry (IOL-Master, Carl Zeiss Meditec, Jena, Germany). Fundus biomicroscopy with a non-contact lens, 45° digital fundus photography (TRC-50LX; Topcon, Tokyo, Japan), and detailed OCT examinations (Spectralis HRA + OCT, Heidelberg Engineering, Heidelberg, Germany) were performed after pupil dilation.
OCT examination of paravascular inner retinal abnormalities
In each eye, the posterior pole was first examined using Spectralis HRA + OCT, with a novel extended-field imaging (EFI) technique [8]. Briefly, the EFI technique involved imaging the posterior pole through trial frames fitted with a + 20-diopter lens. The placement of a convex lens between the eye and the OCT probe increases the imaging light incidence angle, resulting in expansion of the imaging field. With the use of Spectralis HRA + OCT, the EFI technique allowed us to capture images with a 1.45- to 1.49-fold increase in the scan length as compared with conventionally obtained images [8]. For comprehensive detection of paravascular inner retinal abnormalities, the posterior pole and paravascular areas of both the superotemporal and inferotemporal arcade vessels were examined with dense radial scanning by Spectralis HRA + OCT using the EFI technique (Fig. 1). B-scan images were obtained radially at 7.5-degree intervals (24 sections) through the fovea centralis; a total of 40 B-scan images were averaged.
Examination of inner retinal abnormalities along the temporal arcade retinal vessels using optical coherence tomography (OCT). A) A monochromatic image and an OCT section obtained without using the extended field imaging (EFI) technique. B) A monochromatic image and an OCT section obtained using the EFI technique. The EFI technique allowed us to capture images with a 1.45- to 1.49-fold greater scan length than that of conventional OCT images. Red arrowhead = retinal artery; blue arrowhead = retinal vein
Paravascular inner retinal abnormalities were classified according to a report of Miyoshi et al. [5]. On OCT, typical defects of the inner retinal tissue adjacent to the major retinal vessels were defined as grade 3 PIRDs. Paravascular inner retinal cleavages that showed openings to the vitreous cavity, with no apparent defect of the inner retinal tissue, were defined as grade 2 PIRDs. Paravascular inner retinal cystoid or fissure-like spaces that showed no connection to the vitreous cavity were defined as grade 1 PIRDs. In eyes with multiple PIRDs, the higher grade was used to define the grade of the eye.
Statistical analysis
All values are presented as the means ± standard deviation. The statistical analysis was performed using PASW Statistics, version 21.0 (SPSS, Chicago, IL, USA). For statistical analysis, the VA measured by means of a Landolt chart was converted to a logarithm of the minimum angle of resolution (logMAR). The Student’s t test was performed to compare quantitative data that were normally distributed and had equal variance. Significant differences in the sampling distributions were determined using the chi-square test. A p value of less than 0.05 was considered to be statistically significant.
Results
In the current study, we evaluated 178 healthy eyes (178 subjects) with no ocular diseases (72 women and 106 men; Table 1). The mean axial length was 23.60 ± 1.06 mm. Twenty-six eyes were pseudophakic.
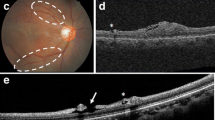
On fundus photographs, no retinal abnormalities were detected adjacent to the temporal arcade vessels. However, dense radial scanning by Spectralis HRA + OCT using the EFI technique showed paravascular inner retinal abnormalities along the temporal arcade vessels in 77 (43.3%) eyes. In 71 (39.9%) eyes, transverse OCT sections of the retinal arcade vessels showed paravascular cystoid or fissure-like spaces that had no connection to the vitreous cavity (PIRD grade 1). Most of these cystoid or fissure-like spaces were detected on single or several consecutive OCT sections; they seemed to have a short lesion length (Fig. 2). In 4 (2.2%) eyes, OCT sections showed paravascular inner retinal cleavages with openings to the vitreous cavity (PIRD grade 2; Fig. 3). No eyes showed typical broad defects of the inner retinal tissue (PIRD grade 3).
Paravascular inner retinal cystoid or fissure-like spaces that showed no connection to the vitreous cavity seen in a healthy eye without any ocular disease. A) Fundus imaging shows no inner retinal abnormalities. B–F) Monochromatic images and optical coherence tomography sections obtained with an extended field imaging technique. Cystoid or fissure-like spaces that had no connection to the vitreous cavity were seen adjacent to the inferotemporal artery. Red arrowhead= paravascular cystoid or fissure-like space; green arrowhead = retinal artery
Paravascular inner retinal cleavage that shows openings to the vitreous cavity, seen in a healthy eye without any ocular disease. A, B) Monochromatic images and optical coherence tomography (OCT) sections obtained with an extended field imaging technique. An inner retinal cleavage was seen along the inferotemporal retinal vein. C, D) Monochromatic images and OCT sections that were longitudinal to the major retinal vessels. Retinal cleavage seemed to extend beneath the vein. No apparent defect of the inner retinal tissue is seen. White arrow = paravascular inner retinal cleavage; red arrowhead = retinal artery; blue arrowhead = retinal vein
Paravascular inner retinal abnormalities were more frequently detected in the inferior than in the superior hemisphere; 19 eyes only demonstrated these abnormalities in the superior hemisphere and 39 eyes only in the inferior hemisphere, while the remaining 19 eyes demonstrated these in both hemispheres. OCT examinations revealed vitreous traction on the inner retinal tissue and the retinal vessels. Of 71 eyes with paravascular cystoid or fissure-like spaces, 9 showed vitreous adhesion to major retinal vessels.
