Abstract
Background and purpose
Data on procedure time (PT) for mechanical thrombectomy (MT) are scarce. Moreover, the relationship among PT, postprocedural hemorrhagic transformation (HT), and functional outcomes in MT patients remains unclear. We investigated whether postprocedural HT mediated the relationship between PT and functional outcomes in patients with stent-retriever thrombectomy.
Methods
We retrospectively analyzed consecutive patients who underwent MT at two comprehensive stroke centers. PT was defined as the time from puncture to first successful recanalization or to abortion of the procedure if successful recanalization was not achieved. A favorable outcome was defined as a 90-day modified Rankin Scale score of 0–2. HT was classified using the European Cooperative Acute Stroke Study definition.
Results
Among 283 patients (mean age, 67.2 ± 11.9 years; male, 53.7%), 124 (43.8%) patients had a favorable outcome and 27 (9.5%) patients experienced symptomatic intracranial hemorrhage (sICH). Whether in the overall cohort or in the successful recanalization cohort, extended PT was an independent predictor for a poor outcome (per 30 min: OR 1.433, 95% CI 1.062–1.865, p = 0.019; OR 1.522, 95% CI 1.062–2.159, p = 0.020, respectively) and sICH (per 30 min: OR 1.391, 95% CI 1.030–1.865, p = 0.029; OR 1.716, 95% CI 1.161–2.648, p = 0.009, respectively). Moreover, postprocedural HT might partially explain the worse function outcomes in patients with an extended PT (the regression coefficient was changed by 28.2% and 28.1%, respectively).
Conclusions
The PT is an independent predictor for 90-day outcomes in stent-retriever thrombectomy patients. Postprocedural HT was partially responsible for the worse outcome in patients who experienced a longer PT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Mechanical thrombectomy (MT) has become the current standard of care for large vessel occlusion stroke (LVOS) of the anterior circulation [1]. Furthermore, the benefit of MT is critically time-dependent [2]. Traditionally, studies evaluating the relationship between time metrics and outcomes in patients undergoing thrombectomy have mainly focused on the time from stroke onset to door or to vessel revascularization [3, 4]. However, a breakdown of various time metrics based on the extent of impact on clinical outcomes has not been well studied.
A previous study showed that the association between the time from stroke onset to reperfusion and outcomes may be determined by the time from imaging to reperfusion [5]. However, compared with the time from imaging to puncture, the time from puncture to reperfusion or procedure time (PT) demonstrates considerable variation due to the complicated and individualized process of recanalization for MT. Moreover, these variations may directly impact clinical outcomes [6]. Previous studies have investigated the relationship between PT and clinical outcomes in patients with LVOS who underwent endovascular treatment [6,7,8]. However, these studies were based on the older-generation thrombectomy devices.
According to current guidelines, stent-retriever thrombectomy is now recommended as the first-line approach for LVOS of the anterior circulation [9]. The development of new thrombectomy approaches not only improves the speed and extent of MT recanalization but also creates a concurrent need to analyze the impact of the complex intraprocedural time metrics on outcomes. Recently, two publications reported the effect of the PT on outcomes based on modern thrombectomy techniques [10, 11] and showed that a longer PT may lead to lower rates of functional independence and higher rates of procedural complications or symptomatic intracranial hemorrhage (sICH). However, the relationship among PT, postprocedural hemorrhagic transformation (HT), and 90-day outcomes in MT patients is still unclear. Based on the previous findings, we hypothesized that postprocedural HT mediated the relationship between the PT and functional outcomes in patients undergoing stent-retriever thrombectomy. Additionally, we tried to construct the time–benefit curve of the PT and outcomes for stent-retriever thrombectomy patients.
Materials and methods
Patient selection
We retrospectively analyzed the clinical data of patients with LVOS involving the anterior circulation who underwent endovascular treatment at two comprehensive stroke centers (Jinling Hospital between January 2014 and October 2018 and Yijishan Hospital between July 2014 and December 2018). The stroke centers met the following criteria: (1) all operators were required to have performed at least 50 endovascular procedures annually, including at least 20 MT procedures with the stent retrieval devices; (2) all intervention teams were certified interventionists for intra-arterial intervention on LVOS of the anterior circulation; and (3) all operators were required to have engaged in intervention work for more than 2 years. The study was approved by the local ethics committee.
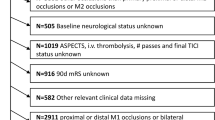
Patients were enrolled if they fulfilled the following inclusion criteria: (1) age ≥ 18 years; (2) time from stroke onset to puncture (OTP) ≤ 8 h; (3) baseline National Institutes of Health Stroke Scale (NIHSS) score ≥ 6, baseline Alberta Stroke Program Early CT (ASPECT) score ≥ 6 and pre-stroke modified Rankin Scale (mRS) score < 2; (4) the internal carotid artery (ICA) or M1 segment of the middle cerebral artery (MCA) occlusion confirmed by emergency computed tomographic angiography (CTA)/magnetic resonance angiography (MRA)/digital subtraction angiography (DSA); and (5) the initial MT was performed with stent retrievers. The flow chart of inclusion of the study population is displayed in Fig. 1.
Data collection
All clinical data were prospectively documented, which included demographics, medical history, baseline NIHSS score, baseline ASPECT score and pre-mRS score. The stroke cause was assessed using the Trial of ORG 10172 in Acute Stroke Treatment (TOAST) classification.
Procedural characteristics were evaluated by the operators, including OTP, PT, the collateral circulation score, passes of the retriever and the grade of vessel recanalization. Vessel recanalization was assessed using the modified Thrombolysis in Cerebral Infarction (mTICI) grading system. Successful recanalization was defined as a score of 2b or 3. The PT was defined as the time from puncture to first successful recanalization or to abortion of the procedure if successful recanalization was not achieved [10]. If the patients had an intraprocedural complication, the PT was defined as the time from puncture to the time when the complication was recorded [10]. Collateral circulation was assessed based on the DSA using a 3-point scale score (grade 0, little or no significant filling of the occluded territory or less than one-third of the occluded territory; grade 1, the collateral flow filled less than two-thirds of the occluded territory; and grade 2, the collateralization filled more than two-thirds of the territory or the proximal main stem) [12].
Functional outcomes were assessed using the mRS score at 90 days. A favorable outcome or functional independence was defined as a mRS score of 0–2. The HT was classified using the European Cooperative Acute Stroke Study (ECASS) definition, which is based on CT imaging obtained within 24 h of the procedure [13]. The sICH was defined as a type 2 parenchymal hematomas (PH) or as a newly observed intracranial hemorrhage with an NIHSS score that increased by more than four points.
Statistical analysis
The continuous variables were presented as the mean ± standard deviation (SD) or as the median (interquartile range, IQR), and the categorical variables were expressed as frequency (percentages). The continuous variables were compared using the Student’s t test or Mann–Whitney U test, and the categorical variables were compared using the chi-square test or Fisher’s exact test. The association between the PT and clinical outcomes was analyzed using binary logistic regression. Variables were included in the logistic models based on the statistical significance of the univariate analysis (p ≤ 0.05), with goodness of fit being assessed using the Hosmer–Lemeshow test. Regression coefficients and odds ratios (OR) with two-sided 95% confidence intervals (CI) for each of the variable included in the model were finally calculated.
Mediation analysis was performed to determine whether the HT (ECASS classifications) influences the association between the PT (continuous variable) and functional outcome (the 90-day mRS score) [14]. Mediation analysis consists of a four-step procedure [15]. The Sobel test was used to detect the statistical significance of the mediation effect.
To generate time–benefit curves, we used a logistic regression model to estimate the probability of clinical outcomes based on the PT after adjusting for age, baseline NIHSS score, baseline ASPECT score, and OTP [16]. In addition, curves representing changes in the percentages of the outcomes, passes of the retriever or sICH associated with the PT were performed by GraphPad Prism 7 (GraphPad, La Jolla, California, USA), and a best-fitting curves model was constructed. The models were evaluated using the R2 and the Runs test for model deviance from actual values [10].