Table 1 presents the ocular characteristics of eyes with or without paravascular inner retinal abnormalities. There were no significant differences in age, gender, VA, refractive error, axial length, or rate of systemic diseases between eyes with or without paravascular inner retinal abnormalities.
Discussion
Originally, a PIRD was defined as a defect of the inner retina, adjacent to the major retinal vessels, as a feature in eyes with high myopia and/or ERM. However, previous reports did not mention PIRDs in healthy eyes [1, 5, 9,10,11,12,13,14]. In the current study, we studied the posterior pole and paravascular areas of the temporal arcade vessels of 178 healthy eyes with dense radial OCT scanning, using the EFI technique. However, no eyes showed a typical broad defect of the inner retina as reported by Muraoka et al. [1]. A force would be required to cause the major retinal vessels to deviate, leading to formation of PIRDs.
Miyoshi et al. [5] showed that the original PIRDs included the paravascular inner retinal cystoid or fissure-like spaces that show no connection to the vitreous cavity and the paravascular inner retinal cleavages with openings to the vitreous cavity. Of our 178 patients, 77 (43.3%) eyes showed paravascular cystoid or fissure-like spaces or cleavages in the inner retina. In a previous report on 81 eyes with ERMs, 31 (38.3%) eyes demonstrated these lesions along the temporal arcade vessels (grade 1 in 6 eyes, grade 2 in 4 eyes, and grade 3 in 21 eyes) [5]. ERM often showed a typical broad defect in the inner retina (grade 3, typical PIRDs). In healthy eyes, although typical PIRDs were very rare, the paravascular cystoid or fissure-like spaces in the inner retina would be common.
These paravascular inner retinal abnormalities were also reported in eyes with high myopia or glaucoma. Shimada et al. studied 287 eyes with high myopia and found paravascular retinal cysts in 49.5% and paravascular lamellar holes in 26.8% [15]. In addition, Lee et al. [16] observed peripapillary retinoschisis in glaucomatous eyes as hyporeflective spaces within the inner retina. In addition, Xin et al. [7] found paravascular hypodense holes in the retinal nerve fiber layer on circumpapillary OCT sections in 33 (16%) of 208 eyes with glaucoma and suspected glaucoma. In addition to the nerve fiber layer defects [17], glaucomatous eyes showed various morphological features in the inner retina on OCT sections [18]. However, Xin et al. [7] also reported that these paravascular features were absent from control healthy eyes. Although the authors evaluated only a single circumpapillary OCT section, we adopted dense radial scanning to avoid missing even a miniscule lesion. The discrepancy in the healthy eyes may be explained by the density of OCT sectioning.
On fundus photography, PIRDs often appear as spindle- or caterpillar-shaped dark areas along the major retinal vessels. In healthy eyes of our subjects [1], however, no paravascular abnormalities could be detected on fundus photographs. In our subjects, most of the paravascular abnormalities were seen only on single or several consecutive OCT sections. Because their lesion length was expected to be short, it would be difficult to detect these on fundus photographs. In a previous report by Hood et al. [6], 10 (37.0%) of 27 paravascular defects seen in glaucoma patients or glaucoma-suspect patients were <1.0 mm in length. Although we did not measure the length of the paravascular spaces, it would be smaller than the PIRDs originally reported in eyes with high myopia and/or ERM [1].
In eyes with high myopia, Shimada et al. [15] suggested that paravascular lamellar holes developed when the inner wall of paravascular retinal cysts was avulsed by vitreous traction. In eyes with ERM and/or high myopia, OCT sections clearly showed that the posterior vitreous membrane sometimes adhered to the retinal surface around the PIRDs and seemed to contribute to the opening of their inner surface. In the healthy eyes of our subjects, while nine eyes with paravascular cystoid or fissure-like spaces showed vitreous adhesion to major retinal vessels, no eyes with paravascular inner retinal cleavages showed vitreous adhesion. Vitreous traction might be involved in the formation of retinal cleavages by the detachment of their inner surface.
The current study has several limitations. First, this study was cross-sectional, without follow-up. We could thus provide no information on the longitudinal change of PIRDs over time. Second, the current study did not include Goldmann perimetry; therefore, we could not assess the association between our findings on the retinal functions. Third, consistent with previous reports, paravascular inner retinal abnormalities in our subjects were more frequently seen along the retinal veins [1]. However, these lesions were more often detected in the inferior hemisphere. This is not consistent with previous reports, and the reason, therefore, is unclear [5, 11].