For all analyses, a two-tailed value of p < 0.05 was considered significant. All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Patient baseline characteristics
A total of 283 patients (mean age, 67.2 ± 11.9 years; male, 53.7%) were included in this study. The baseline NIHSS score, baseline ASPECT score and OTP was 17 (IQR 14–20), 9 (IQR 8–10), and 256 ± 76.6 min, respectively. Successful recanalization was achieved in 227 (80.2%) patients. All enrolled patients underwent a 90-day follow-up. Of the enrolled patients, 124 (43.8%) patients achieved 90-day functional independence, 27 (9.5%) patients had an sICH, and 70 (24.7%) patients died.
Multivariate analysis of the relationship among procedure time, functional outcome, and symptomatic intracranial hemorrhage
In the univariate analysis, the PT was significantly shorter in patients with a favorable outcome than in patients with a poor outcome (66 min vs. 89 min, respectively, p < 0.001). Similarly, there was a significantly longer PT in patients with sICH than in patients without sICH (111 min vs. 75 min, respectively, p = 0.001). However, there was no significant difference in OTP between the two groups. We used logistic regression models to analyze the predictive effect of the PT for clinical outcomes. The univariate analysis and the multivariate logistic regression analyses between the PT and clinical outcomes are shown in Tables 1 and 2. After adjustment for confounding factors, the extended PT was associated with a decreased likelihood of 90-day functional independence (per 30 min: OR 1.433, 95% CI 1.062–1.865, p = 0.019) and an increased likelihood of postprocedural sICH (per 30 min: OR 1.391, 95% CI 1.030–1.865, p = 0.029).
In the subgroup analysis, we investigated the relationship between the PT and outcomes in patients with successful recanalization (n = 227). Significant variables in the univariate analysis were entered into the multivariate logistic model (Tables 3 and 4). We also found that the extended PT was associated with a decreased likelihood of 90-day functional independence (per 30 min: OR 1.522, 95% CI 1.062–2.159, p = 0.020) and an increased likelihood of postprocedural sICH (per 30 min: OR 1.716, 95% CI 1.161–2.648, p = 0.009).
Mediation analysis of the relationship among procedure time, postprocedural hemorrhagic transformation and clinical outcomes
We used the mediation analysis to explore whether postprocedural HT is partially responsible for the worse functional outcomes in patients with a longer PT. After including postprocedural HT as a mediator, we observed a significant partial mediation effect for postprocedural HT on PT-related effects on the 90-day mRS score. The regression coefficient was changed by 28.2% in the overall cohort and 28.1% in patients with successful recanalization (Fig. 2).
Each step of the analyses assessing the mediation effect of postprocedural HT on the association of the procedure time with functional outcome (A for all patients; B for patients with mTICI ≥ 2b). The coefficient and p values of the regression of each step are described. The percentage difference of the coefficients (1 − c/c′) is shown. mRS modified Rankin Scale
Curve representing changes in the percentage of clinical outcomes with procedure time
The changes in the probability of a poor outcome (90-day mRS score 3–6) and sICH associated with PT are shown in Fig. 3. We found that the predicted probabilities for a mRS score 3–6 were > 50% after 52.8 min of PT (Fig. 3A). Moreover, there was a near linear relationship between the poor outcome and the PT within 100 min. A sigmoidal curve was fitted between the rate of a good outcome and the PT (Fig. 4A, R2 = 0.741; Runs test, p = 0.788). Similarly, a significant change was observed after almost 60 min of PT. As shown in Fig. 3B, the rate of sICH gradually increased with the prolongation of the PT. The incidence of sICH with a PT of more than 119.6 min was higher than the average of this study (9.5%). Similarly, the association between the rate of sICH and the PT was fitted to an exponential growth curve (Fig. 4C, R2 = 0.847; Runs test, p = 0.853). However, the number of attempts of the stent retriever and the rate of different outcomes showed a linear relationship (Fig. 4B, R2 = 0.753; Runs test, p = 0.971).