Despite these shortcomings, we have here described the prevalence and characteristics of paravascular inner retinal abnormalities in healthy eyes. Paravascular cystoid or fissure-like spaces were frequently seen in healthy eyes. However, we could not detect any typical PIRDs that were accompanied by broad defects of the inner retinal tissue. Further prospective cohort studies with longer follow-up periods are necessary to confirm the natural course of these lesions.
References
Muraoka Y, Tsujikawa A, Hata M, Yamashiro K, Ellabban AA, Takahashi A, Nakanishi H, Ooto S, Tanabe T, Yoshimura N (2015) Paravascular inner retinal defect associated with high myopia or epiretinal membrane. JAMA Ophthalmol 133:413–420
Sayanagi K, Ikuno Y, Gomi F, Tano Y (2005) Retinal vascular microfolds in highly myopic eyes. Am J Ophthalmol 139:658–663
Kishi S (2016) Vitreous anatomy and the vitreomacular correlation. Jpn J Ophthalmol 60:239–273
Nitta E, Shiraga F, Shiragami C, Fukuda K, Yamashita A, Fujiwara A (2013) Displacement of the retina and its recovery after vitrectomy in idiopathic epiretinal membrane. Am J Ophthalmol 155:1014–1020 e1011
Miyoshi Y, Tsujikawa A, Manabe S, Nakano Y, Fujita T, Shiragami C, Hirooka K, Uji A, Muraoka Y (2016) Prevalence, characteristics, and pathogenesis of paravascular inner retinal defects associated with epiretinal membranes. Graefes Arch Clin Exp Ophthalmol 254:1941–1949
Hood DC, De Cuir N, Mavrommatis MA, Xin D, Muhammad H, Reynaud J, Ritch R, Fortune B (2016) Defects along blood vessels in glaucoma suspects and patients. Invest Ophthalmol Vis Sci 57:1680–1686
Xin D, Talamini CL, Raza AS, de Moraes CG, Greenstein VC, Liebmann JM, Ritch R, Hood DC (2011) Hypodense regions (holes) in the retinal nerve fiber layer in frequency-domain OCT scans of glaucoma patients and suspects. Invest Ophthalmol Vis Sci 52:7180–7186
Uji A, Yoshimura N (2015) Application of extended field imaging to optical coherence tomography. Ophthalmology 122:1272–1274
Chihara E (2015) Myopic cleavage of retinal nerve fiber layer assessed by split-spectrum amplitude-decorrelation angiography optical coherence tomography. JAMA Ophthalmol 133:e152143
Chihara E, Chihara K (1992) Apparent cleavage of the retinal nerve fiber layer in asymptomatic eyes with high myopia. Graefes Arch Clin Exp Ophthalmol 230:416–420
Hwang YH, Kim YY, Kim HK, Sohn YH (2015) Characteristics of eyes with inner retinal cleavage. Graefes Arch Clin Exp Ophthalmol 253:215–220
Komeima K, Ito Y, Nakamura M, Terasaki H (2010) Inner retinal cleavage associated with idiopathic epiretinal membrane. Retin Cases Brief Rep 4:132–134
Komeima K, Kikuchi M, Ito Y, Terasaki H, Miyake Y (2005) Paravascular inner retinal cleavage in a highly myopic eye. Arch Ophthalmol 123:1449–1450
Tuulonen A, Yalvac IS (2000) Pseudodefects of the retinal nerve fiber layer examined using optical coherence tomography. Arch Ophthalmol 118:575–576
Shimada N, Ohno-Matsui K, Nishimuta A, Moriyama M, Yoshida T, Tokoro T, Mochizuki M (2008) Detection of paravascular lamellar holes and other paravascular abnormalities by optical coherence tomography in eyes with high myopia. Ophthalmology 115:708–717
Lee EJ, Kim TW, Kim M, Choi YJ (2014) Peripapillary retinoschisis in glaucomatous eyes. PLoS One 9:e90129
Nukada M, Hangai M, Mori S, Nakano N, Nakanishi H, Ohashi-Ikeda H, Nonaka A, Yoshimura N (2011) Detection of localized retinal nerve fiber layer defects in glaucoma using enhanced spectral-domain optical coherence tomography. Ophthalmology 118:1038–1048
Hasegawa T, Akagi T, Yoshikawa M, Suda K, Yamada H, Kimura Y, Nakanishi H, Miyake M, Unoki N, Ikeda HO, Yoshimura N (2015) Microcystic inner nuclear layer changes and retinal nerve fiber layer defects in eyes with glaucoma. PLoS One 10:e0130175
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Research involving human participants
This prospective study was approved by the Ethics Committee of Kagawa University Faculty of Medicine and conducted in accordance with the tenets of the Declaration of Helsinki.
Informed consent
Written informed consent was obtained from each subject before any study procedure or examination was performed.
Rights and permissions
About this article
Cite this article
Osaka, R., Manabe, S., Miyoshi, Y. et al. Paravascular inner retinal abnormalities in healthy eyes. Graefes Arch Clin Exp Ophthalmol 255, 1743–1748 (2017). https://doi.org/10.1007/s00417-017-3717-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-017-3717-7