The adjusted predicted probabilities of the association between the procedure time and a poor outcome (mRS score 3–6, A) or sICH (B). The regression curve estimates the probability of outcomes for an average patient (mean age, 67.2 years; baseline NIHSS score, 17.4; baseline ASPECT score, 8.7; OTP, 256.2 min). The gray area indicates the 95% confidence interval. ASPECT Alberta Stroke Program Early CT, mRS modified Rankin Scale, NIHSS National Institutes of Health Stroke Scale, OTP symptoms onset to groin puncture time, sICH symptomatic intracerebral hemorrhage
A, likelihood of achieving a good versus poor outcome at 90 days as a function of procedure time (R2 = 0.741; Runs test, p = 0.788); B rates of a good or poor outcome with the number of attempts (R2 = 0.753; Runs test, p = 0.971); C rates of symptomatic intracerebral hemorrhage with procedure time (R2 = 0.847; Runs test, p = 0.853)
Discussion
The major findings of this study were as follows. First, a prolonged PT was significantly associated with a lower rate of 90-day functional independence and a higher rate of sICH, even in patients with successful recanalization. Moreover, worse functional outcomes associated with the prolonged PT could be explained partially by postprocedural HT. Second, we preliminarily constructed the time–benefit curve of the PT and outcomes for stent-retriever thrombectomy patients.
Previously, several studies have investigated the relationship between the PT and clinical outcomes in endovascular treatment [6,7,8]. However, the conclusions were based on the older-generation thrombectomy devices. Recently, Alawieh et al. showed that in a direct aspiration at first pass technique (ADAPT) thrombectomy procedures, extended PT may reduce the likelihood of a good outcome [17]. Considering the considerable difference in PT between different thrombectomy devices, the present study further explored the relationship between the PT and functional outcomes in stent-retriever-based thrombectomy. Our data showed that the PT was an important predictor of 90-day functional outcomes. These findings corroborated the results of recent studies [10, 11], and added to the evidence underscoring the benefits of achieving recanalization rapidly in thrombectomy.
Postprocedural HT is a common complication after MT. A previous study showed that extending PT beyond 60 min may increase intraprocedural complications [8]. Moreover, Kass-Hout et al. suggested that a longer PT is an independent predictor for sICH in patients receiving MT [7]. In the study, we further highlighted the effect of extended PT on sICH in patients undergoing stent-retriever thrombectomy and confirmed that worse outcomes associated with prolonged PT may be related to postprocedural HT. To the best of our knowledge, this is the first study to assess the mediation effect of postprocedural HT on functional outcomes based on the PT in thrombectomy patients.
Several mechanisms could explain the results. First, the prolonged PT may be related to difficult catheter access, which may be related to older age or more comorbidities [18]. These factors could increase the risk of HT after endovascular therapy [19]. Second, for stent-retriever MT, the longer PT represents more attempts or rescue treatments to achieve recanalization, which may result in an increased risk of intraprocedural and procedural complications [20]. Third, the longer PT may lead to the progression of ischemia, which may diminish the benefits of recanalization and increase the risk for HT [19]. In this study, even in patients with successful recanalization, prolonged PT significantly affected the prognosis. Therefore, the impact of the PT on prognosis is not limited to ‘time delay’ itself, but is multifactorial.
Establishing a standardized intraprocedural time metric for MT will likely help to improve clinical outcomes and assist in refining the application of endovascular thrombectomy [21, 22]. In this study, we found that the probability of 90-day functional independence was less than 50% after a PT of more than 52.8 min. Moreover, the probability of a 90-day poor outcome had a steep increase within the first 100 min after the procedures. According to these findings, we suggested that the ‘golden 60’ may serve as the first metric for MT using the stent retriever. In addition, our data demonstrated that postprocedural HT is an important mediator of the prognosis in prolonged PT patients. This finding is important because it provides a potential warning to the operators. The result of our study showed that after more than 119.6 min of PT, the rate of sICH would be higher than the average from the current study. Therefore, the ‘warning 120’ may serve as the second metric for MT using the stent retriever. The metric could assist the operators in determining whether the procedure should continue, especially for a prolonged PT in patients with a high HT risk. Although these results were consistent with the findings reported in previous studies [8, 23], they still need to be validated in other large cohorts.
A Korean study demonstrated that the number of attempts may be a surrogate for PT [23]. However, the breaking point of the number of attempts was significantly different in different studies [19, 23, 24]. Furthermore, a recent study showed that the PT remained a significant predictor even if the number of attempts was included as a variable [10]. We speculated that the difficult anatomy and various types of rescue therapy may affect the relationship among the number of attempts, the PT, and functional outcomes. Further analyses centered on this question should be performed in the future to individualize treatment strategies and determine the best approach to achieving rapid recanalization in each patient.
Notably, these cutoff points were determined by constructing a time–benefit curve, which did not represent an optimal intraprocedural time metric for stent-retriever thrombectomy. Every procedure needs to be considered individually. Moreover, the process of successful recanalization is variable. Thus, we considered that the metrics are doubly important in the setting of the procedure. First, the ‘golden 60’ can help establish standardized procedural protocols, which could help the operators choose the best approaches based on patient- and treatment-related factors to achieve recanalization as soon as possible. Second, for patients whose PT has exceeded the ‘warning 120’, the operators would need to reassess the risks and benefits of continuing the procedure.
This study has several limitations. First, our study was a retrospective, medium sample-size study. A multicenter prospective study will be required to confirm our results. Second, this study did not include all outcome-related variables for mediation analysis, such as infarct volume. Thus, selection biases might have occurred. Third, we did not further analyze the relevant factors affecting PT, due to the retrospective nature of the data. In addition, since this study enrolled only patients in which stent retriever devices were used as first pass, the results could not be extended to patients with other thrombectomy techniques [17]. However, our study provided additional support for the time metric in MT patients using the stent-retriever. Furthermore, to the best of our knowledge, this study was the first to assess the mediation effect of postprocedural HT on functional outcomes based on the PT in MT patients using the stent retriever.
Conclusion
Our data indicated that a longer PT is an independent risk factor for poor 90-day outcomes in patients undergoing stent-retriever thrombectomy. Postprocedural HT was partially responsible for a worse mRS score at 90 days in patients with a prolonged PT. Our findings provided novel information to help improve the process and the determination of procedural decisions for stent-retriever thrombectomy.
References
Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, Davalos A, Majoie CB, van der Lugt A, de Miquel MA, Donnan GA, Roos YB, Bonafe A, Jahan R, Diener HC, van den Berg LA, Levy EI, Berkhemer OA, Pereira VM, Rempel J, Millan M, Davis SM, Roy D, Thornton J, Roman LS, Ribo M, Beumer D, Stouch B, Brown S, Campbell BC, van Oostenbrugge RJ, Saver JL, Hill MD, Jovin TG, Collaborators H (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 387:1723–1731
Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, Campbell BC, Nogueira RG, Demchuk AM, Tomasello A, Cardona P, Devlin TG, Frei DF, du Mesnil de Rochemont R, Berkhemer OA, Jovin TG, Siddiqui AH, van Zwam WH, Davis SM, Castano C, Sapkota BL, Fransen PS, Molina C, van Oostenbrugge RJ, Chamorro A, Lingsma H, Silver FL, Donnan GA, Shuaib A, Brown S, Stouch B, Mitchell PJ, Davalos A, Roos YB, Hill MD, Collaborators H (2016) Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA 316:1279–1288
Khatri P, Yeatts SD, Mazighi M, Broderick JP, Liebeskind DS, Demchuk AM, Amarenco P, Carrozzella J, Spilker J, Foster LD, Goyal M, Hill MD, Palesch YY, Jauch EC, Haley EC, Vagal A, Tomsick TA, Trialists II (2014) Time to angiographic reperfusion and clinical outcome after acute ischaemic stroke: an analysis of data from the Interventional Management of Stroke (IMS III) phase 3 trial. Lancet Neurol 13:567–574
Nogueira RG, Smith WS, Sung G, Duckwiler G, Walker G, Roberts R, Saver JL, Liebeskind DS, MERCI, Multi MWC (2011) Effect of time to reperfusion on clinical outcome of anterior circulation strokes treated with thrombectomy: pooled analysis of the MERCI and multi MERCI trials. Stroke 42:3144–3149
Ribo M, Molina CA, Cobo E, Cerda N, Tomasello A, Quesada H, De Miquel MA, Millan M, Castano C, Urra X, Sanroman L, Davalos A, Jovin T, Investigators RT (2016) Association between time to reperfusion and outcome is primarily driven by the time from imaging to reperfusion. Stroke 47:999–1004
Hassan AE, Chaudhry SA, Miley JT, Khatri R, Hassan SA, Suri MF, Qureshi AI (2013) Microcatheter to recanalization (procedure time) predicts outcomes in endovascular treatment in patients with acute ischemic stroke: when do we stop? AJNR Am J Neuroradiol 34:354–359
Kass-Hout T, Kass-Hout O, Sun CJ, Kass-Hout TA, Nogueira R, Gupta R (2016) Longer procedural times are independently associated with symptomatic intracranial hemorrhage in patients with large vessel occlusion stroke undergoing thrombectomy. J Neurointerventional Surg 8:1217–1220
Spiotta AM, Vargas J, Turner R, Chaudry MI, Battenhouse H, Turk AS (2014) The golden hour of stroke intervention: effect of thrombectomy procedural time in acute ischemic stroke on outcome. J Neurointerventional Surg 6:511–516
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, Jauch EC, Kidwell CS, Leslie-Mazwi TM, Ovbiagele B, Scott PA, Sheth KN, Southerland AM, Summers DV, Tirschwell DL (2018) 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 49:e46–e110
Alawieh A, Vargas J, Fargen KM, Langley EF, Starke RM, De Leacy R, Chatterjee R, Rai A, Dumont T, Kan P, McCarthy D, Nascimento FA, Singh J, Vilella L, Turk A, Spiotta AM (2019) Impact of procedure time on outcomes of thrombectomy for stroke. J Am Coll Cardiol 73:879–890
Hassan AE, Shariff U, Saver JL, Goyal M, Liebeskind D, Jahan R, Qureshi AI (2019) Impact of procedural time on clinical and angiographic outcomes in patients with acute ischemic stroke receiving endovascular treatment. J Neurointerventional Surg. https://doi.org/10.1136/neurintsurg-2018-014576
Christoforidis GA, Mohammad Y, Kehagias D, Avutu B, Slivka AP (2005) Angiographic assessment of pial collaterals as a prognostic indicator following intra-arterial thrombolysis for acute ischemic stroke. AJNR Am J Neuroradiol 26:1789–1797
Yaghi S, Willey JZ, Cucchiara B, Goldstein JN, Gonzales NR, Khatri P, Kim LJ, Mayer SA, Sheth KN, Schwamm LH (2017) Treatment and outcome of hemorrhagic transformation after intravenous alteplase in acute ischemic stroke: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 48:e343–e361
Baron RM, Kenny DA (1986) The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 51:1173–1182
Kimberly WT, Dutra BG, Boers AMM, Alves H, Berkhemer OA, van den Berg L, Sheth KN, Roos Y, van der Lugt A, Beenen LFM, Dippel DWJ, van Zwam WH, van Oostenbrugge RJ, Lingsma HF, Marquering H, Majoie C, Investigators MC (2018) Association of reperfusion with brain EDEMA in patients with acute ischemic stroke: a secondary analysis of the MR CLEAN trial. JAMA Neurol 75:453–461
Kim J-T, Fonarow GC, Smith EE, Reeves MJ, Navalkele DD, Grotta JC, Grau-Sepulveda MV, Hernandez AF, Peterson ED, Schwamm LH, Saver JL (2017) Treatment With tissue plasminogen activator in the golden hour and the shape of the 4.5-hour time-benefit curve in the National United States get with the guidelines-stroke population. Circulation 135:128–139
Alawieh A, Pierce AK, Vargas J, Turk AS, Turner RD, Chandry MI, Spiotta AM (2018) The golden 35 min of stroke intervention with ADAPT: effect of thrombectomy procedural time in acute ischemic stroke on outcome. J Neurointerventional Surg 10:213–220
Ribo M, Flores A, Rubiera M, Pagola J, Mendonca N, Rodriguez-Luna D, Pineiro S, Meler P, Alvarez-Sabin J, Molina CA (2013) Difficult catheter access to the occluded vessel during endovascular treatment of acute ischemic stroke is associated with worse clinical outcome. J Neurointerventional Surg 5(Suppl 1):i70–i73
Hao Y, Yang D, Wang H, Zi W, Zhang M, Geng Y, Zhou Z, Wang W, Xu H, Tian X, Lv P, Liu Y, Xiong Y, Liu X, Xu G, for the ACTUAL (Endovascular Treatment for Acute Anterior Circulation Ischemic Stroke Registry) Investigators (2017) Predictors for symptomatic intracranial hemorrhage after endovascular treatment of acute ischemic stroke. Stroke 48:1203–1209
Bourcier R, Saleme S, Labreuche J, Mazighi M, Fahed R, Blanc R, Gory B, Kyheng M, Marnat G, Bracard S, Desal H, Consoli A, Piotin M, Lapergue B (2018) More than three passes of stent retriever is an independent predictor of parenchymal hematoma in acute ischemic stroke. J Neurointerventional Surg. https://doi.org/10.1136/neurintsurg-2018-014380
Sun CH, Nogueira RG, Glenn BA, Connelly K, Zimmermann S, Anda K, Camp D, Frankel MR, Belagaje SR, Anderson AM, Isakov AP, Gupta R (2013) "Picture to puncture": a novel time metric to enhance outcomes in patients transferred for endovascular reperfusion in acute ischemic stroke. Circulation 127:1139–1148
Gonzalez NR (2019) Endovascular thrombectomy procedure time and other predictors of futility in acute ischemic stroke interventions. J Am Coll Cardiol 73:891–892
Baek JH, Kim BM, Heo JH, Nam HS, Kim YD, Park H, Bang OY, Yoo J, Kim DJ, Jeon P, Baik SK, Suh SH, Lee KY, Kwak HS, Roh HG, Lee YJ, Kim SH, Ryu CW, Ihn YK, Kim B, Jeon HJ, Kim JW, Byun JS, Suh S, Park JJ, Lee WJ, Roh J, Shin BS (2018) Number of stent retriever passes associated with futile recanalization in acute stroke. Stroke 49:2088–2095
Bai Y, Pu J, Wang H, Yang D, Hao Y, Xu H, Zhang M, Geng Y, Wan Y, Wang W, Zhang H, Zi W, Liu X, Xu G, for the ACTUAL (Endovascular Treatment for Acute Anterior Circulation Ischemic Stroke Registry) Investigators (2018) Impact of retriever passes on efficacy and safety outcomes of acute ischemic stroke treated with mechanical thrombectomy. Cardiovasc Interv Radiol 41:1909–1916
Funding
This work was supported by the National Natural Science Foundation of China (nos. 81870946, 81771424, 81530038), Natural Science Foundation of Jiangsu Province (no. BE2016748), and National Key Research and Development Program (no. 2017YFC1307901).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
There are no conflicts among the authors. All authors read and approved the final submission of the manuscript.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Huang, X., Cai, Q., Xiao, L. et al. Influence of procedure time on outcome and hemorrhagic transformation in stroke patients undergoing thrombectomy. J Neurol 266, 2560–2570 (2019). https://doi.org/10.1007/s00415-019-09451-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09451-5